Translate this page into:
Barriers to national accreditation board for hospitals and healthcare provider accreditation in public tertiary hospitals: A comprehensive review
*Corresponding author: Narinder Kumar, Department of Hospital Administration, All India Institute of Medical Sciences, Rishikesh, Uttarakhand, India. narinder.aiims@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kumar N, Reddy AN, Ramya T, Rathod PK. Barriers to national accreditation board for hospitals and healthcare provider accreditation in public tertiary hospitals: A comprehensive review. Indian J Med Sci. 2025;77:62-7. doi: 10.25259/IJMS_258_2024
Abstract
In India, the National Accreditation Board for Hospitals and Healthcare Providers (NABH) has become a well-respected framework that’s helped raise standards in many hospitals. Both private and public hospitals are now looking to get NABH accreditation, but public hospitals face a few challenge because they often deal with larger patient numbers and have limited resources. Public hospitals, especially big ones that serve a mix of different communities, tend to struggle with things such as old infrastructure and strict regulations. This review goes into these challenges, looking at the main obstacles that public hospitals face when they try to meet NABH standards. It covers areas such as money issues, lack of staff, and inefficiencies that make the accreditation process tougher. The review also suggests a few strategies and policy ideas that could help public hospitals push through these problems, with the goal of improving patient care across the board. By focusing on these challenges, this review hopes to give some useful insights to hospital administrators, policymakers, and the accreditation bodies working to make NABH standards a bit easier to achieve for all hospitals in India.
Keywords
Healthcare quality standards
National accreditation board for hospitals and healthcare provider accreditation
Operational challenges in healthcare
Patient safety
Public hospitals
INTRODUCTION
The National Accreditation Board for Hospitals and Healthcare Providers (NABH) represents one of the most respected frameworks in India and has driven significant improvements in healthcare institutions across the country. While NABH accreditation is increasingly pursued by both private and public sector hospitals, it poses distinct challenges for public tertiary care hospitals due to their unique operational and resource constraints. These institutions, often under-resourced and catering to large, diverse populations, face multifaceted hurdles ranging from infrastructural limitations to regulatory compliance issues.
This review article explores these challenges, providing a comprehensive analysis of the common roadblocks encountered by public tertiary care hospitals in their pursuit of NABH standards. This review also intends to contribute valuable insights for hospital administrators, policymakers, and accreditation bodies striving to make NABH standards more accessible and achievable across India’s diverse healthcare landscape.
OVERVIEW OF NABH ACCREDITATION
The NABH is a constituent board of the Quality Council of India, established with the goal of promoting and regulating healthcare quality standards across hospitals and healthcare institutions in India. NABH accreditation serves as a comprehensive framework for assessing the quality of healthcare services, safety measures, and patient care protocols, making it an essential benchmark for hospitals aspiring to elevate their standards to match international healthcare norms.[1-3]
NABH accreditation is structured around 100 standards (Guidebook to NABH Accreditation Standards for Hospitals, 5th Edition), addressing various aspects of hospital operations, including patient safety, infection control, human resource management, and quality management systems.
These standards are periodically updated to reflect the latest healthcare advancements and best practices in patient care. Each of these standards is broken down into objective criteria that are evaluated during an extensive, multistage process, where hospitals are assessed for compliance, improvements, and corrective actions to ensure continual quality improvement.[4,5]
Accredited hospitals have shown improvements in clinical outcomes, patient satisfaction, and operational efficiencies, creating an environment of trust and safety for both patients and healthcare providers. The rigorous standards and continual assessments required for NABH accreditation, however, can be challenging for resource-constrained hospitals, especially in the public sector, which often struggle with limited financial resources and staffing.[6]
POSITIVE OUTCOMES ARE OBSERVED POST-ACCREDITATION TO NABH
Improved patient outcomes
NABH standards prioritize patient safety, clinical excellence, and evidence-based practices, all of which contribute to better health outcomes. Accredited public tertiary hospitals are required to implement standardized protocols for infection control, medication management, and emergency care, which can significantly reduce the risk of medical errors, healthcare-associated infections, and other adverse events. Studies indicate that accredited hospitals demonstrate lower mortality rates and higher levels of patient satisfaction, reflecting the effectiveness of these rigorous quality measures.[7,8]
Enhanced operational efficiency
Accredited hospitals are encouraged to implement systematic documentation, structured workflows, and continuous monitoring of key performance indicators. In public tertiary care hospitals, where limited resources and high patient volumes are common challenges, these efficiency gains are particularly beneficial. Improved operational efficiency through accreditation can result in faster patient processing times, reduced waiting periods, and optimized resource allocation, which ultimately improves service delivery and patient throughput.[9,10]
Increased staff satisfaction and professional development
Compliance with NABH standards involves regular training and upskilling of healthcare staff, enabling them to keep pace with evolving medical practices and safety protocols. This emphasis on training helps healthcare professionals gain confidence in their skills and improves morale by providing clear guidelines and expectations. Furthermore, accreditation supports a positive work environment by encouraging transparent communication, team collaboration, and staff involvement in quality improvement initiatives, all of which contribute to higher job satisfaction.[11,12]
Building a culture of accountability and quality
NABH accreditation establishes a framework for regular audits, performance evaluations, and continuous monitoring, which collectively foster an environment of accountability. By embedding accountability into daily operations, NABH standards encourage healthcare professionals to adhere to best practices consistently, leading to improved trust between patients and providers.[13]
Financial incentives through government initiatives
Examples include the Ayushman Bharat Pradhan Mantri Jan Arogya Yojana, which offers a Silver Certification for hospitals meeting NABH Entry Level standards, rewarding them with an increased percentage of financial incentives. A 10% incentive is being provided to the hospitals with entry-level NABH certification and 15% for NABH full accreditation over and above the base rate of health benefit packages (HBP) packaged master rates.[14]
UNIQUE CHALLENGES FACED BY PUBLIC TERTIARY CARE HOSPITALS AND THEIR WORKABLE SOLUTIONS
While NABH accreditation offers significant advantages, public tertiary care hospitals face numerous challenges in meeting its rigorous standards. These challenges stem from a combination of financial constraints, staffing limitations, infrastructure deficiencies, and administrative hurdles, all of which hinder their ability to achieve and maintain NABH accreditation. Following are the primary challenges encountered by public hospitals.
Procurement-related issues
-
Requirement to procure medicines and consumables from Jan Aushadhi, where “look-alike” drugs increase risk to patient safety. Ref: NABH Standard management of medication (MOM).3.e - High-risk medications including look-alike, sound-alike (LASA) medications and different concentrations of the same medication are stored physically apart from each other.[15]
Solution: Implement color-coding or labeling on LASA drugs to differentiate them and minimize confusion.
Near expiry policy: Near expiry policy cannot be maintained as Jan Aushadhi as the clause is not included in Memorandum of Understanding of many public hospitals with Jan Aushidhi. Ref: NABH Standard: MOM.6.c - Near-expiry medications are handled effectively.
-
Mandatory procurement from government e-marketplace, which can slow down purchasing processes.[16]
Solution: Propose a streamlined approval process for urgent procurements and create buffer stock for essential supplies.
-
Lengthy procurement processes that delay access to essential drugs and supplies.
Solution: Establish a dedicated procurement team to handle and expedite processes, especially for critical items.
-
Equipment maintenance challenges, especially with Annual Maintenance Contracts or Comprehensive Maintenance Contracts that are often delayed or lack sufficient coverage.
Solution: Monitor maintenance schedules closely and establish local vendor partnerships for faster support on equipment maintenance.
Infrastructure and facilities issues
-
Aging infrastructure that requires frequent repairs and upgrades, which can be costly and time-consuming.
Solution: Schedule phased renovations and prioritize essential areas such as emergency wards and intensive care units.
-
High patient footfall, leading to overcrowding and increased strain on facilities.
Solution: Reorganize layout and create temporary patient waiting areas or expand outpatient areas to manage patient flow.
-
Housekeeping challenges in maintaining cleanliness and infection control in high-traffic areas.
Solution: Implement a rotating housekeeping schedule, increase staff for peak hours, and invest in automated cleaning devices.
-
Time-consuming tendering processes for renovations or new construction, causing delays in critical upgrades.
Financial constraints
-
Delayed approvals from finance departments, which slows down funding for essential upgrades and maintenance.
Solution: Propose a streamlined budgeting and approval process for quality-related expenses and seek periodic allocations.
-
Limited budget allocations for quality improvements and NABH compliance requirements.
Solution: Apply for government grants, utilize public-private partnerships, and seek donor support for specific quality improvement projects.
-
Difficulty in reallocating funds or securing additional resources for emergency purchases or immediate improvements.
Cultural and organizational resistance
-
Resistance to adopting new standards or practices, with staff often preferring established routines.
Solution: Conduct awareness sessions on the benefits of NABH accreditation and provide incentives for staff to adopt new practices.
-
Hierarchical organizational structures that hinder effective communication and cross-departmental collaboration.
Solution: Establish cross-departmental teams to improve communication and foster a collaborative culture for quality improvement.
-
Limited motivation among staff to prioritize quality improvement efforts due to perceived increased workload.
Solution: Include NABH compliance in performance evaluations and recognize departments that show consistent adherence to standards.
-
Reluctance to accept accountability for process changes or errors, hindering continuous improvement initiatives.
Solution: Foster an environment of openness and accountability through regular feedback, peer reviews, and transparent reporting mechanisms.[21]
Policies and standard operating procedures (SOPs) implementation
-
Staff resistance to implementing new policies or SOPs, often due to lack of familiarity or perceived difficulty.
Solution: Conduct training on the importance of SOPs and integrate SOP compliance into routine performance reviews.
-
Challenges in enforcing compliance with new SOPs, such as infection control or documentation standards, which staff may not see as necessary.
Solution: Assign SOP champions in each department to ensure adherence and address any issues promptly.
-
Lack of awareness or training on the importance and benefits of SOPs, leading to inconsistent adherence.
Solution: Implement regular training sessions and provide accessible SOP manuals for all staff members.
-
Footfall in public hospitals is substantial, with patients often coming from lower socioeconomic backgrounds and having limited education levels. Maintaining proper sanitation, housekeeping, and adherence to SOPs related to hygiene presents a significant challenge.
Shortage of human resources
-
Shortage of qualified healthcare professionals, leading to overworked staff and reduced quality of care.
Solution: Offer competitive packages, provide career development opportunities, and prioritize recruitment of qualified healthcare staff.
-
Difficulty in recruiting and retaining skilled personnel due to budget constraints or competitive job markets.
Solution: Partner with medical schools to create a pipeline for new hires and offer retention incentives like training and career progression.
-
Insufficient training and professional development opportunities, resulting in skill gaps and limited staff competency in quality management practices.
Solution: Arrange skill development workshops focused on quality management and compliance with NABH standards.
-
High turnover rates, with experienced staff often leaving for better opportunities, creating a lack of continuity in care and quality improvement efforts.
Solution: Develop a robust onboarding program and assign mentors to ensure that new staff are quickly brought up to NABH compliance standards.
-
Outsourced staff in public hospitals face three main issues: High turnover, low motivation, and eligibility gaps.
Turnover: Frequent turnover among outsourced workers disrupts operations and leads to constant training needs, impacting service quality
Motivation: Limited career growth, lower wages, and less job security reduce motivation and commitment, affecting overall performance
Eligibility: Outsourced staff may lack essential certifications and training, which can lead to compliance issues with hospital standards.
DISCUSSION
Achieving NABH accreditation in public hospitals is pivotal yet challenging due to unique structural and resource constraints. Accreditation offers significant benefits, such as improved patient safety, enhanced operational efficiency, and a standardized approach to care, which collectively build public trust and elevate healthcare standards. However, public hospitals face hurdles, including financial constraints, procurement challenges, infrastructural limitations, and cultural resistance. Figure 1 summarizes all the factors contributing as barriers, presented in the form of a fishbone diagram.
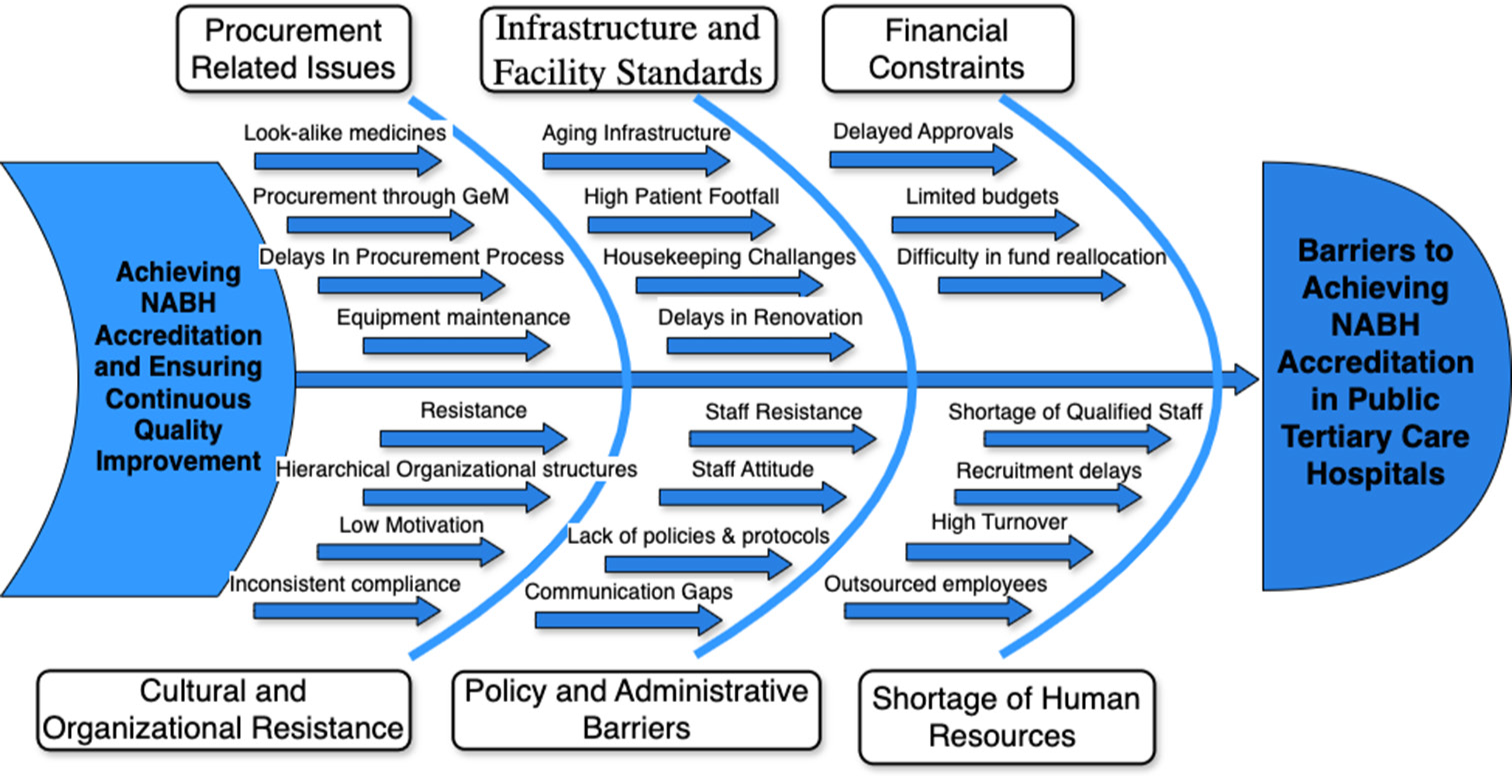
- Fishbone diagram showing the challenges of public hospitals. NABH: National accrediation board for hospitals and healthcare providers.
Financial issues, such as limited budgets and delayed approvals, often stall necessary upgrades and quality initiatives. Procurement processes, further hampered by mandatory sourcing requirements from platforms such as GeM and Jan Aushadhi, can delay access to critical supplies. Moreover, the lack of stringent hiring and training for outsourced staff compromises compliance with NABH standards, risking patient safety and operational continuity. In addition, cultural resistance to change, compounded by hierarchical organizational structures, restricts the adoption of new standards and hinders quality improvement.
Despite these barriers, feasible strategies, including public-private partnerships, focused training, and implementing Lean and Six Sigma methodologies, can help address these challenges. By aligning policy support, financial resources, and streamlined processes with NABH standards, public hospitals can better overcome barriers and deliver consistent, high-quality care.
CONCLUSION
It is a well-known fact that NABH accreditation elevates the healthcare quality and patient safety in both public as well private hospitals. Public tertiary hospitals face significant and unique challenges that can impede progress of accreditation. These range from infrastructure limitations and procurement hurdles to staffing shortages and resistance to organizational change. Addressing these barriers requires a multifaceted approach that includes policy reforms, capacity building, targeted financial support, and strategic partnerships. Emphasis must also be placed on sensitizing hospital staff, strengthening SOP implementation, and ensuring accountability mechanisms.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that they have used artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript or image creations.
Financial support and sponsorship: Nil.
References
- National Accreditation Board for Hospitals and Healthcare Providers. 2023. NABH standards. Available from: https://www.nabh.co [Last accessed on 2024 Oct 23]
- [Google Scholar]
- Quality Council of India. 2023. About NABH. Available from: https://www.nabh.co [Last accessed on 2024 Oct 23]
- [Google Scholar]
- Essentials of accreditation for tertiary care hospitals: NABH standards and procedures. J Hosp Adm. 2019;8:85-91.
- [Google Scholar]
- NABH standards (5th edition). 2020. Available from: https://www.nabh.co/standard.aspx [Last accessed on 2024 Oct 23]
- [Google Scholar]
- Implementation of NABH standards in hospitals: A strategic approach. Indian J Med Res. 2021;154:120-8.
- [Google Scholar]
- NABH in public sector hospitals: Financial and operational hurdles. Indian J Public Health Res Dev. 2021;12:308-12.
- [CrossRef] [Google Scholar]
- Quality healthcare and NABH accreditation: An overview for tertiary hospitals. Indian J Hosp Admin. 2021;9:125-31.
- [Google Scholar]
- Impact of accreditation on infection control in public hospitals. J Hosp Infect Control. 2020;34:89-96.
- [Google Scholar]
- Optimizing patient flow and reducing wait times with NABH protocols. Healthcare Policy Plan. 2021;36:215-22.
- [Google Scholar]
- Sustainability in resource-limited healthcare: NABH’s role in public hospitals. J Health Serv Res Policy. 2022;27:65-72.
- [Google Scholar]
- The role of accreditation in boosting staff morale and retention. Indian J Med Res. 2020;154:200-6.
- [Google Scholar]
- Training and development in NABH-accredited hospitals: Enhancing staff competence. J Health Manag. 2019;21:44-50.
- [Google Scholar]
- Staff satisfaction in NABH-compliant hospitals: Key findings and implications. Health Syst Reform. 2020;6:65-72.
- [Google Scholar]
- AB-PMJAY quality certification. Available from: https://pmjay.qcin.org/index [Last accessed on 2024 Oct 23]
- [Google Scholar]
- Procurement issues in public healthcare: Jan Aushadhi challenges. J Health Policy Econ. 2021;8:55-62.
- [Google Scholar]
- GeM procurement processes and efficiency challenges in public hospitals. Health Syst Reform. 2019;5:200-7.
- [Google Scholar]
- Infrastructure and equipment maintenance for quality compliance. Indian J Hosp Admin Res. 2021;6:77-85.
- [Google Scholar]
- Addressing infrastructural constraints in public tertiary hospitals. J Hosp Qual Manag. 2019;5:98-105.
- [Google Scholar]
- Housekeeping and infection control challenges in high-footfall facilities. Int J Health Policy Manag. 2021;10:145-50.
- [Google Scholar]
- Financial constraints in public healthcare accreditation. Asian Hosp Healthc Manag. 2020;7:89-94.
- [Google Scholar]
- Organizational resistance to change in healthcare. Indian J Med Ethics. 2019;15:78-83.
- [Google Scholar]
- SOP implementation challenges in tertiary care hospitals. Indian J Health Policy Res Dev. 2022;9:54-60.
- [Google Scholar]
- Policy enforcement and compliance issues in healthcare. Indian J Hosp Admin. 2019;8:122-30.
- [CrossRef] [Google Scholar]
- Human resource challenges in achieving healthcare accreditation. Asian J Health Manag. 2018;7:98-105.
- [Google Scholar]
- Impact of high turnover on outsourced healthcare staff. J Health Policy Manag. 2020;15:210-5.
- [Google Scholar]







