Translate this page into:
Florid vascular proliferation due to focal necrotizing enterocolitis in infancy: A case report
*Corresponding author: Seyma Ozturk, Department of Pathology, Sanlıurfa Training and Research Hospital, Sanlıurfa, Turkey. seymoozturk@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Ozturk S, Erdogan Duzcu S, Boran C, Ozturk H. Florid vascular proliferation due to focal necrotizing enterocolitis in infancy: A case report. Indian J Med Sci. 2024;76:144-6. doi: 10.25259/IJMS_87_2024
Abstract
Vascular anomalies rarely emerge in the gastrointestinal tract. The most prevalent benign vascular lesions include angiodysplasia, Dieulafoy’s lesion, vascular ectasia, vascular malformations, and hemangiomas. Florid vascular proliferation (FVP) is also a rare benign vascular lesion associated with intussusception in adults. In infants, there are only a few cases in literature. Although FVP usually presents as a mass in the intestine, it is a nonneoplastic lesion and is thought to occur due to a reactive process. In this study, we present a case of FVP due to an attack of focal necrotizing enterocolitis in a 10-month-old infant.
Keywords
Vascular proliferation
Necrotizing enterocolitis
Intussusception
Colon
Infant
INTRODUCTION
First introduced by Ramsden et al. in 1993, florid vascular proliferation (FVP) is a rare benign vascular anomaly associated with intussusception in adults. In this first case, FVP was detected as a primary angiomatous lesion in a patient with recurrent episodes of intussusception.[1] In general, FVP is thought to develop due to a non-neoplastic reactive process. However, it can histologically be confused with benign and malignant vascular tumors in the colon. Therefore, it may need surgical treatment and then pathological examination for a differential diagnosis.[2] On the other hand, FVP is quite rare in infants, and there is only one case reported by Park et al. in the literature.[3] We present another case of FVP due to a focal necrotizing enterocolitis (NEC) attack in a 10-month-old infant.
CASE REPORT
A 10-month-old male infant born prematurely was admitted to the emergency department with complaints of abdominal distention, vomiting, and constipation. His medical history revealed that he was born at 27 weeks, weighed 700 g, and stayed in the intensive care unit for 2 months. During his stay in the intensive care unit, he had nutritional intestinal problems and was treated with suspicion of NEC. He had also been repeatedly brought to the outpatient clinic with complaint of constipation. The laboratory findings showed a hemoglobin value of 11.4 g/dL (expected value: 11.5 – 17.5 g/dL). Abdominal ultrasonography (USG) revealed a 15 mm-long colon segment suspicious for intussusception in the right lower quadrant. The patient was immediately taken to the operating room. We observed no intussusception during the operation. There was a stricture in the 2 cm-long segment of the sigmoid colon, 20 cm proximal to the peritoneal reflection. The segment was resected, and an appendectomy was performed in the same session.
The macroscopic examination resulted in a 1.5 cm-diameter soft-consistency lesion obstructing the lumen in the 2 cm-long segment of the sigmoid colon. While the wall thickness in this area was 8 mm, the depth of the lesion was 7 mm. In the microscopic examination, the mucosal surface was focally ulcerated; there was a vascular lesion consisting of capillary vessel proliferations starting from the mucosal area and extending to the muscularis propria and subserosa [Figure 1a]. Vascular proliferation was partly accompanied by spindle-shaped fibroblast proliferation and inflammatory cell infiltration. In most of the capillaries, the lumen was prominent, but in some, the luminal structures almost completely disappeared. Endothelial cells in the capillary wall were slightly swollen, but significant nuclear atypia and atypical mitosis were not observed in endothelial cells the inflammatory infiltrate mainly consisted of lymphocytes and plasmocytes, but occasional eosinophils were also noted. There were lymphoid follicle structures with prominent germinal centers in peripheral regions. There was fibrous scar tissue covering a large area adjacent to the lesion in the submucosal area [Figure 1b]. The microscopic examination of the appendix vermiformis showed reactive lymphoid hyperplasia. Ganglion cells were present in the myenteric plexus and in the submucosal area.
![(a) We observed a vascular lesion consisting of capillary vessel proliferations starting from the mucosal area and reaching the subserosal area. There is focal ulceration (upper left) in the mucosa [Hematoxylin-eosin (H&E), ×25]. (b) Vascular proliferation is accompanied by fibroblastic proliferation and inflammatory cell infiltration. Fibrous scar tissue is seen as a globular eosinophilic mass in the center of the figure (H&E, ×100).](/content/101/2024/76/3/img/IJMS-76-144-g001.png)
- (a) We observed a vascular lesion consisting of capillary vessel proliferations starting from the mucosal area and reaching the subserosal area. There is focal ulceration (upper left) in the mucosa [Hematoxylin-eosin (H&E), ×25]. (b) Vascular proliferation is accompanied by fibroblastic proliferation and inflammatory cell infiltration. Fibrous scar tissue is seen as a globular eosinophilic mass in the center of the figure (H&E, ×100).
The immunohistochemical staining revealed vascular proliferation. The endothelial cells were positively stained with CD31 [Figure 2], CD34, factor 13a, and vimentin. Pancytokeratin was negative. In addition, SMA, desmin, MSA, CD117, CD68, caldesmon, S100, D2-40, and CD99 were negative. Ki-67 proliferative activity was low.
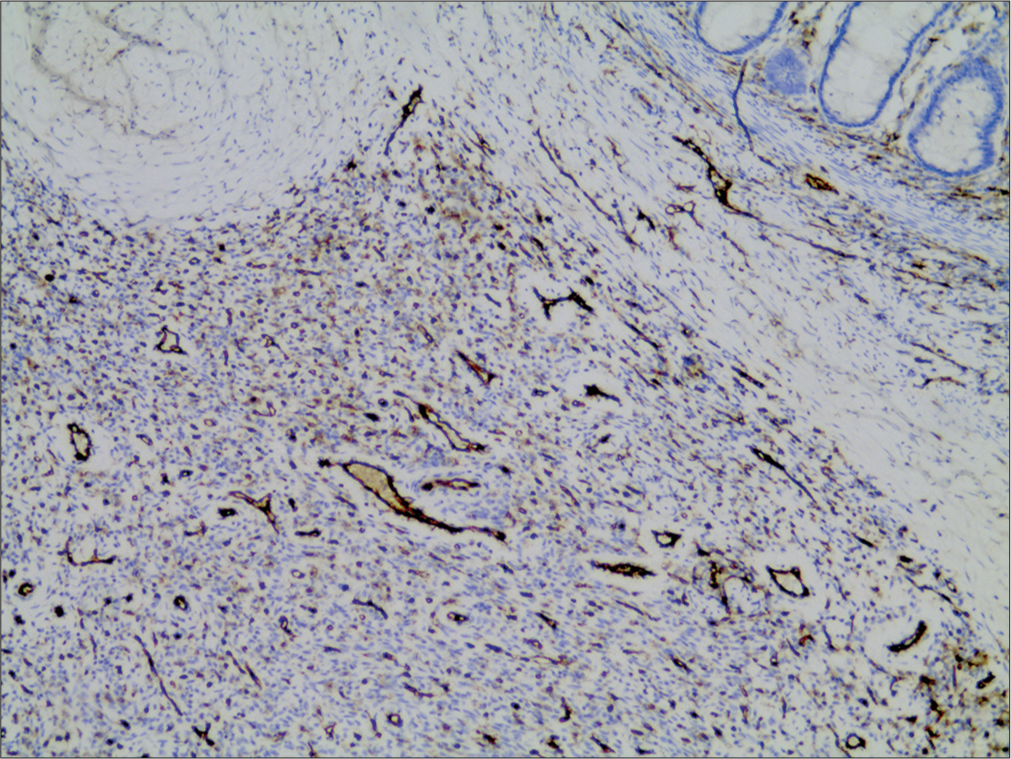
- Immunohistochemical staining with CD31. Proliferating vascular structures are seen in brown (immunoperoxidase, ×100).
With these findings, we reported the case as fluoride vascular proliferation associated with focal NEC. Informed consent was obtained from the parents of the patient.
DISCUSSION
Vascular anomalies rarely show up in the gastrointestinal tract. The most prevalent benign vascular lesions in this area include angiodysplasia, Dieulafoy’s lesion, vascular ectasia, vascular malformations, and hemangiomas.[2] Among the malignant vascular tumors, Kaposi’s sarcoma is frequently observed in the gastrointestinal tract in patients with immunodeficiency. On the other hand, angiosarcoma is relatively rare in this location.[4] As for the FVP, it is a rare benign vascular lesion in adults, and it is a far less common vascular lesion in infants.[3]
The pathogenesis of FVP has not been fully elaborated so far. Most of the patients have intussusception with FVP, and histological changes are seen in the mucosa. Ischemic changes and benign nuclear features in endothelial cells suggest that FVP develops due to a reactive process.[4] Since FVP is a rare entity, one may have some difficulties distinguishing it from benign and malignant vascular lesions. Ramsden et al. (one case),[1] Bavikatty et al. (four cases),[4] Agostini-Vulaj et al. (one case),[2] and Park et al. (one case)[3] mentioned that FVP presents as a mass in the intestine. In the microscopic examination, Park et al. detected inflammatory cell infiltration and fibroblast proliferation mixed with small vessel proliferation, forming well-circumscribed solid nodules in the deep parts.[3] Moreover, characteristic intranuclear and cytoplasmic viral inclusions were observed in endothelial and stromal cells and immunohistochemically stained positive for cytomegalovirus antigen.
Although NEC exhibits similar symptoms to intussusception in infancy, it is often seen in the neonatal period in premature infants.[5] NEC characteristically leads to ischemia and patchy necrosis of the intestinal mucosa. The severity of necrosis in the intestinal wall varies from small, localized involvement to extensive transmural involvement. Intestinal stricture formation occurring during the healing process of NEC is among the best-known complications.[6] The submucosa is often thick and fibrotic due to stricture formation. Even some cases present with mucosal ulceration and inflammation.[7] In our case, although clinical and USG findings were compatible with intussusception, we could not observe it. We identified a soft mass lesion in the resected segment that almost completely occluded the lumen. The lesion is composed of a mixture of proliferating vascular structures and inflammatory cells. Collagenous, fibrous scar tissue is observed adjacent to the lesion. This scar tissue may indicate that the vascular lesion emerged as a reactive process. The lesion probably developed due to NEC in the neonatal stage. The fibrous scar tissue may be supposed to be important evidence of previous NEC.
The findings of the intestinal obstruction and anatomical localization of the obstruction may also lead to thinking about Hirschsprung’s disease as a cause of obstruction, which is the most common cause of intestinal obstruction in children. Histologically, it is characterized by aganglionosis extending from the anus to the proximal at varying rates.[8] In our case, we detected ganglion cells in the submucosal area and the myenteric plexus.
The majority of the vascular lesions in the intestine are benign and show similar histological features to hemangiomas. Epithelioid hemangioma may present as a tumoral mass in the colon.[9] Its distinct feature is the epithelioid appearance of the endothelial cells lining the vessel walls. An epithelioid endothelial cell has a round nucleus and an eosinophilic cytoplasm. In addition, it is accompanied by an inflammatory infiltrate rich in eosinophils and lymphocytes. Our case had some similarities with epithelioid hemangioma, but we found fewer eosinophils than there are in epithelioid hemangioma. In addition, epithelioid endothelial cell character was not evident. There was also fibrous scar tissue adjacent to the lesion.
Angiosarcoma should also be considered among the vascular lesions in the intestine. Prominent nuclear atypia and mitosis are seen in the endothelial cells of angiosarcomas.[10] In our case, endothelial cells were benign in character, and no obvious cytological atypia or mitosis was observed.
In the differential diagnosis, one should also consider the causes of intra-abdominal mass in the infant. The intra-abdominal masses often include embryonal rhabdomyosarcoma, infantile fibrosarcoma, myofibroma, and inflammatory myofibroblastic tumors. The differentiation of these tumors can only be possible with the help of histopathological and immunohistochemical findings.[11]
CONCLUSION
FVP is a rare benign vascular lesion seen in adults, mostly due to intussusception. It is much rarer among infants. There is only one reported case of FVP. The focal NEC attacks might be one of the causes of their occurrence in infants. One should keep in mind that FVP may develop due to previous focal NEC attacks leading to intestinal obstruction in early childhood.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Florid vascular proliferation in repeated intussusception mimicking primary angiomatous lesion. J Clin Pathol. 1993;46:91-2.
- [CrossRef] [PubMed] [Google Scholar]
- Florid vascular proliferation of the small bowel and colon, a potential masquerader of malignancy: Report of three cases. Int J Surg Pathol. 2019;27:609-12.
- [CrossRef] [PubMed] [Google Scholar]
- Cytomegalovirus-associated intussusception with florid vascular proliferation in an infant. J Pathol Transl Med. 2015;49:270-3.
- [CrossRef] [PubMed] [Google Scholar]
- Florid vascular proliferation of the colon related to intussusception and mucosal prolapse: Potential diagnostic confusion with angiosarcoma. Mod Pathol. 2001;14:1114-8.
- [CrossRef] [PubMed] [Google Scholar]
- Challenging diagnosis between intussusception and necrotizing enterocolitis in premature infants. Pediatr Int. 2014;56:e1-3.
- [CrossRef] [PubMed] [Google Scholar]
- Intestinal strictures post-necrotising enterocolitis: Clinical profile and risk factors. J Neonatal Surg. 2014;3:44.
- [CrossRef] [PubMed] [Google Scholar]
- Late intestinal strictures following successful treatment of necrotizing enterocolitis. Acta Paediatr Suppl. 1994;83:80-3.
- [CrossRef] [PubMed] [Google Scholar]
- Hirschsprung disease-current diagnosis and management. Indian J Pediatr. 2017;84:618-23.
- [CrossRef] [PubMed] [Google Scholar]
- A case of angiolymphoid hyperplasia with eosinophilia in proximal ascending colon mimicking colon carcinoma. Bangladesh J Med Sci. 2018;17:158-60.
- [CrossRef] [Google Scholar]
- Benign vascular tumors and malformations In: Enzinger and Weiss’s soft tissue tumors (7th ed). Netherlands: Elsevier; 2020. p. :697-756.
- [Google Scholar]
- Borderline and malignant fibroblastic/myofibroblastic tumors In: Enzinger and Weiss’s soft tissue tumors. Netherlands: Elsevier; 2019. p. :306-17.
- [Google Scholar]






