Translate this page into:
Sonographic detection of abdominal pathologies in human immunodeficiency virus/acquired immunodeficiency syndrome patients and its correlation with CD4 counts – A prospective analysis
*Corresponding author: Tejas Kanthrao Mankeshwar, Department of Radiodiagnosis and Imaging, B.J. Medical College and Sassoon General Hospitals, Pune, Maharashtra, India. tejasm2008@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Mankeshwar TK, Sharma AK. Sonographic detection of abdominal pathologies in human immunodeficiency virus/ acquired immunodeficiency syndrome patients and its correlation with CD4 counts – A prospective analysis. Indian J Med Sci 2021;73:297-304.
Abstract
Objectives:
Abdominal pathologies are the second most common after pulmonary diseases in human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS) patients. Ultrasonography (USG) is a vital imaging technique for the evaluation of abdominal pathologies. This study was aimed at evaluating the abdominal pathologies using USG in HIV/AIDS and further analysis of its correlation with CD4 count.
Material and Methods:
The present study was carried out on 392 HIV-positive patients with abnormal abdominal sonographic findings. All data were analyzed by Chi-square test and one-way analysis of variance using SPSS 16.0 software.
Results:
Of these 392 patients, 66.3% were males, the mean age was 35.7 years, (range 7–64 years) and most of them were in 4th decade. On ultrasonographic evaluation, spleen was involved in 45.2% patients and liver as well as lymph nodes each was involved in 43.6% patients. Other cases displayed ascites and bowel thickening in 5.3% and 3.8% patients, respectively. Less involvement of kidney (2.3%), pancreas (1.5%), and biliary system (1.3%) was observed. In addition, pathologies such as hepatomegaly, splenomegaly, splenic microabscess, focal pancreatic lesion, mesenteric, and periportal lymphadenopathy showed significant correlation with CD4 counts. Lymphoma was found in 1% of patients, involving liver, pancreas, and retroperitoneal lymph nodes.
Conclusion:
Our study highlights the clinical utility of abdominal USG in HIV/AIDS patients. CD4 counts largely affect the differential diagnosis in HIV/AIDS patients. USG findings interpreted in the context of CD4 count may help in guiding the exact diagnosis.
Keywords
CD4 count
Human immunodeficiency virus/acquired immunodeficiency syndrome
Lymphoma
Splenic microabscess
Ultrasonography
INTRODUCTION
Human immunodeficiency virus (HIV) is a retrovirus that infects CD4 cells and disrupts their function. In the last decade, there has been an unprecedented increase in the number of immunocompromised patients globally. UNAIDS and WHO estimated that 35–38 million individuals lived with HIV in 2019 globally, 90% of which were from developing countries.[1]
HIV/acquired immunodeficiency syndrome (AIDS) is frequently associated with Koch’s and other viral, fungal, mycobacterial, and protozoal infections. The degree of immunodeficiency observed is related to CD4 levels and is a good index for monitoring disease progression.[2] As the immune status of a patient decreases, susceptibility to infection and consequently abnormal sonographic findings are expected to increase.[2-4]
Therefore, the current study was aimed to evaluate the effectiveness of ultrasonography (USG) for the detection of abdominal pathologies, and the changes to the HIV disease progression in infected individuals. Since CD4 levels affect abdominal pathologies and their progression, we also analyzed correlations between abnormalities detected through USG and levels of CD4 cells.
MATERIAL AND METHODS
Subject enrolment
A total of 1003 HIV patients that tested positive for the disease through ELISA were identified between December of 2013 and June of 2015 in the Department of Radiodiagnosis, BJGMC & SGH, Pune. Abdominal sonography results were indicated by the presence of abdominal pain, abnormal liver and/or kidney functioning, weight loss, vomiting, diarrhea, fever, and sepsis. Of these, 392 patients that tested positive for the presence of abnormal abdominal findings through USG were included in our study, irrespective of their age. Exclusion criteria for the study were as follows: Patients who were not HIV positive, patients that did not provide consent, and patients that did not have positive abdominal findings on USG. Informed consent for voluntary participation in the study was obtained from all participants. In the current study, we performed FNAC and/or biopsy in patients, when they did not respond to antituberculosis/antibacterial treatment and/or were highly suspicious of malignancy.
Imaging technique and interpretation
In the present study, real-time USG was performed using a Philips HD11 XE Ultrasound Machine and GE Healthcare LOGIQ 3 Ultrasound Machine. Convex abdominal probe was used to evaluate deeper structures, linear probes for superficial structures, and transvaginal probes for female pelvic evaluation. Initially, the size, echotexture, and focal lesions of the liver of each study participant were evaluated. Hepatomegaly was considered to be present when the longitudinal dimension at the mid clavicular line was more than 15 cm. A comparison of the echogenicity of the liver to the kidney/spleen was also performed. Later, the size of the portal vein and hepatic veins, and their patency and flow color were determined. Common bile duct (CBD) and intrahepatic biliary radicles were considered dilated when they measured more than 7 mm and 2 mm, respectively. The right, sub-costal, and oblique section of the gall bladder (GB) were evaluated and a GB wall of more than 3 mm was considered thickened. The presence of gall stones, if any, was recorded.
The pancreas, inferior vena cava, aorta, and its branches were evaluated throughout the epigastric region. The pancreas was considered bulky if the anteroposterior diameter of its head was greater than 3 cm, its body was greater than 2 cm, and its tail was greater than 2.5 cm. The pancreatic duct (PD) was considered dilated if it was greater than 2 mm. Any calcifications within the PD and pancreatic parenchyma were recorded.
The size, presence of focal lesions, cortical echogenicity, and renomegaly, which occurred when kidneys were greater than 12 cm of both kidneys were evaluated. Renal echogenicity was considered to be increased if it was more than the echogenicity of the liver or spleen. Retroperitoneum and abdominal lymph nodes were evaluated and considered to be enlarged if their diameters were greater than 1 cm. Echotexture and hilum of lymph nodes were also recorded.
The spleen of each individual was measured and the presence of focal lesions was evaluated. Splenomegaly was indicated when the length of the spleen was more than 12 cm. The transducer was placed in the right and left iliac fossa to evaluate the appendix, ilium, caecum, sigmoid colon, rectum, anus, and free fluid within the abdominal cavity. Thickened bowel wall was considered when it was more than 4 mm. By placing the transducer in a supra-pubic location, the urinary bladder, prostate, uterus, and adnexa were evaluated.
CD4 classification
Patients were classified based on CD4 cells levels. Patients with CD4 counts ≥ 500, between 499 and 200 cells/mm3, and <200 cells/mm3 were placed in Class-I (Non-significant), Class-II (Mild to Advanced), and Class-III (Sever), respectively.[3,5]
Statistical analysis
The Chi-square test and one-way analysis of variance were performed to analyze correlations between CD4 counts and pathologies. Data have been presented as mean values and as percentages. The level of significance was set at P < 0.05.
RESULTS
For the 392 individuals studied, the mean age of the group was 35.7 ± 10.9 y (min = 7 years, max = 64 years) and the majority (35.2%) of patients were 31–40 years. Further, 66.3% of the patients assessed were males and 33.7% were females, producing a male to female ratio of 1.9:1.
In the current study, 23.2% of the patients assessed had a CD4 count ≥500 cells/mm3 (Class I), 52.6% patients had CD4 count of 200–499 cells/mm3 (Class II), and 24.2% patients had a CD4 count <200 cells/mm3 (Class III). We observed that hepatomegaly, splenomegaly, splenic microabscess, focal pancreatic lesions, mesenteric lymph node, and periportal lymph node characteristics of patients within each of these classes significantly differed. Abnormalities were consistently observed in patients with CD4 counts <500 cell/mm3, and their occurrence further increased in patients with CD4 counts <200 cells/mm3. In contrast, the presence of focal liver lesions, dilated CBD and PD, bowel wall thickening, ascites, renomegaly as well as renal focal lesions was most common in patients with CD4 levels <500 cells/mm3. However, these findings were not significant different among the CD4 classes considered.
Sonographic findings
Among cases with positive abdominal sonographic findings, 60.2% of patients showed that a single system was affected, while 39.8% had multisystem involvement. Of this population, the abdominal USG revealed involvement of spleen in 45.2% of cases, liver and lymphadenopathy in 43.6% of cases, followed by ascites in 5.3%, bowel in 3.8%, kidney in 2.3%, and biliary and pancreatic organs in 1.3% of cases. The least (0.8%) commonly involved organs were the uterus and adnexa [Table 1]. Out of these cases, 4 (1%) patients had malignancy (lymphoma), while the others had infections. Among the patients with lymphoma, one patient had a hypoechoic lesion in the liver and pancreas, one had a hypoechoic lesion in the pancreas only, and the other had involved retroperitoneal lymph nodes.
| Systems involved | No. of cases | % of cases (prevalence) |
|---|---|---|
| Hepatic | 171 | 43.6 |
| Biliary | 5 | 1.3 |
| Splenic | 177 | 45.2 |
| Kidney | 9 | 2.3 |
| Pancreas | 5 | 1.3 |
| Bowel involvement | 15 | 3.8 |
| Ascites | 21 | 5.3 |
| Lymphadenopathy | 171 | 43.6 |
| Uterus and Adnexa | 1 | 0.8 |
Data are presented as percentages
Hepatobiliary system
Hepatomegaly was detected in 40.3% of the patients assessed and it was the most commonly observed abnormality of the 31–40 years age group. Hepatomegaly was noted in 42.9%, 44.2%, and 29.5% of the patients within Class I, Class II, and Class III, respectively. The prevalence of hepatomegaly differed significantly across the three classes (P < 0.046) and it was most common in patients with CD4 counts > 200 cells/ mm3. Raised echogenicity of the liver was identified in 13% patients and an altered echotexture of liver was observed 6% of patients assessed [Tables 1-3 and Figure 1a].
| USG findings | No. of cases | % of cases (prevalence) |
|---|---|---|
| Hepatomegaly | 158 | 40.3 |
| Focal liver lesion | 16 | 4.1 |
| Portal vein | 2 | 0.6 |
| Dilated CBD | 5 | 1.3 |
| Splenomegaly | 148 | 37.8 |
| Splenic microabscess | 85 | 21.7 |
| Renomegaly | 8 | 2.0 |
| Renal focal lesions | 1 | 0.3 |
| Dilated PD | 4 | 1.0 |
| Focal pancreatic lesion | 2 | 0.5 |
| Bowel wall thickening | 15 | 3.8 |
| Ascites | 21 | 5.4 |
| Retroperitoneal LN | 90 | 22.9 |
| Mesenteric LN | 79 | 20.2 |
| Periportal LN | 60 | 15.3 |
| Uterus and Adnexa | 1 | 0.8 |
CBD: Common bile duct, PD: Pancreatic duct, LN: Lymph nodes. Data are presented as percentages
| USG findings | Class I (n=91) | Class II (n=206) | Class III (n=95) | P-value | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Hepatomegaly | 39 | 42.9 | 91 | 44.2 | 28 | 29.5 | 0.046* |
| Focal liver lesion | 0 | 0.0 | 12 | 5.8 | 4 | 4.2 | 0.065NS |
| Portal vein | 0 | 0.0 | 1 | 0.5 | 1 | 1.1 | 0.401NS |
| Dilated CBD | 1 | 1.1 | 1 | 0.5 | 3 | 3.2 | 0.156NS |
| Splenomegaly | 32 | 35.2 | 69 | 33.5 | 47 | 49.5 | 0.025* |
| Splenic microabscess | 2 | 2.2 | 40 | 19.4 | 43 | 45.3 | 0.001*** |
| Renomegaly | 3 | 3.3 | 5 | 2.4 | 0 | 0.0 | 0.240NS |
| Renal focal lesions | 0 | 0.0 | 0 | 0.0 | 1 | 1.1 | 0.209NS |
| Dilated P.D. | 0 | 0.0 | 3 | 1.5 | 1 | 1.1 | 0.515NS |
| Focal pancreatic lesion | 0 | 0.0 | 0 | 0.0 | 2 | 2.1 | 0.043* |
| Bowel wall thickening | 1 | 1.1 | 8 | 3.9 | 6 | 6.3 | 0.179NS |
| Ascites | 2 | 2.2 | 12 | 5.8 | 7 | 7.4 | 0.267NS |
| Retroperitoneal LN | 20 | 22.0 | 38 | 18.4 | 32 | 33.6 | 0.077NS |
| Mesenteric LN | 12 | 13.2 | 36 | 17.5 | 31 | 32.6 | 0.002** |
| Periportal LN | 9 | 9.9 | 25 | 12.1 | 26 | 27.4 | 0.001*** |
| Uterus and Adnexa | 0 | 0.0 | 1 | 1.4 | 0 | 0.0 | 0.607NS |
CBD: Common bile duct, PD: Pancreatic duct, LN: Lymph nodes. Data are presented as mean valves and percentages. P-values by Chi-square test. P<0.05 is considered to be statistically significant. *P<0.05, **P<0.01, ***P<0.001, NS: Statistically non-significant
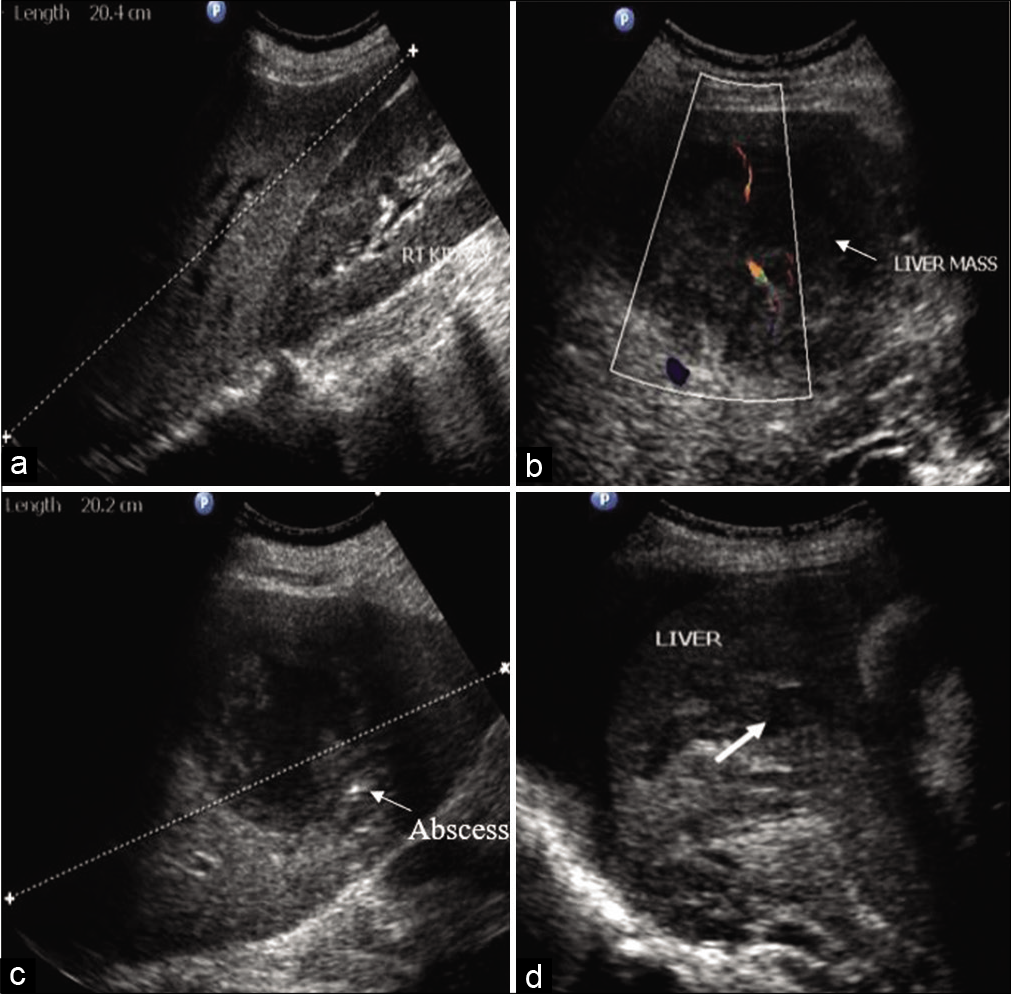
- (a) Hepatomegaly. (b) Well-defined hypoechoic solid mass lesion (arrow) in liver with in a patient of lymphoma. (c) Ill-defined hypoechoic liver abscess (arrow) with central necrotic area and shaggy walls. (d) Target focal lesion (arrow) in a patient of candida infection of liver.
Focal hypoechoic lesions of the liver were identified in 4.1% of patients assessed. Of the hypoechoic lesions identified, hepatic abscesses were observed in 3.8% of patients considered and one patient with lymphoma had multiple, solid mass lesions in liver. One case had multiple hypoechoic lesions in the hepatic parenchyma with associated thrombosis of the portal vein, which, on biopsy, was determined to be caused by candida infection. No significant correlation between hepatic focal lesions and CD4 counts was determined (P < 0.065); however, the lesions were commonly observed in Class II and Class III groups [Tables 2 and 3; Figure 1b-d].
Biliary tract abnormalities were seen in 1.3% of cases considered, and all of these had dilated CBD, which did not significantly correlate with CD4 counts. One case involved a patient with a dilated CBD that was associated with dilated intrahepatic biliary radicles. Other four cases had isolated dilated CBD and did not have intrahepatic biliary radicles dilatation. GB calculi were noted in 1.5% of cases and were not associated with cholecystitis [Tables 1 and 3].
Spleen
Splenomegaly or focal hypoechoic lesions were noted in 45.3% of patients. Splenomegaly was observed in 37.8% patients. Splenomegaly was noted in 35.2%, 33.5%, and 49.5% of patients of Class I, Class II, and Class III groups, respectively. The prevalence of splenomegaly significantly differed between groups (P < 0.025) and was most common in patients with CD4 counts <200 cells/mm3. A significant (P < 0.001) number of patients within Class II and Class III groups (19.4% and 45.3%, respectively) had multiple focal hypoechoic splenic microabscesses relative to patients of Class I [Tables 1-3; Figure 2a and b].
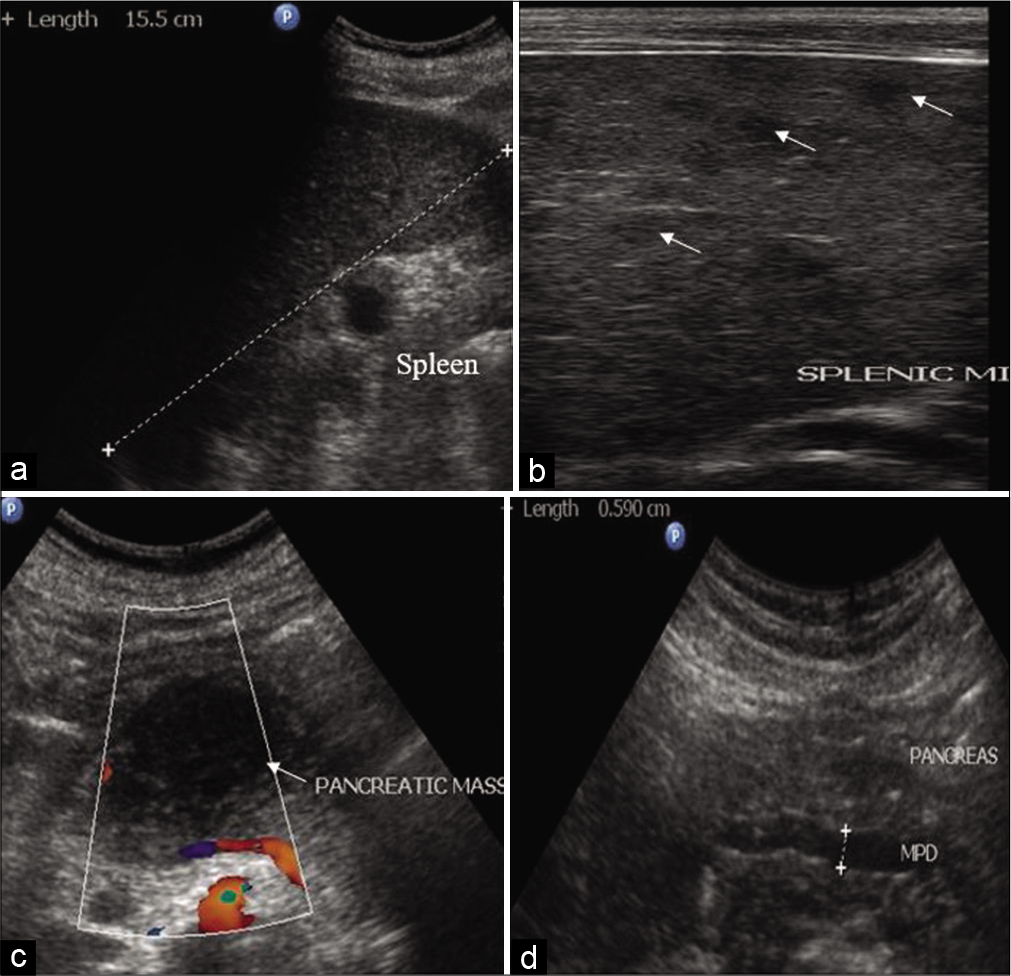
- (a) Splenomegaly. (b) Multiple ill-defined, focal, hypoechoic (arrow) splenic micro abscesses. (c) Well-defined hypoechoic solid mass lesion (arrow) in body pancreas in a patient of lymphoma. (d) Dilated main pancreatic duct in a patient of chronic pancreatitis.
Pancreas
Pancreatic abnormalities were noted in 1.5% cases. These patients were diagnosed as chronic pancreatitis with dilated PD, without significant CD4 counts correlation. Focal hypoechoic lesion within the body of pancreas was seen in two (0.5%) patients and had significant (P < 0.043) correlation with CD4 count <200 cells [Tables 2 and 3; Figure 2c and d].
Lymph node
Abdominal lymphadenopathy was found in 43.6% of the patients examined and was also a commonly observed abnormal USG finding. The retroperitoneal region was most commonly involved region investigated (22.9%), and other areas examined were the pre/para aortic, aortocaval, peripancreatic, and coeliac lymph nodes. The other enlarged lymph nodes identified were mesenteric (20.2%) and periportal (15.3%) nodes. Many of the enlarged lymph nodes identified had areas of necrosis that presented as hypoechoic echotexture with the loss of central fatty hilum. The occurrence of retroperitoneal lymphadenopathy was not significantly different in various CD4 count classes (P < 0.077). However, the prevalence abnormalities associated with mesenteric and periportal lymph nodes were significantly increased in patients with CD4 levels <200 cells/mm3 (P < 0.002 and P < 0.001) [Tables 2 and 3; Figure 3a and b].
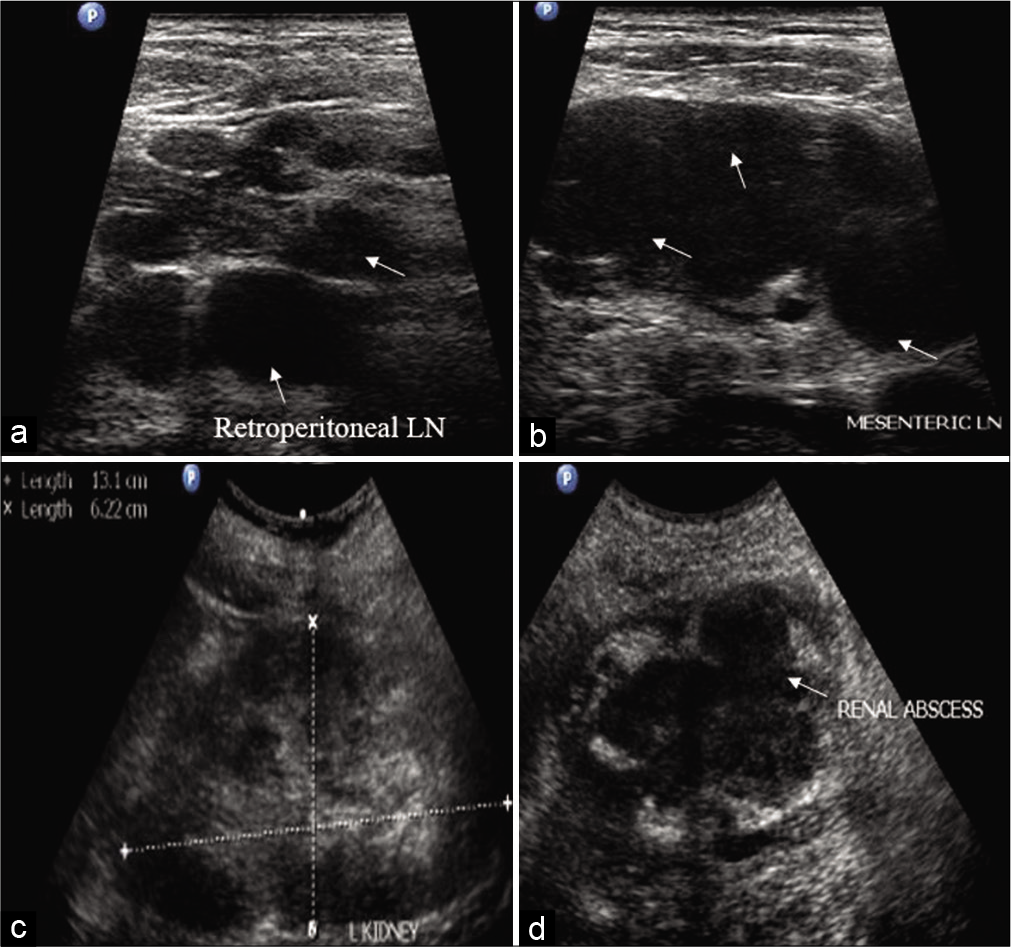
- (a) Enlarged, hypoechoic (arrow), retroperitoneal lymph nodes. (b) Matted mesenteric lymphadenopathy (arrow) in abdominal tuberculosis. (c) Renomegaly with poor corticomedullary differentiation in a patient of pyelonephritis. (d) Ill-defined, hypoechoic, cystic lesion with internal echoes (arrow) in a patient of renal abscess.
Kidney
Raised renal cortical and medullary echogenicity were observed in 9.1% patients with normal sized as well as enlarged kidneys. Renal abnormalities were observed in 2.2% patients assessed. Of these, 2% had renomegaly that did not significantly correlate with CD4 levels (P < 0.24). One patient had a focal hypoechoic lesion that involved mid pole of kidney, which turned out to be a renal abscess, and rest of the patients were diagnosed with pyelonephritis [Tables 2 and 3; Figure 3c and d].
Other systems
In addition, bowel wall thickening was observed in 3.8% of patients examined. Involvement of caecum was the cause of the abnormality identified in all the cases of bowel wall thickening. In our study, the bowel wall thickening was found to be a result of tuberculosis in all cases. Two of these cases were associated with ileal thickening and bowel mass formation. Ascites was seen in 21 (5.4%) cases without internal echoes and septations. One female patient showed changes of the hydrosalpinx. These abnormalities did not significantly correlate with CD4 levels [Tables 2 and 3; Figure 4a-d].
DISCUSSION
HIV/AIDS is a universal pandemic. India is experiencing the third-largest HIV epidemic globally, and approximately 2.1 million people live with HIV, producing a prevalence of approximately 0.3%.[1] Cases of AIDS are rising at a tremendous rate within the Indian population and, correspondingly, so are the various spectra of abnormalities involving various organs. Our study assessed an array of sonographic abnormalities that appear within the abdomens of HIV/AIDS patients. The study revealed that hepatomegaly, splenomegaly, splenic microabscess, the presence focal pancreatic lesions, mesenteric lymphadenopathies, and periportal lymphadenopathies were significantly associated with CD4 counts. This indicates that there is direct association between immunosuppression and the ultrasonographic findings. However, the other sonographic abnormalities did not significantly correlate with levels of CD4 cells.

- (a) Concentric, cecal wall thickening (arrow) in a patient of abdominal tuberculosis. (b) Bowel mass showing ileocecal wall thickening (arrow) in a patient of abdominal tuberculosis. (c) Clear free fluid in the abdomen suggestive of ascites. (d) Dilated, tubular, anechoic hydrosalpinx (arrow) with incomplete septations in the right adnexa.
HIV infection leads to the deterioration of the host immune system and causes a wide spectrum of abdominal pathologies. CD4 count is major indicator of host immunity and CD4 counts below 500 cells/mm3 were shown to increase the likelihood of developing abdominal infections as well as neoplasms. Further decrease in CD4 counts to levels below 200 cells/mm3 enhances these pathologies and is defined clinically as AIDS. In the present study, most of the patients assessed had CD4 levels between 200 and 499 cells/mm3. Previously, Bhabhor et al.[3] and Blessing et al.[5] classified patients into various groups based on their CD4 levels. In contrast to our study, these authors reported that the majority of patients assessed had CD4 levels that were less than 200 cells/mm3.
We observed abdominal abnormalities predominately in male patients, and the male to female ratio was 1.9:1. Similarly, Bhabhor et al.[3] and Mustafa et al.[6] reported that the abnormalities were most likely to be observed in males. However, Blessing et al.[5] and Obajimi et al.[7] identified more female patients with abdominal abnormalities. Our findings are well correlated with the previous studies, who reported the mean age of HIV patients to be 35–40 years.[3,7,8]
The increased proportion of patients in their fourth decade, or between 31 and 40 years, may be due to increased sexual activity during this period. In current study, splenomegalies and splenic microabscesses were observed in a large number of patients. These were commonly seen in HIV patients with CD4 counts <200 cell/mm3 and significantly correlated with CD4 levels. Thus, our findings are in accordance with those reported in various previous studies.[3,5,7,9,10] Splenomegaly in HIV patients in the absence of splenic focal lesions may suggest septicemia, malaria, typhoid, schistosomiasis, portal hypertension and/ or hemolytic anemia. Parallel to Bhabhor et al.,[3] tuberculosis remains the most common cause of splenic microabscesses in current study, frequently affecting HIV patients with CD4 count less than 200 cell/mm3. The great number of patients with splenic microabscesses, in our study, might be due to the increased prevalence of tuberculosis in India.[3,5,7,9]
Hepatomegaly is also a common finding in patients with HIV/AIDS and may be attributed to either a non-specific response to infection, fatty infiltration, hepatic viruses, granulomatous infection, drug hepatotoxicity, or malignancy.[4-6] Hepatomegaly was the most commonly observed abnormalities detected in our study, and the condition significantly associated with CD4 levels. Accordingly, hepatomegaly was reported in multiple previous studies, though they did not report a correlation between hepatomegaly and CD4 count.[3,4-6,11] Similar to Bhabhor et al.,[3] we observed a small number of patients with increased echogenicity and altered echotexture of liver. The diffuse hyperechoic hepatic sonographic pattern observed in HIV-positive patients may be caused by either fatty infiltration or hepatic granulomatosis. USG is useful for differentiating between infectious and non-infectious focal lesions noninvasively in the liver. In our study, focal hypoechoic liver lesions were diagnosed as abscesses in almost all patients, with the exception of one patient in which it was diagnosed as lymphoma. In accordance with these results, Bhabhor et al.[3] and Pawar et al.[4] reported focal hypoechoic liver lesions that did not significantly correlate with CD4 counts. Various fungal infections have been shown to involve the liver in AIDS patients.[11] We identified one patient with CD4 counts less than 200 cells/mm3 with hypoechoic liver lesions that were attributable to candida infection.
Bile duct dilatation in HIV patients is mostly caused by acalculous inflammation of the biliary tract. In accordance with the previous reports by Bhabhor et al.[3] and Pawar et al.,[4] we observed GB wall thickening and gall stones in HIV patients, though the numbers identified in this study were lower than those of previous reports. No significant correlation between GB wall thickening and gall stones and CD4 counts was observed. Similarly, Obajimi et al.[7] and Blessing et al.[5] reported dilated extra-hepatic biliary radicles in HIV patients.
Sonography is vital for assessing the location, number, size, shape, and presence/absence of fatty hilum of abdominal lymph nodes. In our study, lymphadenopathy was also a common finding, with significant association between periportal and mesenteric lymphadenopathy and CD4 levels. Similarly, multiple studies reported that abdominal lymphadenopathy was the most commonly identified abnormal finding that was significantly associated with CD4 levels and was an independent predictor of abdominal tuberculosis in HIV/AIDS patients.[3,4,5,12]
USG is the most commonly used imaging modality in the assessment of renal dysfunction in HIV/AIDS patients. A wide variety of disease processes can affect the kidneys of HIV patients and include HIV nephropathy, infections, malignancy, and drug toxicity.[6,13,14] In our study, renal involvement occurred at a lower incidence (2%) and presented as pyelonephritis and, in one case, renal abscess. There was no significant association observed between renomegaly and the presence of renal focal lesions with CD4 levels. In accordance with findings of study, Blessing et al.[5] and Di Fiori et al.[13] detected renomegaly in 19% and 20% of patients, respectively, which were not determined to be associated with CD4 levels. In fact, most patients involved in the studies had CD4 counts that were between 200 and 349 cells/mm3. Similarly, Adeyekun et al.[15] reported renomegaly in fewer (8%) participants and its appearance did not significantly correlate with CD4 levels.
We observed an increased degree of renal echogenicity in a small number (9.1%) of patients. In contrast to our findings, Blessing et al.[5] reported increased levels of renal cortical echogenicity in 37.3% patients and determined that its appearance significantly correlated with levels of CD4 cells. Likewise, Adeyekun et al.[15] observed increases in renal cortical echogenicity in 41.7% patients but did not observe that the abnormality correlated with CD4 counts. The reason that researchers observed increased prevalence of renal cortical echogenicity in these studies, could be that majority of patients included in the study had CD4 counts that were low (<200 cell/mm3). Although multiple factors contribute to the enhancement of renal echogenicity in HIV/AIDS patients, high viral load and low CD4 counts have been shown to be positive predictors of the pathology.[13]
HIV infection weakens gastric acid secretion, slows intestinal peristalsis, and diminishes cellular immunity. These factors promote enteritis and typhlitis, which is associated with infection by opportunistic pathogens like tuberculosis. The gastrointestinal pathologies observed in the current study included thickened caecum and terminal ilium secondary to tuberculous ileotyphlitis and occurred at an increased prevalence in patients with CD4 counts less than 200 cells/mm3. However, there was no significant correlation observed in patients between gastrointestinal abnormalities and CD4 counts. Blessing et al.[5] and Harriet et al.[16] reported the occurrence of thickened bowel walls in HIV patients significantly correlated with levels of CD4 cells. In accordance with the previous studies, we identified ascites in 5.4% of patients assessed and its presence did not significantly correlate with CD4 counts.[3,6,16] Tubo-ovarian involvement was seen in one patient diagnosed with inflammatory disease.
The weakened immune status of HIV/AIDS patients enhances their risk of developing malignancies. Therefore, early and accurate detection of HIV/AIDS-related malignancies and specific features of their imaging is vital for differentiating malignancies from their mimics. In HIV patients, the most common AIDS-defining malignancy is lymphoma and it is most likely to involve the liver, pancreas, gastrointestinal tract, spleen, kidneys, and retroperitoneal lymph nodes.[8,9] In our study, 1% of patients had lymphoma involving the liver, pancreas, and retroperitoneal lymph nodes.
In the current study, focal hypoechoic lesions within pancreas were detected in a small number of patients (0.5%). Interestingly, all the cases were diagnosed as lymphomas and had CD4 counts below 200 cells/mm3. Further, a significant correlation between the presence of focal hypoechoic lesions and CD4 levels was observed (P < 0.043). In contrast, Blessing et al.[5] observed that 10.3% of patients had an enlarged pancreas and 6% had a hypoechoic pancreas without any focal lesion. Moreover, there was no correlation between CD4 count and pancreatomegaly or hypoechogenicity observed. Similarly, Lito et al.[17] reported the presence of non-AIDS-defining pancreatic neuroendocrine tumors in HIV-infected patients. This was likely due to moderate immunosuppression that occurred in these patients (median CD4 count = 497cell/ mm3). We also observed dilated PD in 1% of patients assessed, which may have been due to atrophy of the pancreas.
Our study is limited by the absence of microbiological confirmation in all patients of liver abscess, abdominal tuberculosis, and splenic microabscess. However, we performed FNAC and/or biopsy in patients with high suspicion of malignancy and/or were not responding to antituberculosis/antibacterial treatment. There is also the possibility of a bias in our study as all the HIV/AIDS patients included were with positive abdominal USG findings and we already knew their CD4 counts. Therefore, outcomes might differ if only general HIV infected populations were studied without being aware of their CD4 counts. Finally, we cannot comment on or compare with HIV patients with low CD4 count without positive abdominal USG findings, as our study was limited to not include these patients.
CONCLUSION
USG is a readily available, safe, sensitive, and inexpensive imaging modality and is very useful for evaluating various abdominal pathologies. Certain discernible patterns of abdominal pathologies that can be evaluated through USG can enhance the accuracy of diagnosis in HIV/AIDS patients. Accurate interpretation of abdominal USG with knowledge of potential pathologic phenomena that may occur in AIDS patients with particular CD4 levels will facilitate narrowing differential diagnoses. Thus, USG will facilitate the assessment of HIV/AIDS patients in resource-limited areas that are common in India.
Ethical statement
This study was conducted after getting approval from the Institutional Ethics Committee (BJGMC/IEC/ Pharmac/D-0214015-15). All procedures were performed in accordance with the ethical standards of our institute as well as the 1964 Helsinki Declaration and its later amendments.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- The current role of abdominal ultrasound in the clinical management of patients with AIDS. Ultraschall Med. 2006;27:20-33.
- [CrossRef] [PubMed] [Google Scholar]
- Abdominal ultrasound findings in HIV infected patients and its correlation with CD4+ counts. Int J Sci Res. 2017;6:1632-7.
- [Google Scholar]
- Correlation of hepatobiliary ultrasound findings with CD4 count and liver function tests in HIV positive patients. Med J West India. 2013;41:86-8.
- [Google Scholar]
- Trans-abdominal ultrasonic findings correlated with CD4+ counts in adult HIV-infected patients in Benin, Nigeria. SA J Radiol. 2009;13:34-40.
- [CrossRef] [Google Scholar]
- AIDS effects in liver and biliary tract by using Ultrasound in Sudan. Afro Egypt J Infect Endem Dis. 2012;2:133-9.
- [CrossRef] [Google Scholar]
- Abdominal ultrasonography in HIV/AIDS patients in South-Western Nigeria. BMC Med Imaging. 2008;8:5.
- [CrossRef] [PubMed] [Google Scholar]
- Liver enlargement associated with opportunistic infections in patients with human immunodeficiency virus infection. J Gastrointestin Liver Dis. 2008;17:401-4.
- [Google Scholar]
- Four-year study of abdominal ultrasound in 900 Central African adults with AIDS referred for diagnostic imaging. Abdom Imaging. 2000;25:290-6.
- [CrossRef] [PubMed] [Google Scholar]
- Focal splenic lesions in patients with AIDS: Sonographic findings. Abdom Imaging. 1998;23:196-200.
- [CrossRef] [PubMed] [Google Scholar]
- Hepatic and biliary abnormalities in patients with AIDS: Sonographic-pathologic correlation. J Ultrasound Med. 1989;8:247-54.
- [CrossRef] [PubMed] [Google Scholar]
- Abdominal sonography in AIDS. A review. J Ultrasound Med. 1989;8:705-14.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic sonography of HIV-associated nephropathy: New observations and clinical correlation. AJR Am J Roentgenol. 1998;171:713-6.
- [CrossRef] [PubMed] [Google Scholar]
- Correlation of CD4 counts with renal disease in HIV positive patients. Saudi J Kidney Dis Transpl. 2008;19:603-7.
- [Google Scholar]
- Renal sonographic parameters in human immunodeficiency virus-infected subjects and relationship to CD4 cell count. Saudi J Kidney Dis Transpl. 2011;22:1164-8.
- [Google Scholar]
- Abdominal sonographic findings in severely immunosuppressed human immunodeficiency virus-infected patients treated for tuberculosis. J Tuberc Res. 2014;2:65-74.
- [CrossRef] [Google Scholar]
- Gastroenteropancreatic neuroendocrine tumours in patients with HIV infection: A trans-Atlantic series. Am J Med Sci. 2009;337:1-4.
- [CrossRef] [PubMed] [Google Scholar]






