Translate this page into:
Assessment of quality of life among head-and-neck cancer patients
*Corresponding author: Afsana Nizar, Department of Dietetics, Lords Hospital, Trivandrum, Kerala. afsananizar111@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Nizar A, Isaac BR. Assessment of quality of life among head-and-neck cancer patients. Indian J Med Sci 2022;74:1-5.
Abstract
Objectives:
To assess QOL of different head and neck cancer patients.
Materials and Methods:
A cross sectional study of 35 subjects with HNC was selected based on the type of cancer. After a background study, 35 subjects were chosen classifying on the type of cancer and were assessed using an interview schedule.
Results:
Physical as well as emotional score was poor among the group (312.5 and 349.5). The results had a high degree of variation.
Conclusion:
QOL among HNC patients were concluded to be poor.
Keywords
Quality of life
Head and neck cancers
Physical score
Emotional and social score
INTRODUCTION
WHO defines quality of life (QOL) as an individual’s perception of their position in life in the context of the culture and value systems in which they live in, in relation to their goals and expectations, standards, and concerns[1] (WHOQOL Group, 1995) and it closely resonates with the perception of health. With the increase in life expectancy in chronic diseases like cancer, the importance of maintaining an acceptable QOL is gaining importance. In conditions like head-and-neck cancers (HNCs), requiring a more radical treatment, longer survival mostly comes with a toll on QOL. Outcome of disease and efficacy of treatment is usually assessed at each stage of the treatment but the patient’s view of the treatment outcome in his daily life is usually not addressed. QOL is now increasingly perceived as the primary outcome of the treatment itself.[2] Moreover, QOL during treatment affects the overall response of the subject to the treatment itself.
According to GLOBCAN (2018) report, HNCs account for approximately 30–40% of all cancer sites, in India.[3] It mostly requires a multimodality treatment involving surgery, radiotherapy, as well as chemotherapy in most cases, affecting the subject’s physical, emotional, and social QOL to a large extent.[4] They can hence be a group vulnerable to lead a poor QOL during as well as post the treatment.
An effective tool to record the patient perception of his/her health is important to assess QOL. University of Washington (UW) developed a questionnaire that is briefly discussing all the domains in a set of 12 questions.[5] UW-QOL is a reliable instrument for assessing the QOL in Indian population and will be a vital tool for an insight into the short- and the long-term QOL of HNC patients.[6]
It is established by now the importance of the QOL perceived by a patient undergoing radical treatment methods involving impairment. At present, such an assessment is not a routine part of their treatment in countries like India, the study aims to bring attention into the very poor QOL in this group so that additional assistance can be provided to help each of them during the treatment as well as post the treatment to restore their social, physical, as well as psychological state. The study aims in conducting a QOL assessment in HNC patients using UW-QOL to bring about the importance of such an assessment in every stage of their treatment.
MATERIAL AND METHODS
The methodology of this study is discussed under the following headings:
Type of study
It was a cross-sectional study. In this way, this study provides a “snapshot” of the outcome and the characteristics associated with the diseased condition, at a specific point in time.
Selection of subjects
For the study, subjects with head or neck associated cancers were selected. A total of 35 subjects including male and female were selected.
Selection of area
The study was conducted in Msgr. Joseph Kandathil Memorial Cancer Research Centre, Cherthala. It was the first comprehensive cancer care center in a rural setting, in Kerala state of India with diagnostic, therapeutic, and palliative facilities for cancer care.
Selection of tools
For the interview, a pre-tested interview schedule prepared by the investigator was used to collect background information of the subjects along with the UW-QOL questionnaire which was developed to identify issues of concern of the individual patient. The questionnaire gives an overall scoring based on emotional, social, and physical status of the patient and allows the investigator to grade them accordingly.
Conduct of study
The consent to conduct the study and interview the patients and caretakers were obtained from the hospital authorities, the subjects, and the caretakers. A personal interview was conducted with subjects based on the questionnaire.
Data analysis and interpretation
Data were recorded, tabulated, and scored using Statistical Package for the Social Sciences Windows software, version 25. The collected data were analyzed and results were discussed.
RESULTS
For an individual to lead a good quality life, he should physically, socially, and emotionally be stable. UW-QOL questionnaire, used in the study consists of 12 single question domains. The domains are pain, appearance, activity, recreation, swallowing, chewing, speech, shoulder, taste, saliva, mood, and anxiety. The results thus obtained are given below.
Medical history
A brief medical history was recorded for each patient, mainly focusing on the type of cancer and the treatments they have undergone.
Ca tongue was the most common diagnosis, seen in 11 patients, which is followed by Ca larynx with six subjects. Ca buccal mucosa was found in four subjects, three subjects had carcinoma alveolus, and another three had Ca thyroid Figure 1. Two subjects had carcinoma cheek and one subject each suffered from cancers associated with brain, esophagus, nasopharynx, oropharynx, tonsil, and neck.
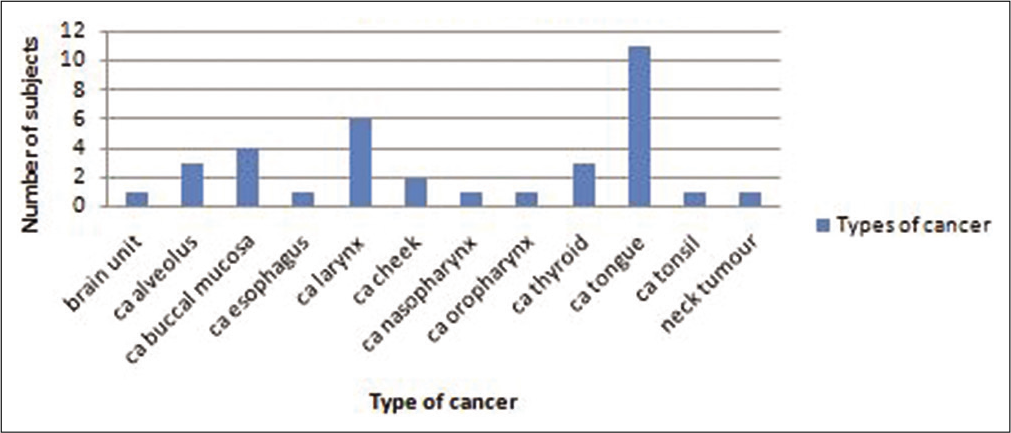
- Distribution of types of cancers in subjects.
In majority of the patients (77.1%), there was no relapse in the cancer, whereas 22.9% suffered a relapse Table 1.
| Relapse of the cancer | Frequency | Percentage |
|---|---|---|
| New diagnosis | 27 | 77.1 |
| Relapsed | 8 | 22.9 |
Treatment record seen in Figure 2 gives an insight into the physical, emotional, and nutritional difficulties experienced by the patient. It also gave an insight into the vulnerable group of patients to poor QOL. Treatment record is represented in the above figure, where the current treatment as well as the past treatments undergone for the present diagnosis is mentioned. More than half (60) of the subjects had undergone surgeries in the past and 57.1 had currently undergone a surgery, 31.4 had radiotherapy ongoing, and 22.9 had undergone radiotherapy in the past. About 5.7% of the subjects were currently under palliative treatment.
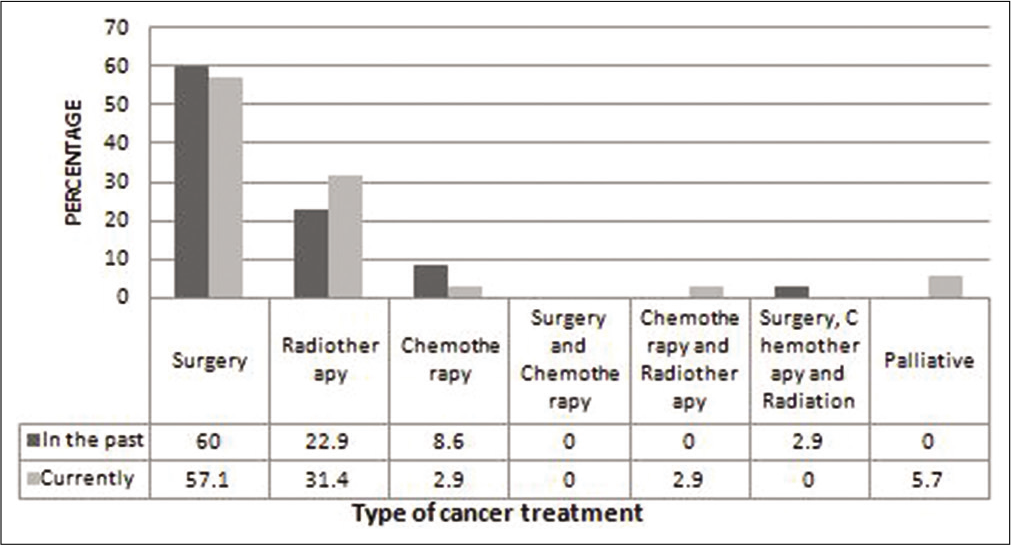
- Distribution of cancer treatment record of the subjects.
QOL
QOL questionnaire for HNCs was developed by UW in 1993 by Hassan and Muller. The tool has been validated by many studies to be brief, valid, and reliable. QOL is discussed under four categories as follows:
Symptoms and scores
Table 2 shows: Pain, 0: No pain; 25: There is mild pain not needing medication; 50: Moderate pain requiring regular medication; 75: Severe pain requiring prescription medicine; 100: Pain uncontrolled with any medication.
| Symptoms | Scores (percentage) | ||||
|---|---|---|---|---|---|
| 0 | 25 | 50 | 75 | 100 | |
| Pain | 2.9 | 20.0 | 62.9 | 5.7 | 5.7 |
| Appearance | 0.00 | 8.6 | 28.6 | 54.3 | 8.6 |
| Activity | 8.6 | 22.9 | 31.4 | 25.7 | 11.4 |
| Mood | 14.3 | 42.9 | 22.9 | 20.0 | 0.00 |
In appearance, 0: No change; 25: Minor change; 50: Appearance bothers the patient, yet chooses to stay active; 75: Feeling of being significantly disfigured leading to limiting of activities; 100: Cannot handle the change in appearance.
In activity, 0: Active like before; 25: Old pace could not be achieved sometimes but not often; 50: Often tired and slowed down activities; 75: Does not go out due to poor strength; 100: Confined to bed or chair.
In mood, 0: Excellent and unaffected by cancer; 25: Generally good; 50: Neither good nor depressed about cancer; 75: Somewhat depressed by cancer; 100: Extremely depressed with the diagnosis.
Among the subjects, 69.2% experienced moderate pain, requiring regular medications like paracetamol and 20% went through a mild pain but not requiring any medication.
Majority (54.3%) of the subjects felt significantly disfigured and limited their activities due to their appearance.
Activity was widely variable, 31.4% felt often tired and has slowed down their activities although they still get out. About 25.7% do not go out and complained of not having the strength to. Another 22.9% felt that were times when they could not keep up their old pace but not often.
Mood was analyzed and 42.9% felt their mood generally good and only occasionally affected by the cancer, while 22% felt neither good nor depressed about the cancer. Twenty percent of the subjects felt somewhat depressed with their cancer.
Table 3 shows: Sleep, 0: Good; 30: Fair; 70: Poor; 100: Very poor.
| Symptoms | Scores (percentage) | |||
|---|---|---|---|---|
| 0 | 30 | 70 | 100 | |
| Sleep | 2.8 | 40 | 40 | 17.1 |
| Saliva | 11.4 | 45.7 | 31.4 | 11.4 |
| Taste | 34.2 | 25.7 | 34.2 | 5.7 |
| Speech | 11.4 | 28.5 | 40 | 20 |
In saliva, 0: Normal saliva; 30: Lesser saliva but satisfied; 70: Too little saliva; 100: No saliva.
Taste: 0: Normal taste; 30: Most foods have normal taste; 70: Can taste some foods; 100: Cannot taste any foods.
In speech, 0: Same as before; 30: Have difficulty but is understood over phone; 70: Only close people can understand; 100: Cannot be understood by any.
Forty percent of the subjects had a fair and another 40% had a poor sleep. Another 17.1% complained of very poor quality of sleep and 45.7% complained of less saliva than normal but found it to be enough. It was noticed that 31.4% had too little saliva. Only some foods could be tasted by 25.7% another 25.7% expressed that they can taste most foods normally. Forty percent of subjects found that only their family and friends could understand them and 28.5% had difficulty saying certain words but could be understood over phone.
Health-related quality
Health-related quality of the subjects depicted in Table 4, was perceived to be somewhat worse by around 65.7% whereas 20% felt the quality to be about the same as before to the month before they developed cancer. However, 14.3% complained that the QOL was much worse.
| Quality of health | Percentage |
|---|---|
| Much better | 0.0 |
| Somewhat better | 0.0 |
| About the same | 20.0 |
| Somewhat worse | 65.7 |
| Much worse | 14.3 |
Study depicted that 51.4% of the subjects believed that their health-related quality for the past 7 days to be fair, 34.3% did find the quality poor, and a minor of 8.6% felt it very poor Table 5. Some of them (5.7%) remarked their health-related quality to be good.
| Health-related quality of life | Percentage |
|---|---|
| Outstanding | 0.0 |
| Very good | 0.0 |
| Good | 5.7 |
| Fair | 51.4 |
| Poor | 34.3 |
| Very poor | 8.6 |
Physical function score
Physical function score is a culmination of six domain scores – those of chewing, swallowing, speech, taste, saliva, and appearance. It gives a perception of the physical status of a patient.
Figure 3 illustrates the percentage of physical function score of the subjects under different types of cancers experienced. It shows that the least mean score was seen in patients suffering from Ca oropharynx, followed by a score of 34.72 among Ca alveolus, 35.42 among Ca larynx, 36.25 among Ca cheek, 43.56 among Ca tongue, 43.33 among Ca tonsil, and 45.42 among carcinoma buccal mucosa. A score of 55.83 was seen in Ca nasopharynx followed by Ca brain with 6.67 and 71.39 in Ca thyroid whereas Ca esophagus had a good score of 84.17. The best score was seen among a newly diagnosed neck tumor that has not undergone any treatment at the time.
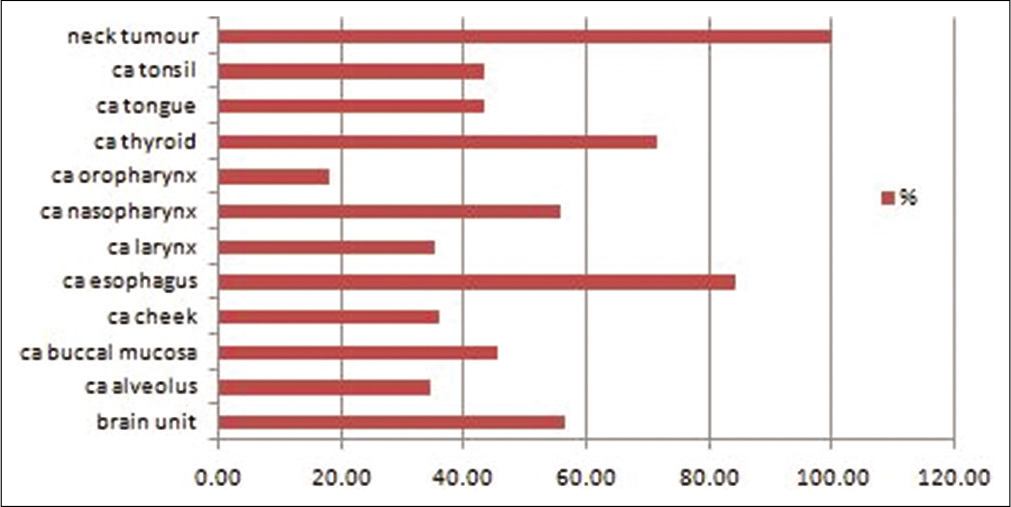
- Physical function score of the subjects.
Social and emotional score
Social and emotional score is the culmination of six domains, namely, pain, activity, recreation, mood, anxiety, and shoulder function [Figure 4]. Among the subjects, the lowest mean score was of subjects with carcinoma cheek of 37.08 followed by 36.94 among Ca larynx, and 37.5 among Ca tonsil. Ca oropharynx had a score of 42.50, Ca alveolus had a mean score of 55.28, and Ca brain had 53.33 as the score. Ca tongue had a score of 51.21. Good scores were seen among Ca esophagus with 75 and Ca thyroid with 76.94 and neck tumor had the highest score of 79.17, again due to the fact that the patient had not undergone any treatment.
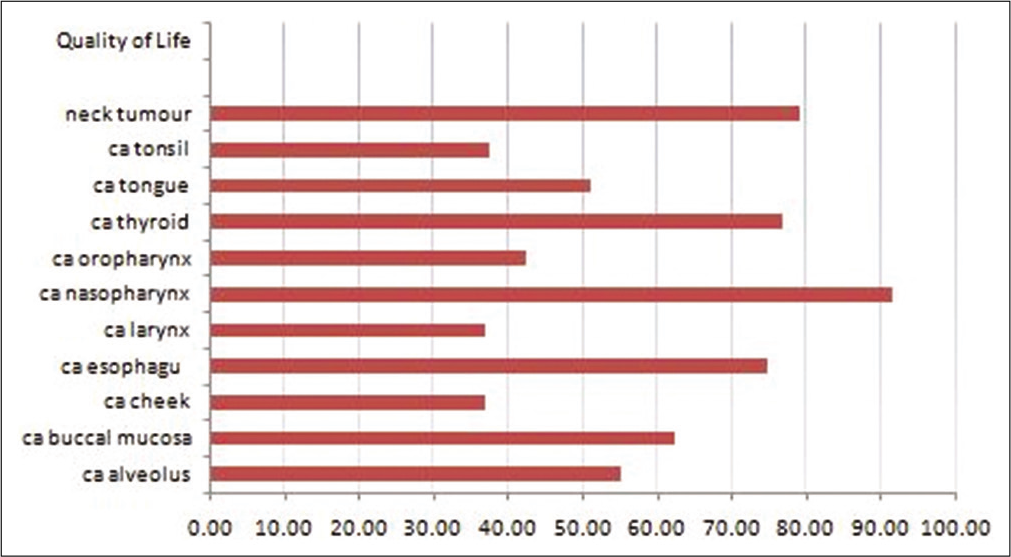
- Social and emotional score of the subjects.
DISCUSSION
Surgery being the most promising treatment, more than half of the subjects had surgeries in the past or recent period. A great subset of the subjects had cancers associated with tongue, larynx, and buccal mucosa. Surgeries in these areas can significantly alter appearance, swallowing, chewing, saliva, etc. Radiotherapy and chemotherapy can further disturb the emotional state of the subject. Therefore, the analysis of the patients QOL is of significance in each step of the treatment as well as post-therapy period.
When assessing symptoms such as pain, appearance, activity, mood, and sleep, the scores were very poor, every subject faced a low score in any one of these symptoms once the treatment began.
Physical function score was poor for all the subjects being treated for various HNCs but was better in carcinoma esophagus and neck tumors due to the fact that they were both in the beginning of their treatment and not much radical treatment was undergone. Cancers affecting oropharynx, alveolus, larynx, and tongue had the least scores largely due to the area of resection and radiation affecting the physical score largely.
Social and emotional score had almost similar results. Carcinomas of thyroid, esophagus, and neck tumors had good scores comparing to the extremely poor scores among carcinoma cheek and larynx, which both had a severe impairment in appearance, mood, and anxiety.
The study sums up the poor QOL of HNC patients. Assessment of their QOL can be monitored in every step of the treatment, which would give insights into the measures that can help them maintain a more satisfactory lifestyle. Now treatment methods such as physiotherapy, occupational therapy, psychology counseling, and group counseling are gaining importance in helping cancer patients worldwide to overcome their treatment-related complications.
Identification of their hurdles is the first step in helping them have a better life beyond cancer, a good assessment tool like the one we have studied here can help the patient as well as the caregivers achieve a good treatment response.
CONCLUSION
The study sums up the very poor QOL among HNC patients. Further, management can be undertaken once an assessment is made in each stage of their treatment and care to provide effective and efficient methods to a better QOL throughout, especially post the treatment.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- The World Health Organization Quality of Life assessment (WHOQOL): Position paper from the World Health Organization. Soc Sci Med. 1995;41:1403-9.
- [CrossRef] [Google Scholar]
- Quality of life versus length of life considerations in cancer patients: A systematic literature review. Psychooncology. 2019;28:1367-80.
- [CrossRef] [PubMed] [Google Scholar]
- Head and neck cancer burden in India. Int J Head Neck Surg. 2013;4:29-35.
- [CrossRef] [Google Scholar]
- Indian clinical practice consensus guidelines for the management of squamous cell carcinoma of head and neck. Indian J Cancer. 2020;57(Suppl):S1-5.
- [CrossRef] [PubMed] [Google Scholar]
- University of Washington quality of life questionnaire In: Michalos AC, ed. Encyclopedia of Quality of Life and Well-Being Research. Dordrecht: Springer; 2014.
- [CrossRef] [Google Scholar]
- Validation of the University of Washington quality of life questionnaires for head and neck cancer patients in India. Indian J Cancer. 2007;44:147-54.
- [CrossRef] [PubMed] [Google Scholar]






