Translate this page into:
A study to compare the role of various antibiotics in reducing the mortality and morbidity among patients with leptospirosis
*Corresponding author: Pramod Thomas, Department of Community Medicine, Biostatistics, Believers Church Medical College, Thiruvalla, Kerala, India. pramodbiostat@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Varughese M, Anjali R, Mohan CA, Thomas P. A study to compare the role of various antibiotics in reducing the mortality and morbidity among patients with leptospirosis. Indian J Med Sci. doi: 10.25259/IJMS_177_2024
Abstract
Objectives
To evaluate the effect of various antibiotics in reducing the mortality and early recovery from leptospirosis.
Materials and Methods
The present retrospective cohort study was conducted at the Believers Church Medical College Hospital with the prior approval of the Ethical Committee. The study duration was 6 months. Leptospirosis participants treated with bacteriostatic, bactericidal, or a combination of both bacteriostatic and bactericidal were included in the study. Data from January 2015 to June 2021 were extracted from the hospital records of Believers church medical college. Mortality and other various morbidity measures were analyzed and compared across various antibiotics.
Results
We collected 162 clinically suspected, laboratory-confirmed leptospirosis patient records. Hastened improvement was observed among patients with bacteriostatic agents rather than bactericidal agents. Bacteriostatic drugs performed better in “time to recovery” while comparing with bactericidal (P = 0.001) and a combination (bacteriostatic and bactericidal) (P = 0.006). The mortality rate was higher in bactericidal group than the other two groups.
Conclusion
In our study, recovery from leptospirosis is faster in patients treated with the bacteriostatic agents. The level of mortality was observed to be higher in patients treated with bactericidal but less in combination. Penicillin is the drug of choice in the early phase. Early diagnosis of leptospirosis is an essential but an unmet target for the better management of the illness. Bacteriostatic, irrespective of the cofactors present and delayed diagnosis is the better option to prevent mortality and faster recovery. Bacteriostatic, even in delayed diagnosed leptospirosis, irrespective of their comorbidity status, is a better option to prevent the mortality and faster recovery.
Keywords
Leptospirosis
Bactericidal
Bacteriostatic
Cytokine storms
Interleukin-6
Acute kidney injury
Delayed diagnosis
INTRODUCTION
Leptospirosis is a major, zoonotic disease commonly affecting people of developing countries in the tropical area.[1] The disease is caused by the spirochete of Leptospira genus exposure to urine of infected animals, commonly seen during rainy season.[2] Clinically, leptospirosis is diagnosed in its early stages with suspicion based on the patient’s risk factors, exposure history along with presenting signs and symptoms.[3] Pulmonary complications remain the major cause of mortality in those patients.[4] Worldwide, there were 1.03 million reported cases of leptospirosis and 58,900 deaths every year.[4] Due to the biphasic clinical presentation of leptospirosis, the optimal treatment is debatable.[5]
There are no specific evidence-based studies on the formulation of antibiotic policy in mortality reduction of leptospirosis cases.[6] Furthermore, there is a lack of controlled trials of penicillin against doxycycline for the treatment of leptospirosis.[6,7] Penicillin is a drug of choice for leptospirosis,[8] which is associated with Jarisch–Herxheimer Reaction, a well-known complication [Figure 1].[9]
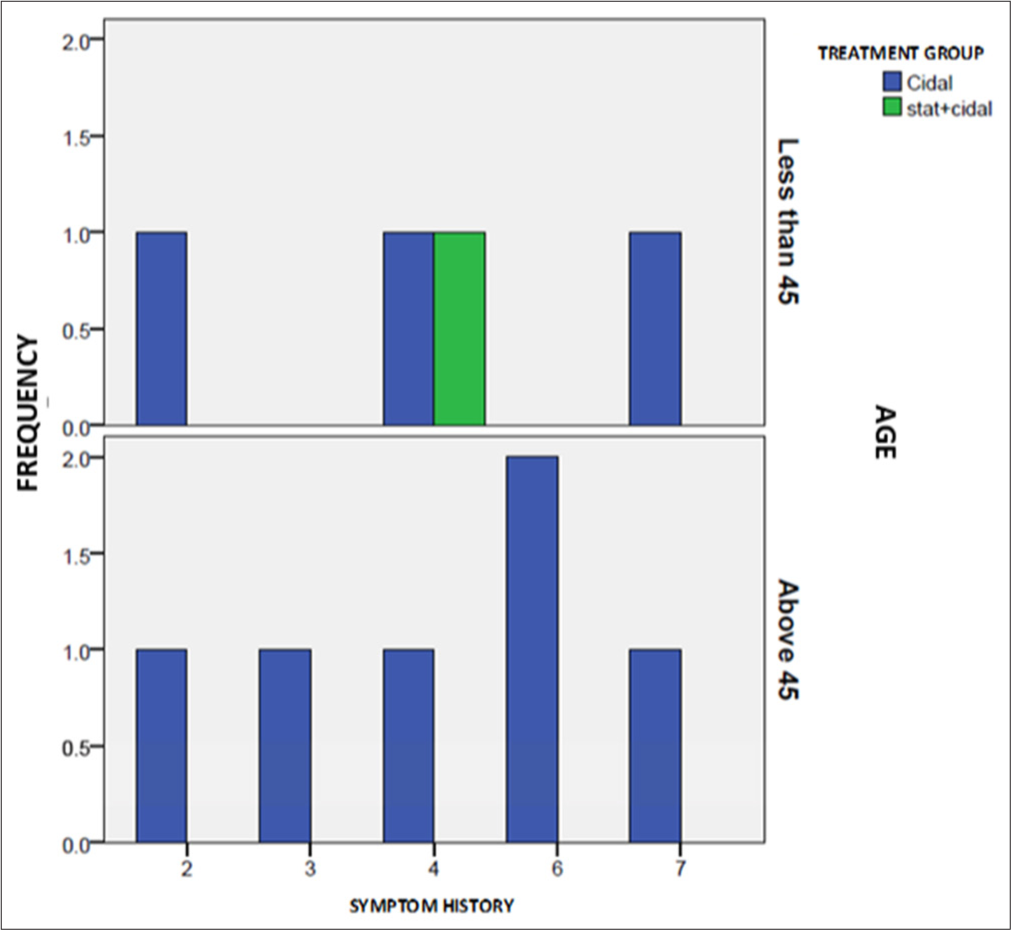
- Participants died during their hospital stay according to the age, type of antibiotic (bacteriostatic*, bactericidal, combination of both), duration of hospital stay (number of days participant survived since the antibiotic initiated), and number of days participant survived since the symptom first appeared. *No Deaths reported on Bacteriostatic group.
Many studies debated the role of antibiotics in the treatment of leptospirosis.[8] Costa et al. reported that the penicillin-treated participant’s mortality with leptospirosis was twice than that of the controls.[7] Among the severe or delayed for more than 4 days of window period, initiation of penicillin was not effective.[7] Even though there are many published studies reporting the advantages of bacteriostatic agents in the clinical management of infectious diseases,[7] less studies reported the advantages of bacteriostatic over bactericidal in the clinical management of leptospirosis, especially in reducing the mortality.[6,10]
The present study evaluated the mortality and morbidity of leptospirosis patients and assessed the efficacy of bacteriostatic agents on mortality reduction in leptospirosis patients over bactericidal or a combination of bactericidal and bacteriostatic drugs.
MATERIALS AND METHODS
The present retrospective cohort study conducted at a tertiary care hospital, under the Department of General Medicine, Believers Church Medical College, Thiruvalla, in South India. Prior ethical permission has been obtained from the Institutional Ethical Committee (IEC/2020/08/227). A total of 162 participant’s records, between January 2015 and June 2021, were extracted from the hospital medical records according to the inclusion and exclusion criteria. Doxycycline was administered as a bacteriostatic drug while ceftriaxone, piperacillin etc., were used as bacteriocidal drugs.
Inclusion criteria
Patient’s with classical signs and symptoms of leptospirosis and Leptospira enzyme-linked immunosorbent assay immunoglobulin M antibody positivity were identified and enrolled (available completed records between January 2015 and June 2021) and their hospital records were extracted.
Data were collected using a structured questionnaire. Variables include demographic profiles (age and gender), clinical variables such as comorbidities (diabetes mellitus, chronic kidney disease, chronic liver disease [CLD], coronary artery disease, and hypertension [HTN]), duration of symptoms, previous hospital visits or admissions and date of admissions, history of antibiotics (dosage, route of administration, frequency and duration), and outcome variable (survival status). Patients were managed either with bacteriostatic, bacteriocidal, or any of these drug combinations.
Data collection and analysis
All the patients who satisfied the inclusion criteria were enrolled. Patients were assessed based on total duration of symptoms irrespective of the day he or she visited our hospital. In case of referral patients, the first drug administered (bactericidal, bacteriostatic, combination [bacteriostatic and bactericidal]) was considered. Further, post-leptospirosis variables hypotension, liver enzymes, creatinine, blood urea, and temperature were also recorded. The required data were retrieved and entered into the pre-designed data collection proforma in Microsoft excel-2010 and analyzed. In addition, the Statistical Package for the Social Sciences 21 was used for statistical analysis.
RESULTS
Data obtained from 162 admitted leptospirosis cases (bacteriostatic [n = 59], bactericidal [n = 23], or combination of bacteriostatic and bactericidal drugs [n = 80]). Participant’s time to recovery or discharge (from admission), duration of illness (from symptoms appearance till discharge), body temperature, systolic and diastolic blood pressure, creatinine, serum glutamic oxaloacetic transaminase (SGOT), and serum glutamate pyruvate transaminase (SGPT) at the time of admission and discharge against the drug administered were analyzed.
Various parameters (temperature, blood pressure, creatinine, SGOT, and SGPT) obtained at the time of admission were compared against the type of antibiotic administered and found out to be non-significant (P > 0.05) as expected (data not shown).
We further evaluated the parameters (time to recovery, duration of illness, blood pressure, renal function tests, and liver function tests) at the time of discharge against the type of antibiotic [Table 1].
| Variable | Mean (SD) | F | Significant |
|---|---|---|---|
| *Time of recovery (days) | |||
| Bacteriostatic (n=59) | 4.18 (0.57) | 42.16 | 0.0001 |
| Bactericidal (n=14) | 6.64 (1.15) | ||
| Combination of both (n=79) | 4.89 (1.06) | ||
| *Duration of illness (days) | |||
| Bacteriostatic (n=59) | 8.34 (2.22) | 9.39 | 0.0001 |
| Bactericidal (n=14) | 10.79 (2.58) | ||
| Combination of both (n=79) | 9.18 (2.28) | ||
| Systolic 2 | |||
| Bacteriostatic | 78.64 (6.3) | 16.9 | 0.00001 |
| Bactericidal | 66.96 (14.3) | ||
| Combination of both | 77.5 (7.7) | ||
| Diastolic 2 | |||
| Bacteriostatic | 123.39 (8.4) | 10.49 | 0.00005 |
| Bactericidal | 110 (22.2) | ||
| Combination of both | 120.45 (9.9) | ||
| SGOT 2 | |||
| Bacteriostatic | 33.27 (13.5) | 17.37 | 0.00001 |
| Bactericidal | 74.83 (78.5) | ||
| Combination of both | 33.0 (11.8) | ||
| SGPT 2 | |||
| Bacteriostatic | 36.8 (16.6) | 14.67 | 0.00001 |
| Bactericidal | 85.48 (10.4) | ||
| Combination of both | 34.1 (14.0) | ||
| Creatinine 2 | |||
| Bacteriostatic | 1.047 (0.48) | 19.882 | 0.00001 |
| Bactericidal | 2.73 (3.04) | ||
| Combination of both | 1.025 (0.39) |
Multiple comparison analysis was performed (Bonferroni’s multiple comparison analysis) and observed that bacteriostatic was significantly superior in comparison with bactericidal in all parameters considered. Combination (bacteriostatic and bactericidal) was significantly better than bactericidal with all the parameters. In Table 2, we described the average values of each parameter (clinical and laboratory) among the total participants, those who survived and those who died against the type of antibiotic prescribed.
| Mean clinical and laboratory parameters | Survival | Dead | |||
|---|---|---|---|---|---|
| Bacteriostatic (n=59) | Combination of both (n=79) | Bactericidal (n=14) | Combination of both (n=1) | Bactericidal (n=9) | |
| Mean | Mean | Mean | Mean | Mean | |
| Systolic BP1* | 75.2 | 71.8 | 77.9 | 50 | 64.5 |
| Systolic BP2* | 78.6 | 78 | 76.4 | 40 | 52.2 |
| Diastolic BP1* | 116.5 | 115.7 | 122.9 | 70 | 100.8 |
| Diastolic BP2* | 123.3 | 121.1 | 126.4 | 70 | 84.5 |
| Creatinine 1 | 2.4 | 2.5 | 1.9 | 1.3 | 4.3 |
| Creatinine 2 | 1.0 | 0.99 | 0.79 | 3.2 | 5.75 |
| SGOT 1 | 71.7 | 75.6 | 64.1 | 197 | 80.4 |
| SGOT 2 | 33.2 | 32.8 | 30.4 | 49 | 144 |
| SGPT 1 | 76.0 | 72.7 | 67.7 | 55 | 85.6 |
| SGPT 2 | 36.8 | 34.2 | 32.4 | 26 | 168.1 |
| Time to recovery/death | 4.2 | 4.9 | 6.6 | 1.0 | 3.22 |
| Duration of illness | 8.3 | 9.5 | 10.7 | 5.0 | 7.7 |
We observed no death in bacteriostatic group, one death in combination and 9 deaths in bactericidal group [Table 2].
Systolic and diastolic blood pressures were lower and serum creatinine was higher among patients who died. SGOT and SGPT were significantly reduced among the survivors irrespective of their treatment group but that worsened among died in bactericidal group. Shorter hospitalization (time to recovery and duration of illness) was observed among bacteriostatic group [Table 2].
Comorbidities were more prevalent in the bacteriostatic group. No significant differences were observed between the baseline characteristics of bacteriostatic versus bactericidal and combination groups (data not shown). Mortality was marginally higher among patients with >45 year’s [Figure 1]. In bactericidal group, we observed less number of survivors among comorbid participants [Figure 2].
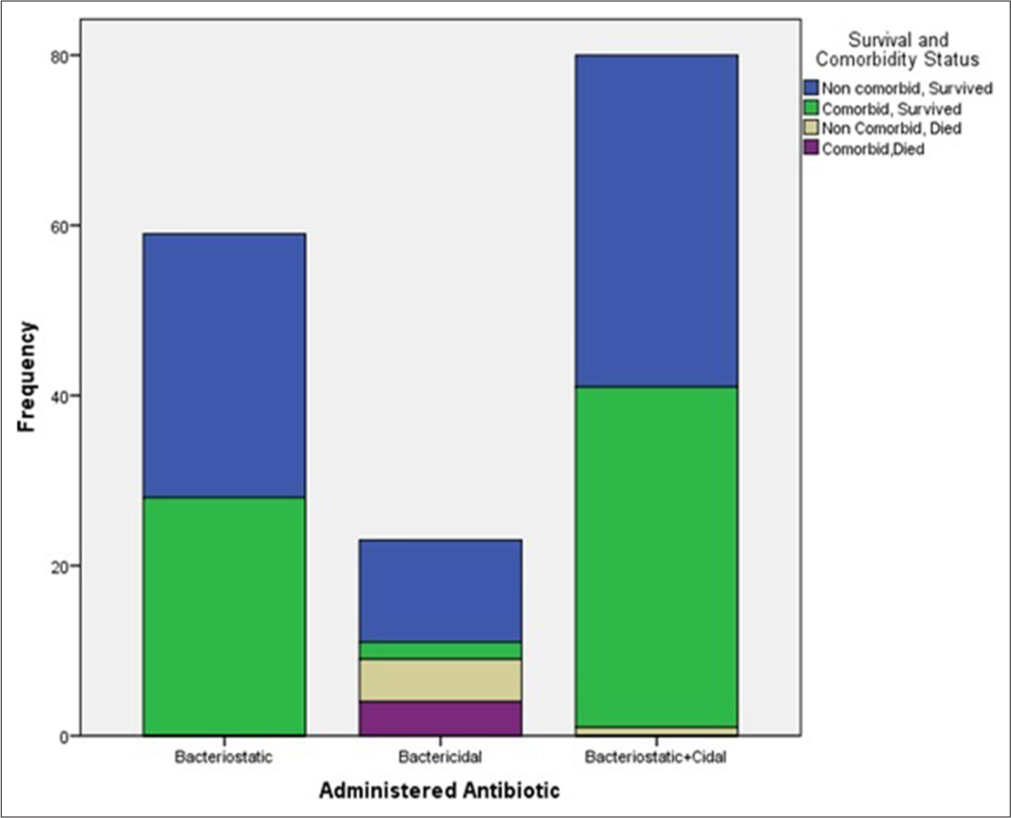
- Survival status of the participants according to their comorbidity status and type of antibiotic received.
Time to recovery from leptospirosis in patients treated with bactericidal agents and combination [Figure 3].
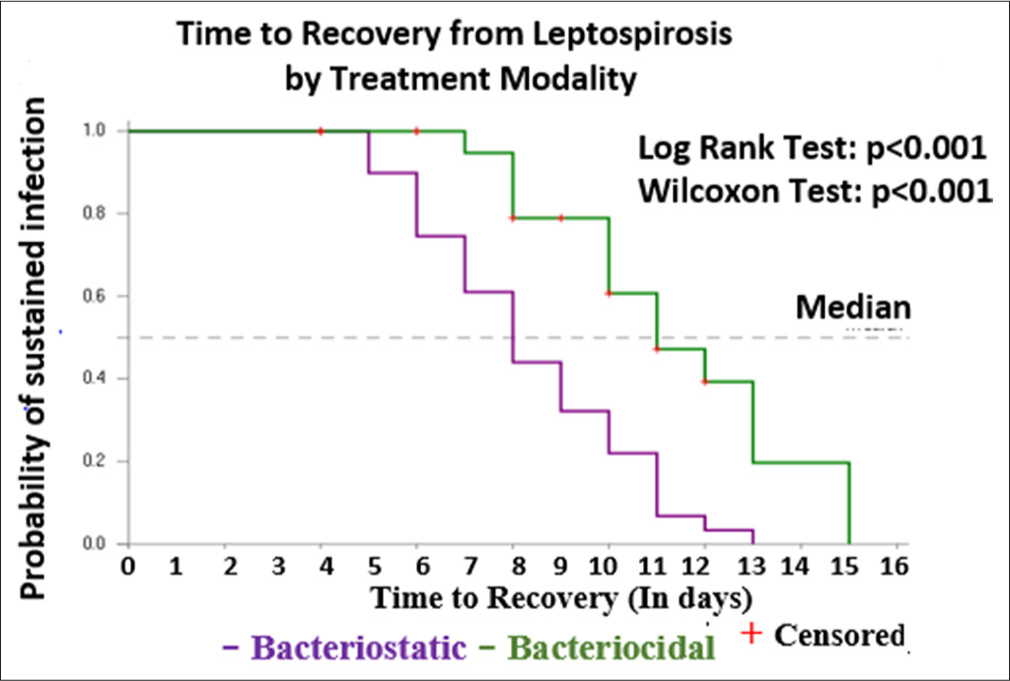
- Time to recovery (or mortality) from Leptospirosis in patients treated with bactericidal agents and combination of bacteriostatic and bactericidal.
Faster improvement was seen among patients treated with bacteriostatic drugs. Mortality rate was more observed in the bactericidal group.
DISCUSSION
Leptospirosis, with 1.03 million cases, 59000 deaths reported worldwide.[5] Bacteriostatic drug decreases the production of pro-inflammatory cytokines, in severe leptospiral infection along with the lungs, kidney, and liver involvement when compared to the patients without complications.[11]
Mortality increases with increased age, rising 3.7-fold for 40–49-year old to 7.3-fold among those 60 or older,[12] In our data, above 45 years, irrespective of their comorbidity status, higher mortality rate was observed among the participants treated with bactericidal drugs [Figures 1 and 2].[13]
Bactericidal antibiotics are better in destroying the actively dividing bacterial cells and are misinterpreted as more effective or superior than bacteriostatic antibiotics by clinicians.[14] However, even though the complete destruction of Leptospira happens, mortal remains produce pro-inflammatory cytokines such as interleukin-8, granulocyte-macrophage colony-stimulating factor, interleukin-6, matrix metalloproteinases, and tumor necrosis factor-α of the spirochetes produce cytokine storms leading to end-organ involvement. Bacteriostatic used in combination with bactericidal, resulted in the inhibition of growth and overall reduction of efficacy of bactericidal drugs (Ocampo et al., 2014).[15] The abovementioned principle worked while bacteriostatic decreased the production of pro-inflammatory cytokines which led to the reduction in mortality.[16]
Various types of antibiotics bactericidal and bacteriostatic are prescribed by clinicians for the treatment of leptospirosis. Both agents are characterized by rapid absorption, excellent tissue penetration, similar mechanisms of action (inhibition of protein synthesis), and similar peak serum concentrations at standard therapeutic dosing.[16] Before the laboratory diagnosis, empirical antibiotic treatment is commonly prescribed. Few studies reported bactericidal drugs as more potent compared to the bacteriostatic agents.[17] Costa et al. reported that case fatality was twice as higher among the delayed (more than 4 days) diagnosed leptospirosis cases than those with early (<4 days) diagnosed and those who treated with penicillin.[7] Azithromycin (bacteriostatic) shares many pharmacodynamic properties with doxycycline.[18] As an acute treatment for leptospirosis and a prophylactic agent, bacteriostatic is useful and provides a good survival rate. There are no controlled clinical trials on estimating the efficacy of penicillin or doxycycline in the treatment of leptospirosis or in comparing the mortality, hence the evidence is lacking to provide any clear guidelines for practice.[2]
Our study compared the efficacy of bacteriostatic and bactericidal drugs and the combination (bacteriostatic and bactericidal drugs) in various stages of leptospirosis, especially in preventing the mortality. We observed the mortality from early phase (4th day onwards) of the disease. Participants of bacteriostatic group even with comorbidities (acute liver and kidney injuries, CLD, coronary artery heart disease, and HTN) showed zero mortality and less complications.
In our study, bacteriostatic was significantly superior to bactericidal (P < 0.0001) and in combination (P = 0.006) (bacteriostatic and bactericidal drugs) in time to recovery and duration of illness [Table 1]. Similar 56 studies were reviewed by Wald-Dickler et al.[19] and only one study reportedly demonstrated the superiority of bactericidal over bacteriostatic, six studies documented the superiority of bacteriostatic over bacteriocidal.[19] We also observed that, combination performs significantly better than bactericidal with all the parameters. Even though the comorbidities were more observed among the participants in bacteriostatic group, no statistically significant differences were identified in baseline characteristics of the participants who received bacteriostatic, bactericidal, and combination (bacteriostatic and bactericidal of drugs).
Figure 3 shows the time to recovery (or mortality) from the onset of leptospirosis in patients treated with bacteriostatic and bactericidal drugs, faster improvement was seen in patients who were treated with bacteriostatic agents, and all the mortalities were observed in bactericidal group except one in the combination group. In a randomized, placebo-controlled, double-blinded study, doxycycline therapy was reportedly shortened the duration of illness due to the leptospirosis by 2 days and improved fever, malaise, headache, and myalgia.[3]
The bacteriostatic agent is reportedly superior in efficacy and cost-effective than the bactericidal agent.[19] We observed similar findings in the management of leptospirosis. Our clinical experience and present study also evidenced the same. Bacteriostatic, an antibiotic that achieves more than 1000-fold reduction in bacterial density and 8-fold above the minimum inhibitory concentration of the drug is considered to kill the bacteria[19] Even though the debate on the management of leptospirosis is continuing due to the biphasic clinical presentation of the illness, we observed that fatality and severity due to the complications can completely be avoided with the bacteriostatic drug initiation at the time of initial diagnosis or even in suspected cases.[2]
Limitations of the study
Major patient characteristics could not be assessed due to the retrospective study design
Pre-hospital antibiotic intake history could not be assessed.
CONCLUSION
Observed mortality among patients with leptospirosis was negligibly small among bacteriostatic and combination (bacteriostatic and bactericidal) groups. Bacteriostatic is useful even in patients presenting late and reportedly, and recovery is faster resulting in reduced mortality. Penicillin may be the drug of choice in early diagnosis, which rarely happens in the case of leptospirosis, the only empirical and prophylactic-safe option is doxycycline. Comorbidities are not influencing the outcome of leptospirosis with bacteriostatic agents, which markedly reduce the treatment expenses.
Ethical approval
The research/study approved by the Institutional Review Board at Believers Church Medical College, number IEC/2021/08/227, dated July 14, 2021.
Declaration of patient consent
Patient’s consent was not required as we used hospital records of the patients anonymously.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in writing or editing the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Report of the first meeting of the leptospirosis burden epidemiology reference group Geneva: WHO; 2010. p. :1-34.
- [Google Scholar]
- Leptospirosis in humans. Curr Top Microbiol Immunol. 2015;387:65-97.
- [CrossRef] [PubMed] [Google Scholar]
- Global morbidity and mortality of leptospirosis: A systematic review. PLoS Negl Trop Dis. 2015;9:e0003898.
- [CrossRef] [PubMed] [Google Scholar]
- Factors associated with severity and mortality in patients with confirmed leptospirosis at a regional hospital in Northern Taiwan. J Microbiol Immunol Infect. 2010;53:307-14.
- [CrossRef] [PubMed] [Google Scholar]
- Current evidence on the antimicrobial treatment and chemoprophylaxis of human leptospirosis: A meta-analysis. Pathogens. 2021;10:1125.
- [CrossRef] [PubMed] [Google Scholar]
- Penicillin at the late stage of leptospirosis: A randomized controlled trial. Rev Inst Med Trop Sao Paulo. 2003;45:141-5.
- [CrossRef] [PubMed] [Google Scholar]
- Ceftriaxone compared with sodium penicillin g for treatment of severe leptospirosis. Clin Infect Dis. 2003;36:1507-13.
- [CrossRef] [PubMed] [Google Scholar]
- Leptospirosis complicated by a Jarisch-Herxheimer reaction and adult respiratory distress syndrome: Case report. Clin Infect Dis. 1994;18:1004-6.
- [CrossRef] [PubMed] [Google Scholar]
- Assessing cost effectiveness of empirical and prophylactic therapy for managing leptospirosis outbreaks. Epidemiol Infect. 2009;137:1323-32.
- [CrossRef] [PubMed] [Google Scholar]
- Leptospirosis: Increasing importance in developing countries. Acta Trop. 2020;201:105183.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative study of the inhospital case-fatality rate of leptospirosis between pediatric and adult patients of different age groups. Rev Inst Med Trop Sao Paulo. 2004;46:19-24.
- [CrossRef] [PubMed] [Google Scholar]
- Cytokine response signatures in disease progression and development of severe clinical outcomes for leptospirosis. PLoS Negl Trop Dis. 2013;7:e2457.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of macrolides and telithromycin against leptospirosis in a hamster model. Antimicrob Agents Chemother. 2006;50:1989-92.
- [CrossRef] [PubMed] [Google Scholar]
- Antagonism between bacteriostatic and bactericidal antibiotics is prevalent. Antimicrob Agents Chemother. 2014;58:4573-82.
- [CrossRef] [PubMed] [Google Scholar]
- Azithromycin: Mechanisms of action and their relevance for clinical applications. Pharmacol Ther. 2014;143:225-45.
- [CrossRef] [PubMed] [Google Scholar]
- Disproportional exaggerated aspartate transaminase is a useful prognostic parameter in late leptospirosis. World J Gastroenterol. 2005;11:5553-6.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of timing and duration of azithromycin therapy of leptospirosis in a hamster model. J Antimicrob Chemother. 2007;59:148-51.
- [CrossRef] [PubMed] [Google Scholar]
- Busting the myth of “static vs cidal”: A systemic literature review. Clin Infect Dis. 2018;66:1470-4.
- [CrossRef] [PubMed] [Google Scholar]






