Translate this page into:
A giant retroperitoneal liposarcoma with hemoperitoneum: A rare tumor with unusual presentation
*Corresponding author: Purnima Tiwari, Department of Obstetrics and Gynaecology, All India Institute of Medical Sciences, Nagpur, Maharashtra, India. purnima_gupta30@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Mukherjee S, Bhartiya N, Tiwari P, Khurana U. A giant retroperitoneal liposarcoma with hemoperitoneum: A rare tumor with unusual presentation. Indian J Med Sci 2022;74:48-51.
Abstract
Retroperitoneal liposarcoma (RPLS) is a rare mesenchymal tumor which accounts for 0.02–0.7% of all malignancy. The presentations of these tumors are non-specific and early diagnosis is often missed. We are reporting a rare case of 17-year-old girl who came to us with complaints of abdominal distension and other non-specific symptoms but after few hours of admission, she had acute abdomen with hemodynamic instability. She underwent emergency laparotomy and found to have a giant 25 × 20 × 10 cm ruptured retroperitoneum tumor causing hemoperitoneum. The tumor involved left ovary and fallopian tube as well. Complete resection of tumor with left salpingooophorectomy was done. The patient was kept in intensive care unit and discharged in good health after 15 days. This presentation of RPLS has not been reported yet and may demand early diagnosis and management of these tumors. The histopathology revealed dedifferentiated liposarcoma with rhabdomyosarcomatous differentiation. The patient is completely fine at 16 months of follow-up while writing this report. Again, heterologous dedifferentiation of liposarcoma with spindle cell component is a rare morphologic spectrum. Liposarcomas can have various histologic types. In dedifferentiated types, the line of differentiation needs to be identified to decide further line of treatment. Therefore, thorough histopathological analysis and immunostaining is needed. Treatment includes complete surgical resection. Role of radiotherapy and chemotherapy is debatable and is still under trial. Dedifferentiated RPLS with rhabdomyosarcomatous differentiation is a rare tumor and its presentation as acute abdomen and hemoperitoneum has never been reported previously.
Keywords
Retroperitoneal
Liposarcoma
Hemoperitoneum
Dedifferentiated
Mesenchymal
INTRODUCTION
Retroperitoneal sarcomas are mesenchymal tumors accounting for 1–2% of all solid malignancies and 10–20% of all sarcomas. Retroperitoneal sarcoma can have various types, out of which liposarcoma (well differentiated and dedifferentiated) is the most common type (up to 45%) followed by leiomyosarcoma and malignant fibrous histiocytoma. Retroperitoneal liposarcomas (RPLS) generally occur between 40 and 60 years of age group, but these tumor can occur at any age.[1] These tumors are asymptomatic in initial stage and are usually diagnosed only when they become large enough to compress nearby structures and cause symptoms. The surgical resection is the primary modality of treatment. The role of chemotherapy and radiotherapy is still debatable.
The dedifferentiated liposarcomas (DDLS) need to be differentiated from other type of sarcomas for further management. However, many times these tumors do not show distinctive morphological features and to identify their line of differentiation, immunohistochemistry and molecular study play a pivotal role.
We are reporting a case of 17-year-old girl who had acute abdomen with hemoperitoneum which resulted in hemodynamic instability and underwent emergency laparotomy. Intraoperatively, a big retroperitoneal tumor was identified. Complete resection of the tumor was possible. The patient was transfused blood and blood products and was put on inotrope support in post-operative period. Finally, she was discharged from hospital in good health and after 16 months of follow-up, she was free from any recurrence/metastases. On histopathological examination, it was identified as heterologously DDLS with rhabdomyosarcomatous dedifferentiation. This case is unique as hemoperitoneum has never been reported as a presentation of DDLS. Furthermore, rhabdomyosarcomatous dedifferentiation has been reported in only few cases of RPLS in the past.
CASE REPORT
A 17-year-old unmarried young girl presented to us with complaint of pain abdomen for past 3 months. She was apparently healthy 3 months back, when she started having pain abdomen which was gradual in onset, progressive in nature and was not radiating to any other site. She did not have any history of vomiting/fever/weight loss/ burning micturition. The patient also felt heaviness in lower abdomen since past few days when she came to us in out-patient department. Her menstrual cycles were regular. Her past history and family history were unremarkable. On examination, she was thin built with body mass index of 16.6 kg/m2. Her blood pressure was 120/70 mmHg and pulse rate was 76 bpm. On per abdominal examination, abdomen was distended and an abdominopelvic mass corresponding to 30 weeks size was palpated. It was hard in consistency with irregular surface and its margins were not well defined. Abdomen was non-tender and there was no inguinal lymphadenopathy. The patient was admitted for evaluation and further management in view of suspicion of malignancy. She was advised blood investigations, radiological investigations, and tumor markers.
In investigations, her hemoglobin was 10.1 g/dl, total leukocyte count was 8000/mcL, and platelet count was 380 × 103/mcL. Her liver function test, kidney function test, and thyroid function test were within normal limits. Ultrasonography of abdomen and pelvis revealed normal size anteverted uterus with endometrial thickness 5.3 mm. A 23 × 15 × 12 cm right ovarian multicystic lesion containing thick and thin septations was seen, which was extending up to bilateral hypochondrium regions. Few of these cysts contained hemorrhagic content, while few had clear anechoic fluid. Left ovary showed a well-defined rounded 10 × 7 cm lesion containing thick septations and tiny mobile echoes. These findings were suggestive of bilateral complex ovarian masses. Rest of the scan of abdomen and pelvis was normal. Her computed tomography scan was booked for next day and reports of tumor markers were awaited. After few hours of admission, the patient started complaining of excessive pain in abdomen which was sudden onset, progressive in nature, and severe in intensity. Her general condition was deteriorating. She looked pale and dehydrated with pulse rate of 110 bpm and blood pressure of 90/40 mm Hg. On per abdominal examination, tenderness and guarding were present. Her hemoglobin was found to be 4.8 g/dl. She was started on intravenous fluids and taken up for emergency laparotomy under general anesthesia in view of acute abdomen with hemodynamic instability after arranging adequate blood/blood products and informed consent.
Intraoperatively, intraperitoneal hemorrhagic fluid (2 L) and clots (approximated volume 1 L) were present. A large mass (solid-cystic) of approximately 25 × 20 × 10 cm was seen, which was arising from retroperitoneum. Left ovary and left fallopian tube were inseparable from mass. The right-sided fallopian tubes, right ovary, and uterus were normal. The mass had active bleeding surfaces and also contained intracystic hemorrhage/clots. The tumor tissue was sent for imprint cytology and report showed benign possibly hemorrhagic cyst. Left salpingo-ophorectomy along with complete resection of mass from its origin was done. Abdominal exploration was done and no gross deposits or any sign of malignancy anywhere else were seen. However, omental biopsy was taken and thorough peritoneal washing done. Intraoperatively, 2 unit packed red blood cells and 4 unit fresh frozen plasma were transfused. Post-operatively, the patient was shifted to intensive care unit on ventilator and on inotropic support. Post-operatively, she received 2 more units of packed red blood cells. Her CA 125 levels were found to be raised to 81 U/ml (Normal range upto 46 U/ml); the other tumor markers, including alpha fetoprotein, lactate dehydrogenase, and beta HCG, were found to be in normal range. The patient was extubated on post-operative day 3 and discharged on day 15th in good health.
Histopathology report of the excised abdominal mass revealed liposarcoma with rhabdomyosarcomatous differentiation with spindle cell morphology [Figure 1]. Omental biopsy was negative for any sign of malignancy. Sections from ovary and fallopian tubes did not show any significant pathological changes. In immunohistochemistry, tumor cells were Vimentin and Desmin positive. During follow-up, the patient was called with bone scan and CECT both of which came out to be negative for any metastasis. In absence of any metastasis, she was kept on follow-ups every 3 months and is doing well at the last follow-up of 16 months.
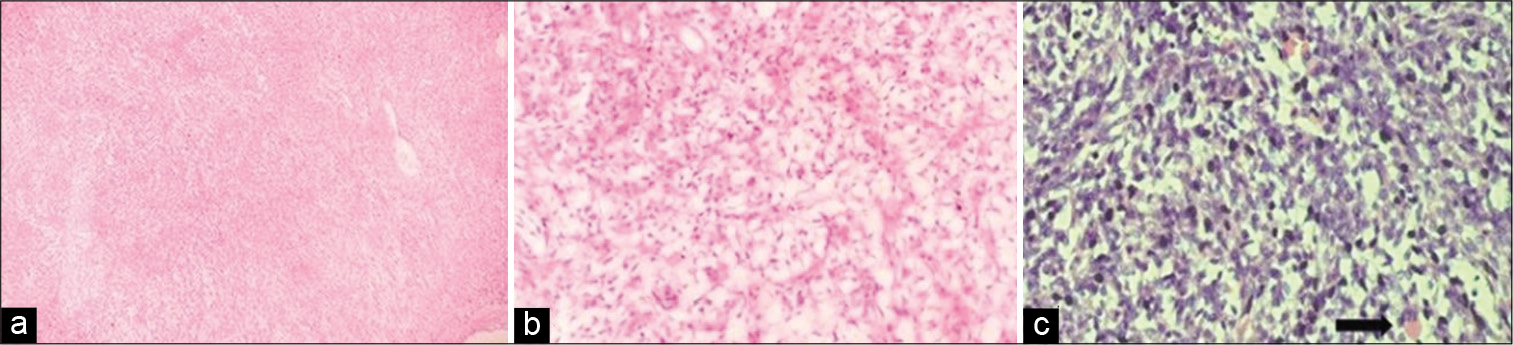
- (a) Scanner view showing cells arranged in fascicles and vague storiform pattern. (H and E; ×40), (b) High power view showing liopsarcomatous areas. (H and E; ×100); (c) Occasional rhabdomyoblast seen. (Arrow pointing in H and E; ×100).
DISCUSSION
Liposarcomas account for 10–20% of all soft tissue sarcomas. They can arise anywhere in the body from fat tissues which are present in soft tissues of body. The most common sites are extremities and retroperitoneum. They are divided into five subtypes – well differentiated, dedifferentiated, myxoid, round cell, and pleomorphic type based on the histology.[2] Retroperitoneal sarcomas are rare malignant tumors, accounting for 0.07–0.2% of all neoplasms. Retroperitoneal sarcomas generally present as vague abdominal mass, pain, or heaviness in abdomen. Larger tumors compress adjacent structures and cause neurological, vascular, and obstructive symptoms. Our patient with RPLS had rupture of the giant tumoral mass resulting in hemoperitoneum. To the best of our knowledge, this presentation of RPLS has never been reported in the literature, though Choi et al. have reported a case of primary colonic liposarcoma presenting as hemoperitoneum.[3]
The CECT is the investigation of choice for such tumors with ultrasound being the primary radiological investigation. However, in current case, ultrasonography was suggestive of the left ovarian mass. Similar to this, Aji et al. also reported a case where RPLS was mimicking an ovarian tumor pre-operatively.[4] This indicates that these tumors can masquerade as other pelvic tumors, especially ovarian tumor as well.
DDLS is an atypical lipomatous tumor, which is well differentiated land shows progression to sarcoma of various histologic grade (usually non-lipogenic). The diagnosis of DDLS is based on histopathology, immunohistochemistry, and molecular study. On histopathology, the dedifferentiation often resembles undifferentiated pleomorphic sarcoma/ myxofibrosarcoma. Rarely, heterologous dedifferentiation resemble rhabdomyosarcoma, leiomyosarcoma, osteomyosarcoma, or angiomyosarcoma. Only few cases of DDLS with rhabdomyosarcamatous dedifferentiation have been reported in the literature till date.[5] As already explained, our case also had spindle cell differentiation in liposarcomatous areas. It is important to differentiate DDLS with rhabdosarcomatous dedifferentiation from rhabdomyosarcoma to further prognosticate and decide course of management. Therefore, adequate specimen processing and IHC are the key to separate both entity. In DDLS, desmin and MyoD1 positivity and focal myogenin reactivity indicates areas of rhabdomyosarcomatous dedifferentiation. Desmin positivity was seen in the present case on IHC. Furthermore, immunostaining for MDM2, CDK4, and p16 along with MDM2 gene amplification is almost definitive for DDLS.[6]
The mainstay of treatment for RPLS is complete surgical resection which might be difficult due to big size and involvement of adjacent structures.[7] Its complete resection may increase the 5-year survival from 16.7% to 58%. Adjuvant radiation therapy/post-operative radiotherapy has been shown to improve overall survival and local recurrence rate in patients than surgery alone.[8-10] Pre-operative radiotherapy also provides advantage of less tumor seeding intra-operatively and need of lesser doses. Therefore, European Organization for Research and Treatment of Cancer is currently conducting a randomized controlled trial for comparison of pre-operative radiotherapy and surgery to surgery alone. In systemic therapies, doxorubicin/ifosfamide and docetaxel/gemcitabine are used for metastatic disease. Newer agents such as trebectedine and eribuline have been recently approved for advanced liposarcomas. DDLS are comparatively chemoresistant and therefore, specific targeted therapy, including Parbociclib (CDK4 inhibitor) and RG7112 (MDM2 antagonist), has shown activity, but further research is needed. In our case, pre-operative radiation therapy could not be given and in the post-operative phase, the patient denied any form of further treatment.[8] However, the patient had good results with surgery, alone with good clinical outcome without any local recurrence or metastasis at the last follow-up.
CONCLUSION
RPLS are rare tumors and may have various presentations but rupture of tumor with hemoperitoneum is a rare phenomenon and warrant earliest diagnosis and management of such cases. Furthermore, DDLS with rhabdomyosarcomatous dedifferentiation is a rare entity and should be differentiated with rhabdomyosarcoma to prognosticate and to decide further course of management. Complete surgical resection is the key for adequate treatment.
Acknowledgment
Nil.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Available from: https://www.sarcomahelp.org [Last accessed on 2020 Nov 29]
- Primary liposarcoma of the ascending colon: A rare case of mixed type presenting as hemoperitoneum combined with other type of retroperitoneal liposarcoma. BMC Cancer. 2010;10:239.
- [CrossRef] [PubMed] [Google Scholar]
- Giant retroperitoneal liposarcoma mimicking ovarian tumour-a case report. J West Afr Coll Surg. 2011;1:105-11.
- [Google Scholar]
- Dedifferentiated liposarcoma with heterologous spindle cell rhabdomyoblastic de-differentiation: An unusual pattern expanding the morphological spectrum. Indian J Pathol Microbiol. 2020;63:630-3.
- [CrossRef] [PubMed] [Google Scholar]
- Retroperitoneal sarcomas: An update on the diagnostic pathology approach. Diagnostics (Basel). 2020;10:642.
- [CrossRef] [PubMed] [Google Scholar]
- En bloc resection of a giant retroperitoneal liposarcoma: A surgical challenge. Cureus. 2020;12:e8730.
- [CrossRef] [Google Scholar]
- Recent advances in the management of liposarcoma. F1000Res. 2016;5:2907.
- [CrossRef] [PubMed] [Google Scholar]
- Preoperative radiotherapy in the management of retroperitoneal liposarcoma. Br J Surg. 2016;103:1839-46.
- [CrossRef] [PubMed] [Google Scholar]
- Prognostic factors in retroperitoneal sarcoma: A multivariate analysis of a series of 165 patients of the French Cancer Center Federation Sarcoma Group. Cancer. 2001;92:359-68.
- [CrossRef] [Google Scholar]






