Translate this page into:
Barriers and facilitators of human papillomavirus vaccination uptake in India: A systematic review
*Corresponding author: Aditya B. Saran, Hinduhridaysamrat Balasaheb Thackeray Medical College and Dr. R. N. Cooper Municipal General Hospital, Mumbai, Maharashtra, India. psaran183@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Saran AB, Gada MB. Barriers and facilitators of human papillomavirus vaccination uptake in India: A systematic review. Indian J Med Sci. 2025;77:34-9. doi: 10.25259/IJMS_9_2025
Abstract
Objectives
Human papillomavirus (HPV) is a primary cause of cervical cancer, a major public health concern in India. Despite the availability of HPV vaccines, uptake remains suboptimal due to various barriers. This systematic review aims to explore the barriers and facilitators influencing HPV vaccination in India.
Materials and Methods
A systematic search of PubMed, Google Scholar, ScienceDirect, and Livivo databases was conducted following Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines. Inclusion criteria included studies from 2014 to 2024 that focused on HPV vaccination awareness, barriers, and facilitators in India. Data were synthesized narratively due to heterogeneity among studies.
Results
Thirteen studies were included. Key barriers identified were cost, lack of awareness, misinformation, and sociocultural factors. Facilitators included educational interventions, physician recommendations, and subsidized vaccination programs. School-based campaigns and community engagement were effective in improving vaccine acceptance. However, marginalized populations and out-of-school girls remain underserved.
Conclusion
Addressing economic and sociocultural barriers, enhancing awareness, and expanding targeted vaccination programs are essential to improve HPV vaccination rates in India. Aligning these efforts with the World Health Organization’s 90/70/90 strategy can significantly reduce the cervical cancer burden.
Keywords
Health education
Human papillomavirus vaccine
Human papillomavirus
Vaccination coverages
INTRODUCTION
Human papillomavirus (HPV) is a major cause of dermatological disorders and malignancies, including cervical, anal, penile, vaginal, vulvar, and oropharyngeal cancers.[1-3] It is the most common sexually transmitted infection, spreading through skin-to-skin or sexual contact.[4,5] While many infections clear spontaneously, persistent HPV can lead to cancer.[1]
Cervical cancer remains the leading cause of cancer-related deaths among women in low- and middle-income countries, despite being highly preventable.[6] In 2022, India recorded 127,526 cases and 79,906 deaths, making it the second most common cancer among women.[7,8] HPV vaccination significantly reduces cervical cancer risk, with immunization available for girls aged 9–26 in India, without requiring prior Pap or HPV screening.[9]
Despite vaccine availability, uptake remains low due to economic constraints, sociocultural factors, and concerns over safety.[10,11] The World Health Organization’s (WHO’s) 90/70/90 strategy aims to eliminate cervical cancer by vaccinating 90% of girls by 15, screening 70% of women by 35 and 45, and treating 90% of detected cases.[12] This approach could prevent over 62 million cases globally.[12] However, awareness and vaccination uptake remain alarmingly low.[13]
Educational interventions improve vaccine acceptance, yet school-based programs often miss out-of-school girls.[13-15] Expanding coverage to young men could further curb HPV transmission.[16] However, misinformation, cultural beliefs, and hesitancy remain major obstacles.[17-19]
Addressing barriers through education, community engagement, and public health initiatives is critical to increasing HPV vaccination coverage.[13,20,21] This review examines facilitators and barriers to HPV vaccination in India, aligning with WHO’s goal of cervical cancer elimination by 2120.
MATERIALS AND METHODS
This systematic review follows the Integrated Methodology approach outlined in the Joanna Briggs Institute Reviewers’ Manual (2015), synthesizing quantitative and qualitative studies using a mixed-methods approach.[22] The Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines were used to ensure compliance with standardized reporting.[23] Due to data heterogeneity, a meta-analysis was not performed.
Search strategy
A comprehensive literature search was conducted in PubMed/MEDLINE, Google Scholar, Science Direct, and Livivo using PRISMA-based Population, Intervention, Comparator, Outcome criteria.[24,25] The search terms included “HPV vaccination,” “cervical cancer,” “India,” “barriers,” “facilitators,” “acceptance,” and “awareness.” Boolean operators (AND, OR) refined the search. Reference lists of included studies were screened, but no additional relevant studies were found.
Eligibility criteria
Inclusion criteria
Studies were included if they (1) were published in the past 10 years (2004–2024); (2) were conducted in India; (3) focused on HPV vaccination awareness, attitudes, uptake, facilitators, or barriers; (3) included primary data; (4) targeted populations of any age, (adolescents, parents, healthcare providers, marginalized communities); and (5) were published in English and indexed in the selected databases.
Exclusion criteria
Studies were excluded if they (1) lacked search keywords in the title or abstract; (2) were unavailable full texts or abstract-only papers; (3) focused solely on cervical cancer treatment, not prevention; (4) lacked empirical data; and (5) did not provide relevant information on HPV vaccination.
Data extraction
Two independent reviewers screened titles and abstracts for eligibility. The Zotero citation manager was used to organize search results and remove duplicates.[26] Full texts were assessed against the inclusion criteria, and key data were extracted into a standardized form, capturing author(s), year, study design, sample size, population characteristics, HPV vaccination uptake, facilitators, barriers, and effectiveness of educational interventions. The screening process followed the Moher model, shown in the PRISMA flow diagram [Figure 1].[27]
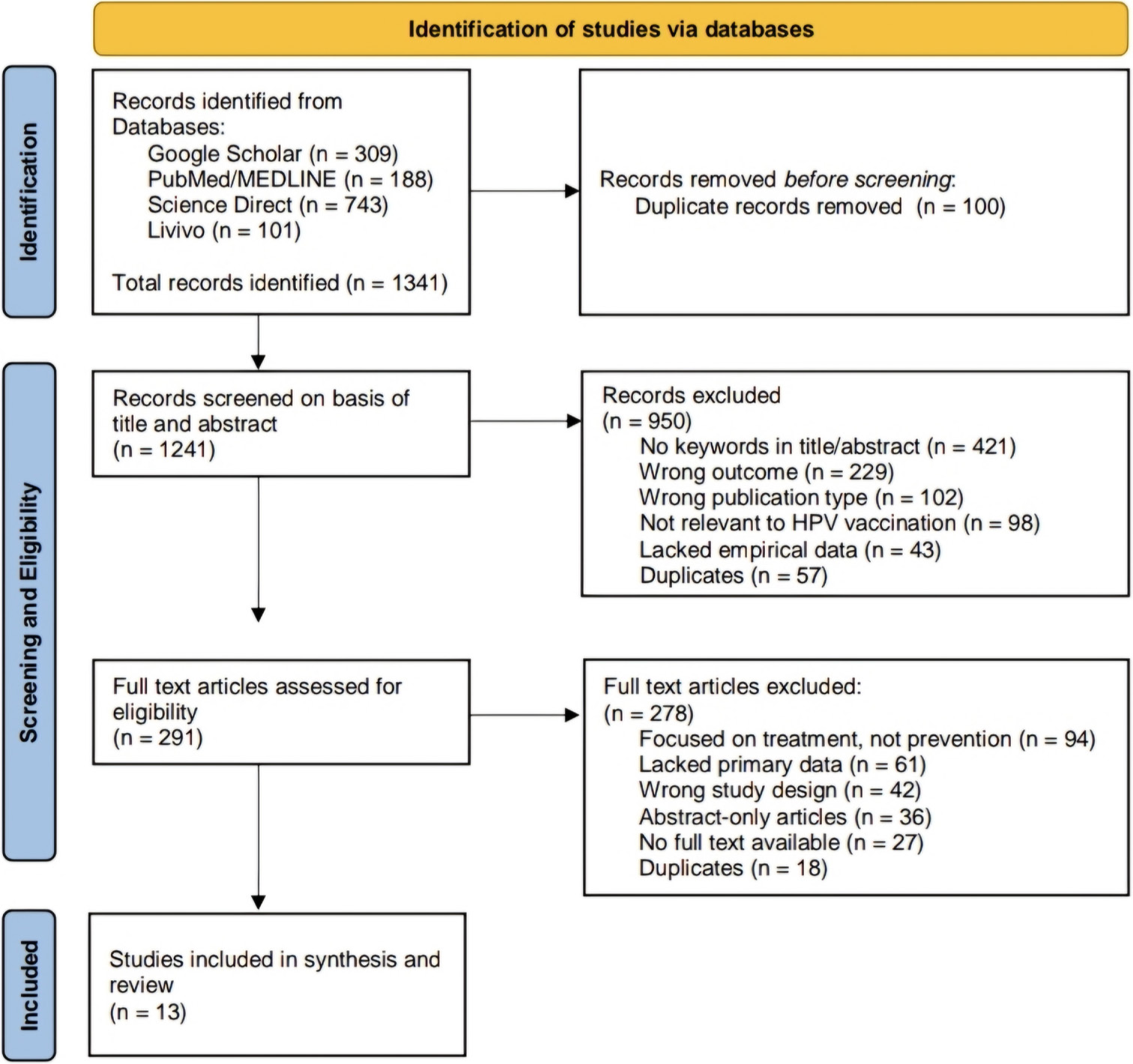
- Preferred Reporting Items for Systematic Reviews and Meta-analyses flowchart. For more information, visit: http://www.prisma-statement.org/. HPV: Human papilloma virus.
Quality assessment
The methodological quality of included studies was evaluated using the Newcastle–Ottawa Scale for observational studies and the Cochrane Risk of Bias Tool for randomized controlled trials. Discrepancies between reviewers were resolved through discussion.
Data synthesis
Data were tabulated following Joanna Briggs Institute guidelines.[22] Two researchers independently extracted and cross-checked data for accuracy. Findings were narratively synthesized, summarizing key barriers, awareness levels, and the impact of educational interventions on vaccine acceptance. Where applicable, quantitative data were aggregated to present vaccination uptake trends and intervention effectiveness.
RESULTS
This systematic review identified thirteen studies that met the inclusion criteria, focusing on HPV vaccination uptake, barriers, and awareness in India [Table 1]. The studies highlight significant gaps in knowledge and vaccination rates among parents, adolescents, and healthcare providers. Findings reveal various barriers and facilitators, providing insights into improving vaccine uptake and reducing cervical cancer burden.
| Study | Study population | Sample size | Study type | Key observations |
|---|---|---|---|---|
| Roy and Shankar[9] | Parents/caregivers, eligible females (9–26 years) |
Not mentioned | Editorial | Low awareness and financial constraints hinder HPV vaccine uptake; school-based programs aim to improve accessibility. |
| Ray et al.[10] | Mothers of adolescent daughters | 319 | Cross-sectional | 79% willing to pay for HPV vaccine, but affordability is low. Awareness and subsidies needed. |
| Degarege et al.[11] | Parents of adolescent girls | 1609 | Cross-sectional | 73.6% unaware of HPV; urban parents were more aware While rural parents were more hesitant. |
| Krokidi et al.[13] | Adolescents (9–20 years), university students |
7 studies | Systematic review | Health education increased HPV vaccine uptake. Barriers: Cost, awareness, and cultural beliefs. |
| Swain and Parida[14] | Young girls | 240 | Pretest-posttest study | Educational improved vaccination acceptance (86%), and screening uptake (58.3%). Sensitization programs needed. |
| Holroyd et al.[15] | Out-of-school adolescent girls | Not specified | Qualitative | Barriers: low awareness, literacy, and accessibility. Community-based strategies recommended. |
| Belani et al.[16] | Young men (general and HIV/AIDS patients) | 178 | Cross-sectional | High vaccine acceptance (83–98%). Barriers: Cost, fear of side effects. Facilitators: Doctor recommendations. |
| Parveen et al.[17] | Indian adults | 639 | Cross-sectional | High vaccine hesitancy. Predictors: religious beliefs, fear of COVID-19, vaccine convenience. |
| Manjunath and Revannasiddappa[18] | Female medical personnel | Not specified | Cross-sectional | 94.3% knew HPV causes cervical cancer, but only 4.1% were vaccinated. Hesitancy due to false sense of security. |
| Tsu et al.[21] | HPV vaccination pilot programs (India, Peru, Uganda, Vietnam) | Not specified | Literature review | Success depends on service delivery, community outreach, and cross-sector coordination. |
| Rashid et al.[28] | Undergraduate students (16–26 years) | 1,580 | Survey | Girls had higher awareness than boys. Educational interventions needed for vaccine promotion. |
| Madhivanan et al.[29] | Parents of adolescent girls | 800 | Survey | 71% accept HPV vaccination. Delaying vaccination to later ages may improve uptake. |
| Vahabi et al.[30] | Women (30–69 years) and families | 240 | Mixed-methods | Sexual health education improved screening rates. 115/120 women chose HPV self-sampling. |
HPV: Human papillomavirus, HIV: Human immunodeficiency virus, AIDS: Acquired immunodeficiency syndrome
Awareness and knowledge gaps
Economic barriers
Cost: Many families, especially in rural or low-income areas, struggle to afford the vaccine, which is often not covered by public health programs. In rural Haryana, mothers were willing to vaccinate daughters but found it unaffordable.[10]
Access: Limited healthcare facilities in remote areas, coupled with transportation costs, hinder vaccine availability.[10]
Sociocultural factors
Misinformation
Gender-related factors
Healthcare infrastructure challenges
Facilitators for HPV vaccination uptake
Education and awareness: School programs and media campaigns effectively increase vaccine acceptance.[13,14]
Subsidized vaccination: Government initiatives, such as free or low-cost school-based programs, improve accessibility.[9,10]
Healthcare provider role: Physician recommendations and training healthcare workers significantly boost uptake.[21]
Community engagement: Involvement of religious leaders, educators, and peer groups fosters trust and reduces hesitancy.[30]
Male inclusion: Vaccinating boys can enhance overall coverage and lower transmission rates.[16]
DISCUSSION
The findings from this systematic review illuminate the multifaceted challenges surrounding HPV vaccination uptake in India, a country grappling with a significant cervical cancer burden. Despite the introduction of HPV vaccines as a preventive measure, coverage remains alarmingly low due to a combination of economic, sociocultural, and informational barriers. Awareness about HPV and its vaccine remains insufficient, even among critical groups such as healthcare providers and college students.[18,28] This lack of knowledge underscores the need for targeted educational interventions. These interventions have proven effective in enhancing awareness and acceptance among diverse populations, particularly parents and young girls,[14] but must be tailored to address the specific cultural contexts and needs of marginalized communities and out-of-school girls, who are often overlooked in traditional school-based programs.[15] A study by Krokidi et al. further emphasizes significant knowledge gaps among college students in India, necessitating structured campaigns in academic settings to address misinformation and low awareness.[13]
Economic barriers, including the high cost of vaccines and limited access to healthcare facilities, further impede vaccination efforts.[10] The willingness of parents to vaccinate often does not translate into action due to financial constraints. This highlights the pressing need for policy interventions aimed at subsidizing costs or providing vaccines through public health initiatives.[21] Such programs, if effectively implemented, could ensure equitable access to the HPV vaccine, particularly in rural and underserved areas. Furthermore, parental attitudes shaped by factors such as religion, age, and misconceptions about vaccine safety must be addressed through culturally sensitive messaging that emphasizes the vaccine’s efficacy and the importance of early vaccination.[11] Madhivanan et al. identified parental preference to delay vaccination until daughters reach adolescence or adulthood, which reduces vaccine efficacy, further underscoring the importance of timely interventions.[29]
The inclusion of young men in vaccination strategies also represents a promising avenue for reducing HPV transmission and cervical cancer risk.[16] By fostering a more inclusive approach involving both genders, public health initiatives could enhance overall vaccination rates and contribute to broader community acceptance. However, this requires a shift in public perception to recognize HPV as a shared health concern rather than one specific to women.
Misinformation and cultural stigma remain significant barriers, perpetuating vaccine hesitancy.[17] The spread of myths regarding vaccine safety and efficacy, often fueled by social media, underscores the importance of comprehensive communication strategies. Engaging community stakeholders, such as healthcare providers, educators, and local leaders, is crucial in dispelling myths and promoting accurate information about the HPV vaccine.[30] Effective training of healthcare workers to advocate for vaccination can also play a pivotal role in countering misinformation and encouraging uptake.[21]
In addition, systemic healthcare challenges, such as inadequate outreach mechanisms and gaps in school-based programs, were noted as barriers. For instance, current school-based initiatives often fail to reach out-of-school girls, highlighting the need for more inclusive delivery systems.[15]
Addressing the barriers to HPV vaccination in India requires a coordinated, multifaceted strategy that integrates education, economic support, and community engagement. Efforts must prioritize equitable vaccination strategies by addressing economic and sociocultural barriers, such as vaccine cost, misinformation, and cultural stigma. Subsidized vaccine programs, community-based educational interventions, and targeted efforts for underserved populations, including out-of-school girls, are critical for improving coverage. Expanding vaccination to include men can further reduce transmission and increase herd immunity. Strengthening healthcare provider training and their active involvement can enhance vaccine acceptance while integrating HPV vaccination into national immunization programs and aligning with global initiatives like the WHO’s 90/70/90 strategy can accelerate cervical cancer elimination.[12] Furthermore, expanding school-based programs to involve parents and community leaders can foster trust and sustainable vaccine uptake.
The findings are limited by heterogeneity across included studies, which precluded meta-analysis. Most studies focused on urban populations, potentially overlooking barriers unique to rural and tribal communities. In addition, reliance on self-reported data in several studies may introduce recall and social desirability biases.
Future studies should explore innovative delivery models for reaching marginalized populations, including mobile health units and digital campaigns. Longitudinal studies are needed to assess the long-term impact of educational interventions and policy changes. Research should also investigate the role of male vaccination in reducing HPV transmission and its broader societal acceptance.
CONCLUSION
This review highlights the need for comprehensive strategies to enhance HPV vaccination uptake in India. Economic challenges, cultural beliefs, and low awareness hinder progress, while educational interventions remain limited.
Expanding vaccination among young men and addressing through culturally tailored communication are crucial.
Policymakers must integrate HPV vaccination into public health programs and ensure affordability, particularly in rural areas.
A multifaceted approach – combining education, accessibility, and community involvement – is critical to increasing coverage and reducing cervical cancer burden. A coordinated, evidence-based national strategy aligned with global health frameworks is vital for sustainable progress.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Mucosal and cutaneous human papillomavirus infections and cancer biology. Front Oncol. 2019;9:355.
- [CrossRef] [PubMed] [Google Scholar]
- Sexually transmitted infections In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560808 [Last accessed on 2025 Jan 08]
- [Google Scholar]
- Worldwide burden of cancer attributable to HPV by site, country and HPV type. Int J Cancer. 2017;141:664-70.
- [CrossRef] [PubMed] [Google Scholar]
- Penises not required: A systematic review of the potential for human papillomavirus horizontal transmission that is non-sexual or does not include penile penetration. Sex Health. 2016;13:10-21.
- [CrossRef] [PubMed] [Google Scholar]
- Cervical cancer in low and middle-income countries. Oncol Lett. 2020;20:2058-74.
- [CrossRef] [PubMed] [Google Scholar]
- Global cancer observatory: Cancer today. 2024. Lyon, France: International Agency for Research on Cancer; Available from: https://gco.iarc.who.int/today [Last accessed on 2024 Dec 27]
- [Google Scholar]
- Cervical cancer in India and HPV vaccination. Indian J Med Paediatr Oncol. 2012;33:7-12.
- [CrossRef] [PubMed] [Google Scholar]
- HPV vaccination of girl child in India: Intervention for primary prevention of cervical cancer. Asian Pac J Cancer Prev. 2018;19:2357-8.
- [Google Scholar]
- Demand and willingness to pay for human papilloma virus vaccine for their daughters among mothers in Haryana, India: A contingent valuation study. J Health Serv Res Policy. 2024;29:76-83.
- [CrossRef] [PubMed] [Google Scholar]
- Urban-rural inequities in the parental attitudes and beliefs towards human papillomavirus infection, cervical cancer, and human papillomavirus vaccine in Mysore, India. J Pediatr Adolesc Gynecol. 2018;31:494-502.
- [CrossRef] [PubMed] [Google Scholar]
- Global strategy to accelerate the elimination of cervical cancer as a public health problem. 2020. Geneva: World Health Organization; Available from: https://www.who.int/publications-detail-redirect/9789240014107 [Last accessed on 2024 Dec 27]
- [Google Scholar]
- The impact of health education interventions on HPV vaccination uptake, awareness, and acceptance among people under 30 years old in India: A literature review with systematic search. Front Reprod Health. 2023;5:1151179.
- [CrossRef] [PubMed] [Google Scholar]
- Preparedness of young girls for prevention of cervical cancer and strategy to introduce the HPV vaccine. Indian J Community Med. 2018;43(Suppl 1):S38-41.
- [CrossRef] [PubMed] [Google Scholar]
- Designing a pro-equity HPV vaccine delivery program for girls who have dropped out of school: Community perspectives from Uttar Pradesh, India. Health Promot Pract. 2022;23:1039-49.
- [CrossRef] [PubMed] [Google Scholar]
- Human papillomavirus vaccine acceptance among young men in Bangalore, India. Int J Dermatol. 2014;53:e486-91.
- [CrossRef] [PubMed] [Google Scholar]
- Vaccine hesitancy in India: Facilitators and inhibitors. Health Educ Behav. 2023;50:822-34.
- [CrossRef] [PubMed] [Google Scholar]
- Knowledge, attitude towards human papillomavirus and HPV vaccine among female medical personnel of a tertiary care teaching hospital in India. Eur J Mol Clin Med. 2022;9:9.
- [Google Scholar]
- Knowledge, attitudes, practices, and sociocultural factors influencing cervical cancer screening and vaccination among women in rural communities of Gujarat: A mixed-methods study. J Family Med Prim Care. 2024;13:3988-94.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of high-risk HPV among marginalized urban women in India and its implications on vaccination: A cross sectional study. Int J Gynaecol Obstet. 2023;162:176-82.
- [CrossRef] [PubMed] [Google Scholar]
- Lessons learned from HPV vaccine delivery in low-resource settings and opportunities for HIV prevention, treatment, and care among adolescents. J Acquir Immune Defic Syndr. 2014;66(Suppl 2):S209-16.
- [CrossRef] [PubMed] [Google Scholar]
- Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015;13:141-6.
- [CrossRef] [PubMed] [Google Scholar]
- The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
- [CrossRef] [PubMed] [Google Scholar]
- Users' guides to the medical literature. I. How to get started. The evidence-based Medicine Working Group. JAMA. 1993;270:2093-5.
- [CrossRef] [PubMed] [Google Scholar]
- Improving reference prioritization with PICO recognition. BMC Med Inform Decis Mak. 2019;19:256.
- [CrossRef] [PubMed] [Google Scholar]
- Zotero [Computer software] 2006. Corporation for digital scholarship. Available from: https://zotero.org [Last accessed on 2024 Dec 27]
- [Google Scholar]
- Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ. 2009;339:b2535-5.
- [CrossRef] [PubMed] [Google Scholar]
- Knowledge, awareness and attitude on HPV, HPV vaccine and cervical cancer among the college students in India. PLoS One. 2016;11:e0166713.
- [CrossRef] [PubMed] [Google Scholar]
- Indian parents prefer vaccinating their daughters against HPV at older ages. Asian Pac J Cancer Prev. 2014;15:107-10.
- [CrossRef] [PubMed] [Google Scholar]
- Effectiveness of family-centred sexual health education and HPV self-sampling in promoting cervical cancer screening among hard-to-reach Indian women in rural and tribal areas: A community-based pilot study. BMC Public Health. 2023;23:671.
- [CrossRef] [PubMed] [Google Scholar]







