Translate this page into:
National and international comparison of Turkish health system outcome indicators and policy recommendations
*Corresponding author: Umut Beylik, Department of Health Management, University of Health Sciences, Keçiören, Turkey. beylik28@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Topaktaş G, Beylik U. National and international comparison of Turkish health system outcome indicators and policy recommendations. Indian J Med Sci. doi: 10.25259/IJMS_230_2024
Abstract
Objectives:
The study aims to analyze and make recommendations based on comparison of the results of the Turkish Health System both national and internationally.
Materials and Methods:
In the study, comments were made within the scope of trend analysis and comparison methods and discussed with the literature. The study data belonged to 2022 and were obtained from the Health Statistics Yearbook of the Ministry of Health, TURKSTAT, Organisation for Economic Co-operation and Development Health Data and EUROSTAT database. Average life expectancy, infant mortality rate, maternal mortality rate, satisfaction ratio with health-care services, and health expenditure impact data were taken into consideration.
Results:
There was poor performance internationally in terms of infant mortality rate and maternal mortality rate. There are extreme differences in these indicators between regions of Turkey. The level of patient satisfaction is well-positioned internationally. However, looking at its trend, it has entered a period of stagnation and decline. The increase in health expenditures in Turkey has also resulted in an increase in average life expectancy and patient satisfaction.
Conclusion:
It has been observed that Turkish’s health system is in the process of transition from middle-upper income group countries to upper-income group countries in terms of its results and performance, but the imbalances in access to service and health service quality between regions and the stagnating system produce negative results and cannot renew itself.
Keywords
Health system
Health policy
Basic health indicators
International comparison
INTRODUCTION
When it comes to health system performance evaluation, countries with close or similar income levels, it is understood that analyses aim to reveal the reasons for injustice in financing, failure to meet users’ expectations and failure to achieve similar health outcomes, and the deficiencies of the health system.[1] In addition, the application of the “Benchmarking” method, which is a management approach, is extremely important in terms of taking the countries with the best or better health results as an example.[2] In addition, there is the potential to create value in comparing countries with similar health status and socioeconomic characteristics, determining priorities in the health system, the need for health reform or developing policies and strategies for small improvement areas.
The World Health Organization (WHO) defines performance evaluation in health systems as the process of monitoring, evaluating, establishing connections, and examining the achievement of high-level health system goals based on a country’s specific health system strategies. Apart from this main purpose, it also aims to determine goals and priorities for health systems, to provide a focal point for coordinating activities in the health system and determining policies, to measure and monitor processes in achieving goals, and to inform society and all relevant stakeholders.[3] In health systems performance evaluation, within the framework of the comprehensiveness and sustainability of the health system, it is seen that basic health indicators (average life expectancy, infant mortality rate, maternal mortality rate, deaths from diseases, etc.) are primarily taken as basis.[4,5]
When the factors affecting the health structure of individuals and therefore societies are examined, these factors are mostly grouped under four basic headings; it can be said that it is heredity, environment, lifestyle or behaviors, and health system. When we look at the studies on health system performance conducted by Balçık and Konca,[6] Mirmirani and Lippmann,[7] Afonso and Aubyn,[8] Asandului et al.,[9] Şener and Yiğit[10] and Ahmed et al.,[11] it is seen that the resources used in the provision of health services are used as input variables.
This study was conducted to make a comparative analysis at national and international levels within the scope of the outcomes of the Turkish Health System and to make recommendations.
MATERIALS AND METHODS
As the basic method of the study, trend analysis and comparison were used through secondary data converted into information. Since the data and information used were prepared with the same scope and content as the databases from which they were taken and provided with definitive evidence, a direct comparison was made, and comments and suggestions were made by discussing them with the literature.
In the study, evaluations and analyses were made based on real data. The data of the study were obtained from the 2022 Health Statistics Yearbook published by the Ministry of Health, the Turkish Statistical Institute website, the Organisation for Economic Co-operation and Development (OECD) Health Data, and the EUROSTAT database. Within the scope of the data provided, comparisons were made on a country basis (national), within a country (by province), at an international level (developed, underdeveloped, and developing countries; OECD countries; and the European Union (EU) and on a global scale, and evaluations and recommendations were made.
As the dataset used in the study, the basic indicators that reflect the health system results mentioned in the literature were considered as follows: “Life Expectancy at Birth, Infant Mortality Rate, Maternal Mortality Rate, Satisfaction Rate with Health Services, and the Effect of Health Expenditures on These Indicators.” The definition and calculation methods of the relevant indicators are given below.[12]
The data used in the study were not subjected to statistical analysis but were ready-made data compiled from relevant databases.
The study data were presented to the public openly and transparently by the competent national and international authorities and were analyzed by showing the data sources. In this context, there was no need to obtain ethical and administrative permission.
RESULTS
Life expectancy at birth
In Figure 1,[13] which shows the average life expectancy at birth, Türkiye’s data are 77.5; it is higher than the average of the World and Upper Middle Income Group countries; it was found to be lower than the WHO European Region, EU, OECD, and High-Income Group countries.
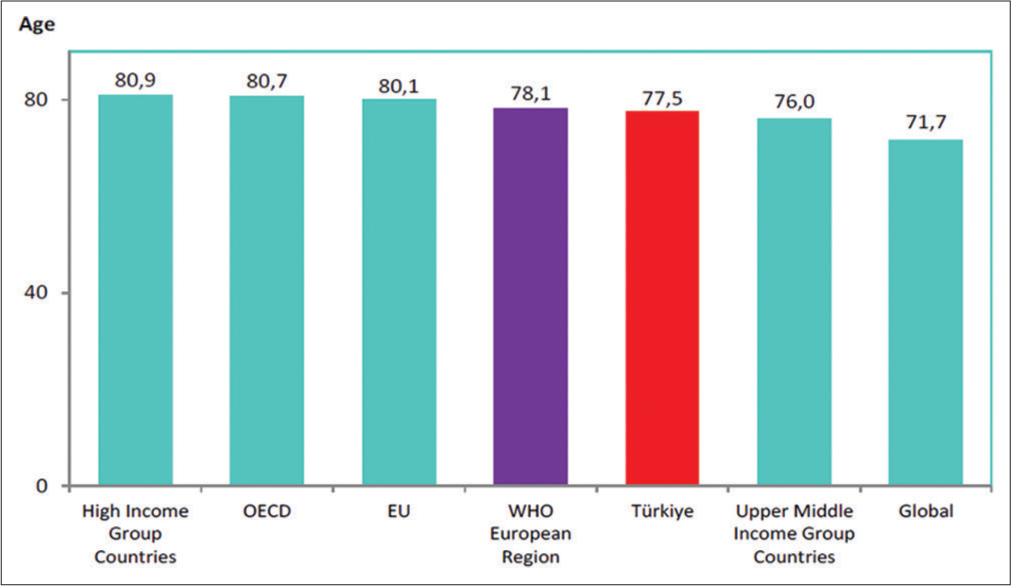
- International comparison of life expectancy at birth (Age), 2022. EU: European union, WHO: World Health Organization, OECD: Organisation for economic co-operation and development.
Infant mortality rate
According to Figure 2,[13] which shows the infant mortality rate in Turkey by regions (NUTS-1), Turkey’s average for all weeks was 9.1/1000, the lowest data were in Western Marmara with 6.2/1000, while the highest data were in Western Marmara. It was realized in Southeastern Anatolia with 13.9.
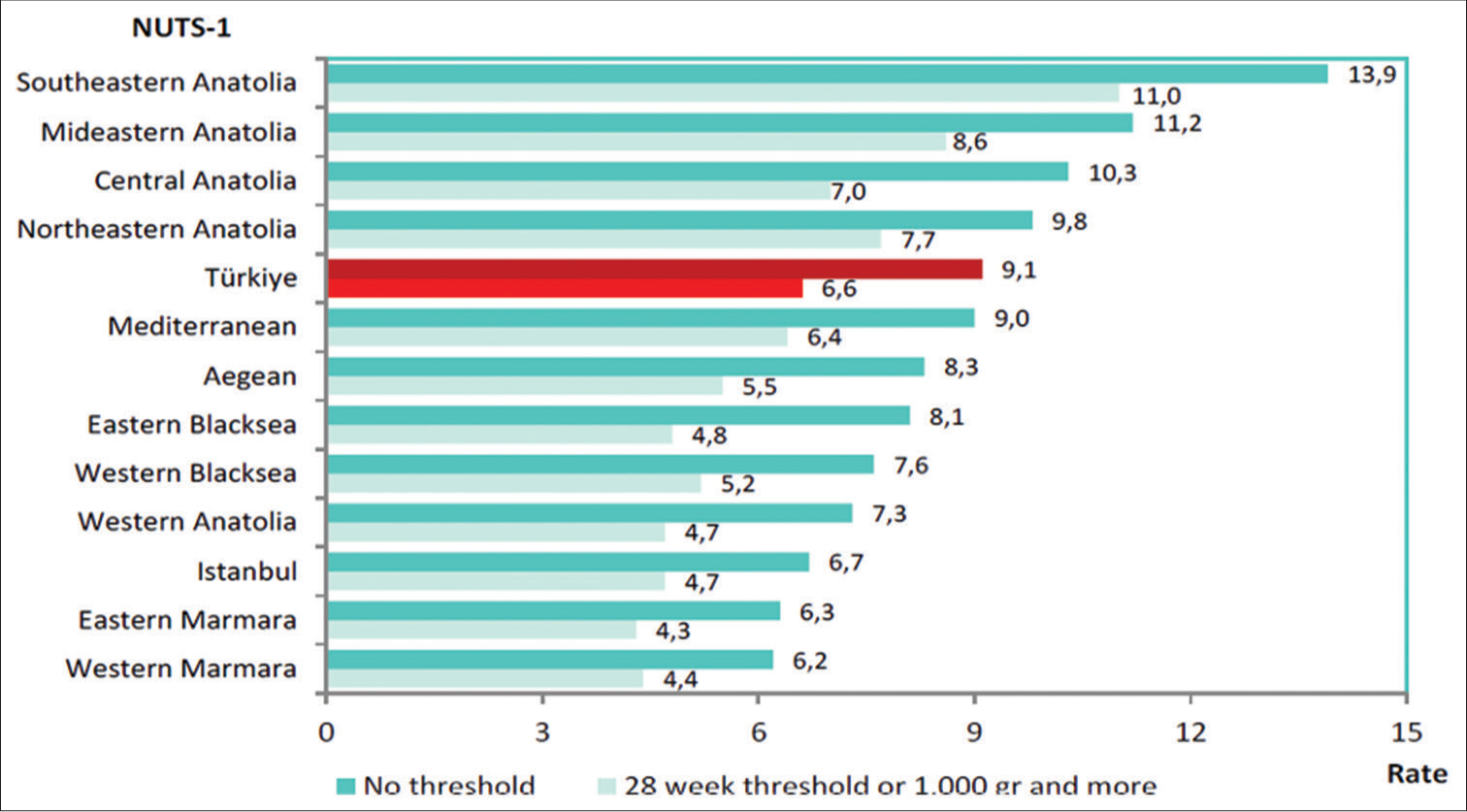
- Infant mortality rate by NUTS-1 (per 1.000 live births), 2022. NUTS: Nomenclature of territorial units for statistics.
When we look at the scope of the international comparison of infant mortality rate, Turkey is ranked similarly in terms of life expectancy at birth but is much lower in proportion. Although it seems to be in a good position compared to the world average, it has an infant mortality rate that is 2–3 times higher on average than the EU, OECD, Upper Income, and WHO European Region.[13]
Maternal mortality rate
Looking at Figure 3,[13] the situation in terms of maternal mortality rate, which is one of the basic health indicators, is the infant mortality rate. Turkey’s average is 12.6/100,000, the lowest data were in the Western Marmara region with 2.9/100,000, and the highest data were in the Aegean region with 19.8/100,000. Compared to the Turkish average, differences between regions are high and the standard deviation is also high.
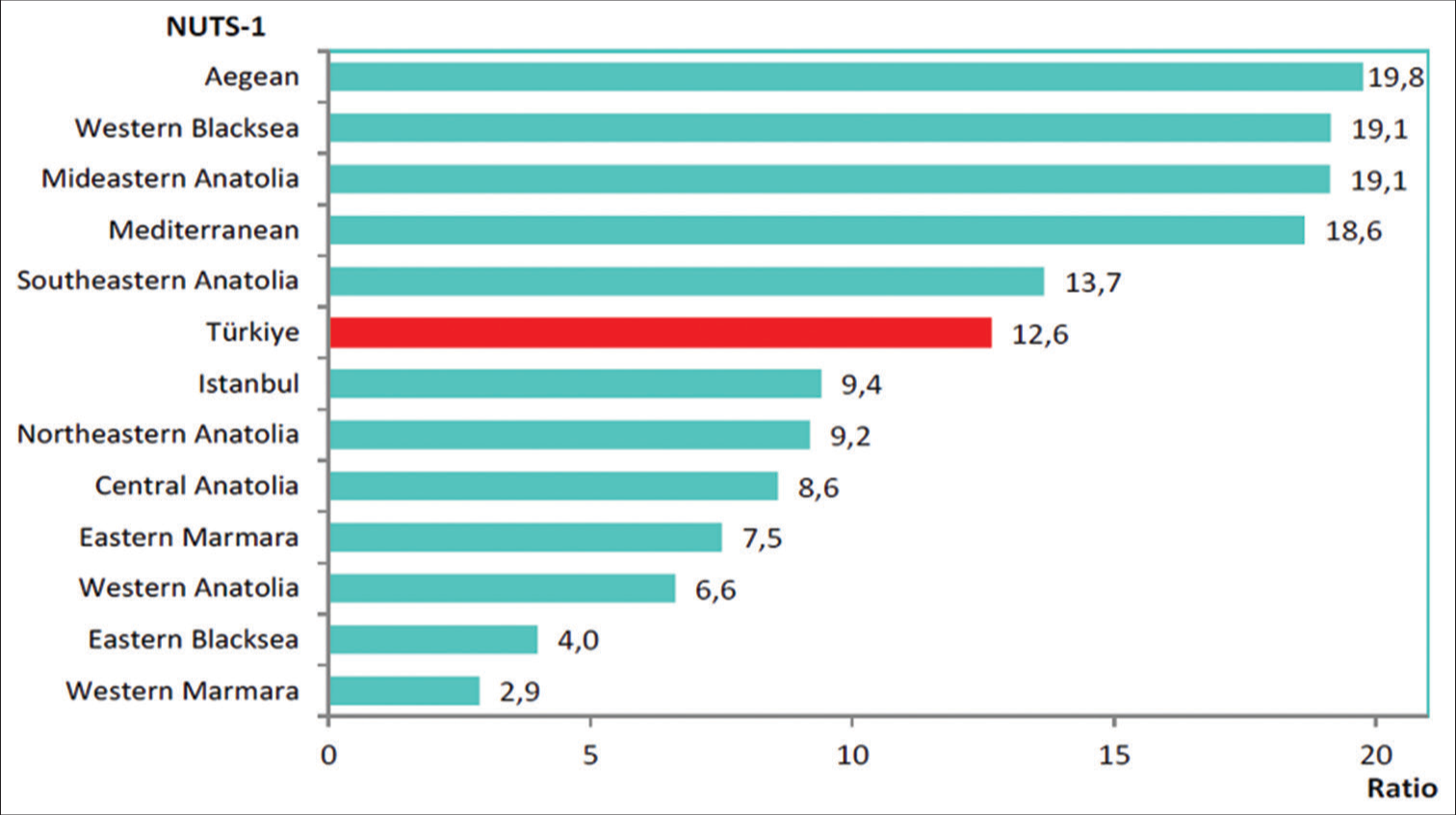
- Maternal mortality ratio by NUTS-1 (per 100.000 live births), 2022. NUTS: Nomenclature of territorial units for statistics.
According to the international comparison within the scope of maternal mortality rate, it can be said that the World average is very high.
Satisfaction rate with health services
The linear function emerges when looking at Figure 4;[14,15] it shows that health expenditures and patient satisfaction are in the same direction and positively. Although this is also valid for Turkey, it is understood from Figure 4 that a slight increase in health expenditures in Turkey resulted in a greater increase in the satisfaction rate, that is, the marginal benefit was higher. A similar situation exists in countries to the left and above the middle line but also close to the satisfaction line (y-axis).
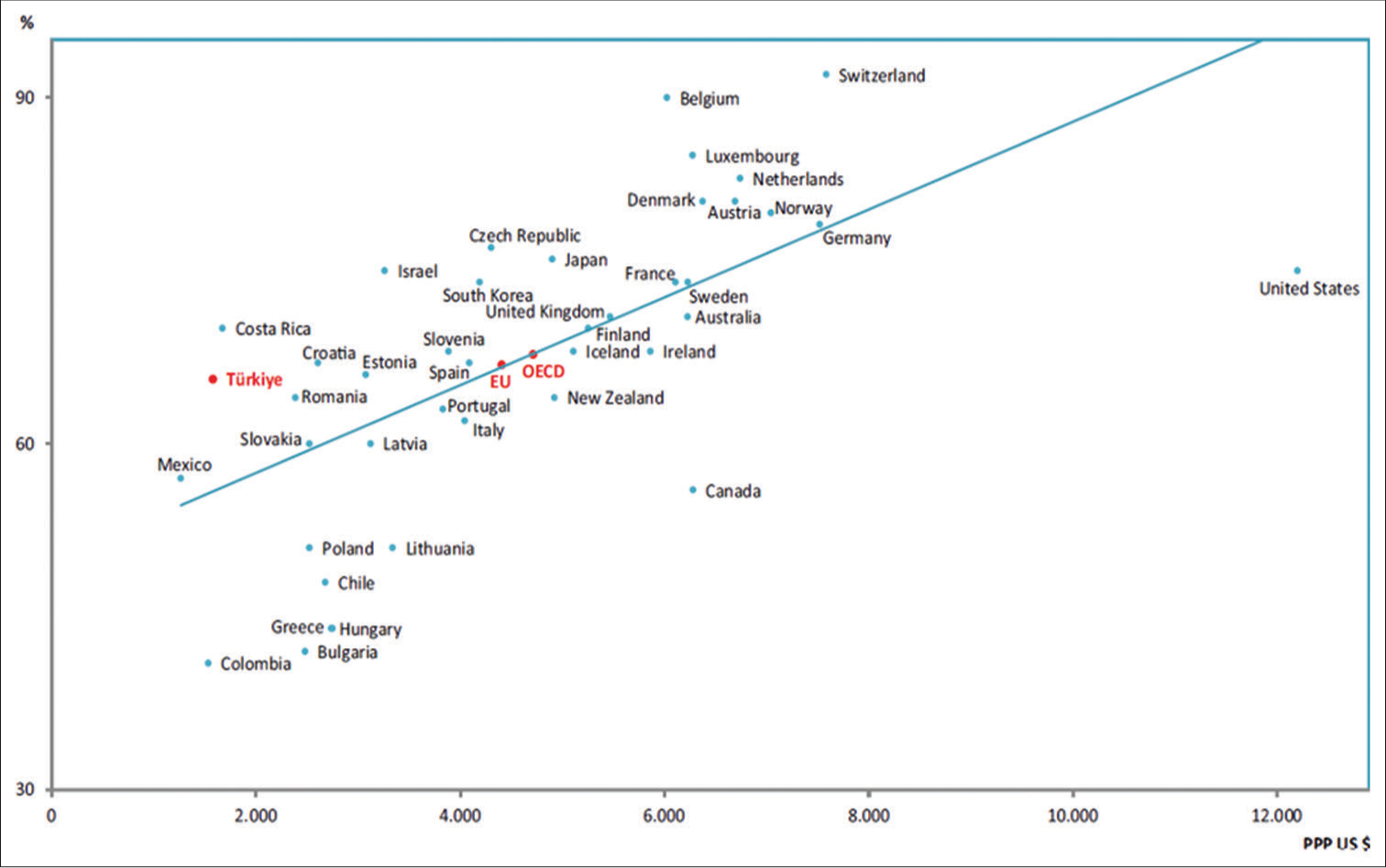
- Satisfaction with health care services, (%) 2022 and total current health expenditure per capita (PPP US $), 2021. EU: European union, OECD: Organisation for economic co-operation and development.
When Figure 5,[15,16] which shows the relationship between Life Expectancy at Birth and Total Current Health Expenditure per Person, is evaluated; it is seen that the average life expectancy also increases with the increase in health expenditures. The strong-positive relationship in these data of Turkey, which is below the OECD average in terms of both data, shows that it has a high-positive potential.
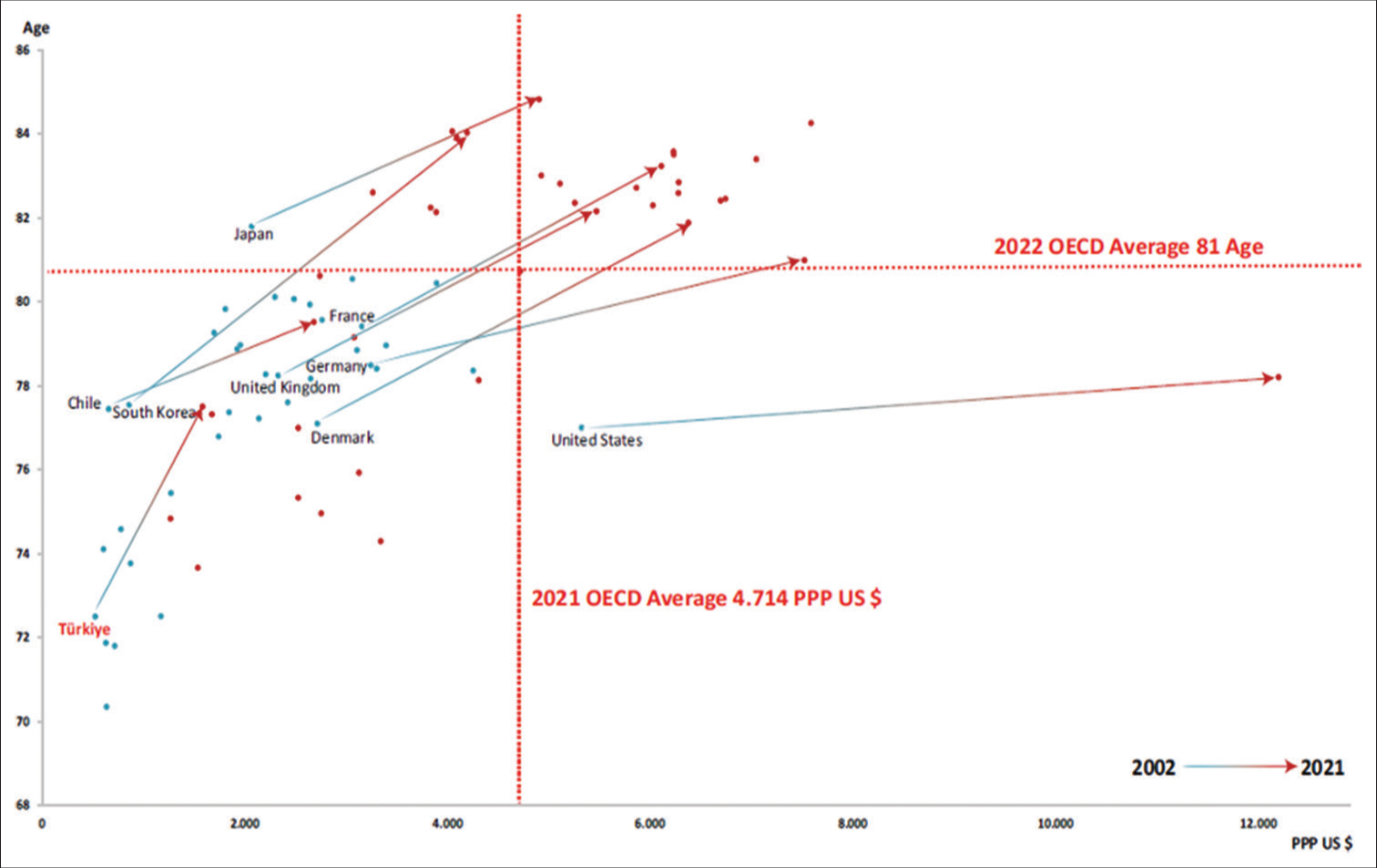
- Life expectancy at birth (age) and total current health expenditure per capita (PPP US $), 2002, 2021. OECD: Organisation for economic co-operation and development.
According to Figure 4, which compares OECD countries with Turkey, the average patient satisfaction rate in 2022 was 68% for OECD countries and has been around this level (68–71%) in the past 10 years. It has been observed that the Turkish average is lower and has decreased significantly, falling from 73% to –66% in the past 10 years.
Countries such as Belgium and Switzerland, which have high patient satisfaction levels and have managed to maintain this for a long time, and Japan and the Czech Republic, which have shown a positive leap, need to evaluate their health systems in the context of patient satisfaction and other parameters and determine practices that can be adapted to Turkey.
DISCUSSION
Study data are data made available to the public by relevant legal organizations and are assumed to be accurate. However, the study is limited within the framework of the indicators discussed. Considering that the performance of health systems can be evaluated comparatively with additional indicators (e.g., financial indicators and other clinical quality indicators) in addition to the indicators discussed in this study, the data covered by the study have a limitation.
The results of this study have been prepared from the latest data made public by the competent authorities. It should also be considered very important to discuss it together with recent similar studies in literature. In this context, it is thought that comparing and discussing with similar studies will guide in terms of results and recommendations.
Examples of studies that produce similar findings to this study: Balçık and Konca compared the health systems of OECD countries and Türkiye in their study and used average life expectancy and infant mortality rate variables as output variables.[6] In their study, Tıraş and Ağır made a descriptive comparison through health and demographic indicators for some selected years in the example of D-8 group countries, including Turkey, which has not been examined before and concluded that health expenditures positively affect demographic indicators.[17] As a result of their study, Daştan and Çetinkaya found a 6-year increase in average life expectancy with the increase in health expenditures in the 20-year period between 1990 and 2010,[18] similar to the findings of this study. In the study conducted by Kocaman et al., the health systems of OECD countries were compared, and average life expectancy and under-5 mortality rate were used as output variables.[19]
Examples of studies that are not consistent with these study findings: Şener and Yiğit used five inputs (number of hospital beds per capita, number of doctors per capita, health expenditure per capita, number of magnetic resonance images per capita, and smoking rate) and two outputs to measure the technical efficiency of health systems in OECD countries. Infant mortality rate and healthy life expectancy were used in their study.[10] Türkiye was among the productive countries in this study.
Yıldırım, in his study comparing the health systems of Türkiye and EU countries, used total health expenditure as input variable and average life expectancy and infant mortality rate as output variables and showed Turkey among the efficient countries. In such studies, giving priority to output-oriented approaches rather than input-oriented approaches, especially in evaluating the performance of health systems, can pave the way for more accurate analyses.[20] Likewise, it suggests that inefficient countries use unnecessary health-care human resources and hospital beds. In the study conducted by Lorcu, the efficiency performances of the health systems of 27 EU member countries and Turkey, a full candidate country, were measured with similar indicators and Turkey was among the productive countries.[21]
When the study findings are evaluated, it is seen that Türkiye’s position in the world is good in terms of life expectancy at birth, especially the health expenditures add additional value to life expectancy.
In the context of maternal and infant mortality rates, extreme imbalances between regions in Turkey have come to the fore and attracted attention. At the same time, there seems to be a need for rapid improvement in the data, and it can be said that the family medicine system has deficiencies in terms of pregnancy and baby/child follow-up. Likewise, strengthening and expanding the Maternal and Child Health Centers and channeling today’s technological opportunities into monitoring and guidance activities in this field have been seen as basic issues. In the study conducted by Kurnaz et al.,[22] it was determined that adequate information about pregnancy was not provided in Turkey and the negative impact of this situation on maternal and infant deaths was mentioned.
According to the research conducted by Yetim and Çelik, it has been found that the level of unmet needs is 13.2% in Türkiye, and it is more among women than men. Furthermore, the level of unmet needs decreases when the education level is higher.[23]
Within the scope of satisfaction with health services, it is predicted that Turkey is in a stagnant and slowing position; health expenditures have recently been an effective tool in increasing the patient satisfaction rate, but there has been a significant decline in the access and quality aspects of the health system and if no intervention is made, the decline may accelerate.
When the study findings are evaluated in terms of marginal benefit, it is noteworthy that Turkey provides more additional life expectancy with less health expenditure compared to many other countries.
However, although Türkiye has made a faster leap forward, it has been observed that it is still relatively behind among the compared countries in terms of both average life expectancy and patient satisfaction. In this context, Turkey directs its health expenditures correctly, which can be attributed to the fact that its health plans and policies yield positive results. However, the fact that Türkiye has gone backward, especially in patient satisfaction rates in the past 10 years, and has made us think that it should give importance to the quality and accessibility of health services.
CONCLUSION
When maternal and infant mortality rates are evaluated in Turkey, the problem of access to health services and imbalances in resource distribution are among the main problems. In addition, due to the stagnation and downward trend in patient satisfaction rates in the past 10 years, quality improvement activities in health services should be prioritized. In this context, it can be said that reformist and inclusive health policies are needed.
Ethical approval
Since the secondary data used in the study are publicly available and accessible and do not contain personal information, it was not necessary to obtain ethics committee approval.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Assessment of the world health report 2000. Lancet. 2000;356:1598-601.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of health financing on health systems performance: An evaluation on European Union member and candidate countries. Socioeconomics. 2020;28:229-42.
- [CrossRef] [Google Scholar]
- Performance and quality measurement in occupational health services: Current status and agenda for further research. Am J Ind Med. 2001;40:295-306.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of health systems performance of OECD countries with Malmquist Index. J Ankara Haci Bayram Veli Univ Fac Econ Admin Sci. 2019;21:666-82. Available from: https://dergipark.org.tr/en/download/article-file/887755
- [Google Scholar]
- Health care system efficiency analysis of G12 countries. Int Bus Econ Res J. 2004;3:35-42.
- [CrossRef] [Google Scholar]
- Non-parametric approaches to education and health expenditure efficiency in OECD countries. J Appl Econ. 2005;8:227-46.
- [CrossRef] [Google Scholar]
- The efficiency of healthcare systems in Europe: A data envelopment analysis approach. Proc Econ Finance. 2014;10:261-8.
- [CrossRef] [Google Scholar]
- Technical efficiency of health systems: A study on OECD countries. Süleyman Demirel Univ Soc Sci Inst J. 2017;26:266-90.
- [Google Scholar]
- Measuring the efficiency of health systems in Asia: A data envelopment analysis. BMJ Open. 2019;9:e022155.
- [CrossRef] [PubMed] [Google Scholar]
- Estimation of factors affecting life expectancy at birth: Example of E-7 countries. Cumhuriyet Univ J Econ Admin Sci. 2021;22:145-67.
- [CrossRef] [Google Scholar]
- General directorate of health information systems 2022 Health statistics yearbook. 2022. Ankara. Available from: https://dosyasb.saglik.gov.tr/eklenti/48054/0/siy202205042024pdf [Last accessed on 2024 Apr 22]
- [Google Scholar]
- Available from: https://www.oecd.org/els/health-systems/health-data.html [Last accessed on 2023 Dec 18]
- Turkish Statistic Institute (Turkstat) Available from: https://data.tuik.gov.tr/kategori/getkategori?p=saglik-ve-sosyalkoruma-101 [Last accessed on 2023 Dec 22]
- [Google Scholar]
- Eurostat. Available from: https://ec.europa.eu/eurostat/web/products-datasets/-/teicp060 [Last accessed on 2023 Nov 14]
- [Google Scholar]
- Comparison of D-8 countries in terms of health expenditures: A descriptive analysis. J Kahramanmaras Sütçü Imam Univ Fac Econ Administr Sci. 2017;7:195-220.
- [Google Scholar]
- Comparison of health systems, health expenditures and health indicators of OECD countries and Turkey. Soc Secur J. 2015;5:104-34.
- [Google Scholar]
- European union health policies and comparative technical efficiency analysis of health systems of European Union member and candidate countries. Hacettepe University, Institute of Health Sciences, Doctoral Thesis.
- [Google Scholar]
- Evaluation of the activities of Turkey and European Union Countries in the field of health with data envelopment analysis (DEA), (Doctoral Thesis) Istanbul: Istanbul University; 2008.
- [Google Scholar]
- How and how long do family physicians follow up pregnant women? Türk Aile Hek Derg. 2015;19:187-95.
- [CrossRef] [Google Scholar]
- Access to Healthcare: The Issue of Unmet Needs. Toplum Sosyal Hizmet. 2020;31:423-40.
- [CrossRef] [Google Scholar]







