Translate this page into:
Co-infection with Mycobacterium and 20% acid-fast Nocardia in an immunocompetent patient – A case report
*Corresponding author: Vinita Rawat, Department of Microbiology, VCSG Government Institute of Medical Sciences and Research, Srinagar, Uttarakhand, India. drvinitarawat@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Singh A, Rawat V, Chaudhary P, Devrari JC. Co-infection with Mycobacterium and 20% acid-fast Nocardia in an immunocompetent patient – A case report. Indian J Med Sci. doi: 10.25259/IJMS_162_2024
Abstract
Nocardiosis is an opportunistic infectious disease in immunocompromised individuals, which may be fatal and in people with healthy immune systems, which is reported as a case. Mixed infections with Nocardia and Mycobacterium tuberculosis complex (MTBC) are rare. We are reporting a case of co-infection with Nocardia spp. and MTBC in an immunocompetent patient presenting with neck swelling. Interestingly, in this case, the primary identification of Nocardia was done using 20% H2SO4 as decolorizer for Ziehl–Neelsen staining. The patient was given first-line anti-tubercular treatment for the first 2 months as an intensive phase, followed by isoniazid and rifampicin for an additional 4 months, with a total of 6 months treatment, along with linezolid (600 mg twice daily for 15 days). The patient subsequently improved.
Keywords
Nocardia spp
Mycobacterium tuberculosis complex
Mixed infection
INTRODUCTION
Cervical tubercular lymphadenitis is the commonest presentation of extrapulmonary tuberculosis, it may be manifestation of a systemic tuberculous disease or a unique clinical entity localized to neck.[1] Nocardiosis is an opportunistic infectious disease in immunocompromised individuals, infection mainly occur either due to inhalation or by direct inoculation into the skin.[2] Mixed infections with Nocardia and Mycobacterium tuberculosis complex (MTBC) are rare.[3] When patients are co-infected with two organisms, rapid and accurate identification of two pathogens is crucial for patient management. We are reporting a case of co-infection with Nocardia spp. and MTBC in an immunocompetent patient presenting with neck swelling.
CASE REPORT
A 22-year-old male, farmer by occupation, visited to out-patient department with chief complaint of swelling on neck since past 1 month. There was no history of tuberculosis or trauma. Local examination revealed firm and non-tender swelling on the left supraclavicular region [Figure 1]. Laboratory report showed slight anemia and elevated C-reactive protein (22 mg/L), rest parameters were within normal limit. Hepatitis B surface antigen and total anti HCV were non-reactive and human immunodeficiency virus infection was also ruled out.

- Right supraclavicular swelling.
His X-ray chest was found to be normal. Fine-needle aspiration cytology (FNAC) report showed infective pathology, with no granuloma. Microbiological examination was not performed at the first hospital visit due to unknown reasons. Tablet amoxycillin-clavulanic (650 mg BD × 5 days) was prescribed and the patient was asked to report after 5 days of treatment. However, there was no relief, and the swelling became tender, soft, and erythematous. Aspiration of the swelling was performed and pus was sent to microbiology laboratory for Ziehl–Neelsen (ZN) staining, Gram staining, and culture sensitivity. A repeat FNAC was also sent to pathology department. Empiric therapy with injection ceftriaxone was started, Gram stained smear revealed Gram-positive, thin branching; filamentous bacteria suggestive of Nocardia. On ZN staining, two types of organism were seen – thin branching acid-fast bacteria suggestive of Nocardia and slender beaded acid-fast bacilli suggestive of Mycobacterium [Figure 2]. M. tuberculosis infection was, further, confirmed by True Nat. Repeat FNAC revealed granulomatous lesions with presence of acid-fast bacilli.
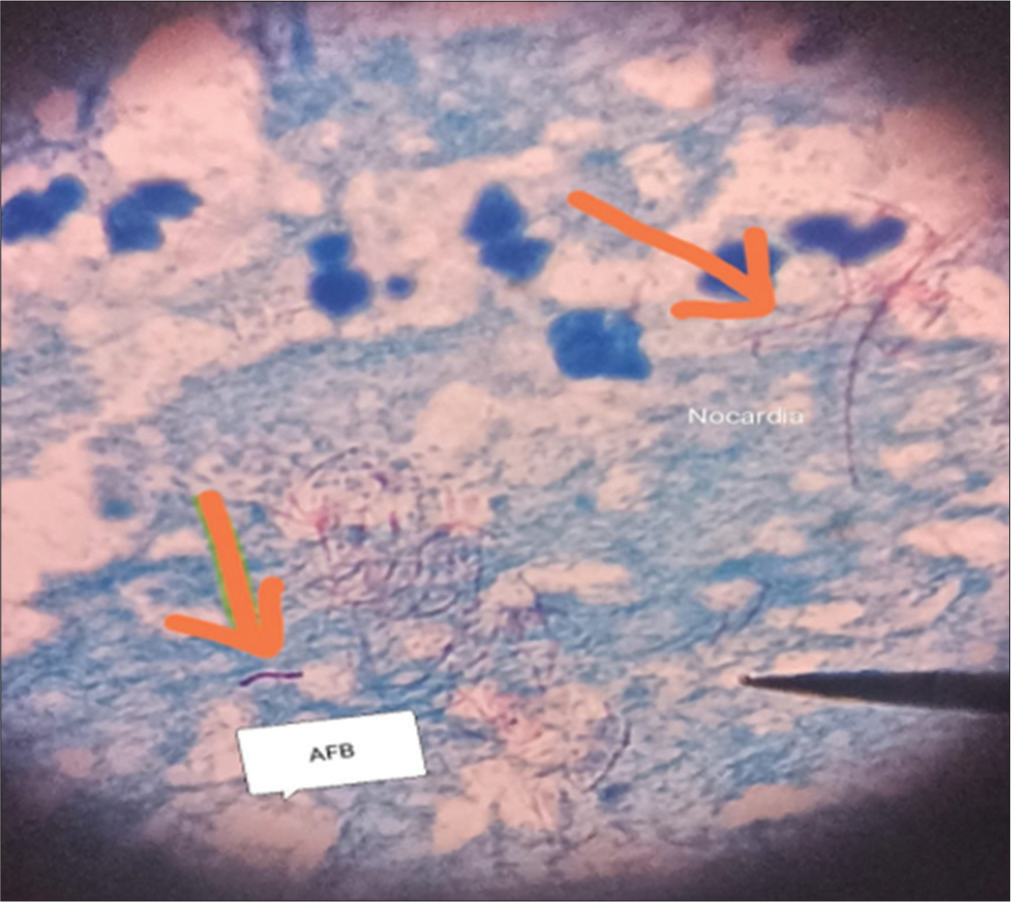
- Ziehl-Neelsen stained smear showing Mycobacterium spp. and thin branching acid- fast bacteria (Nocardia spp.).
Aerobic culture was done on blood agar and MacConkey agar and plates were incubated at 37°C till 3 weeks but no growth was observed.
The diagnosis was made as tuberculous lymphadenitis co-infected with Nocardia spp. and the patient was started on first-line anti-tubercular treatment for the first 2 months as an intensive phase, along with linezolid (600 mg twice daily for 15 days), followed by isoniazid and rifampicin for an additional 4 months, with a total of 6 months treatment.
The patient reported after 2 months of treatment, and there was significant improvement. The patient hailed from interior of Garhwal and expressed his inability to come for frequent follow-up so he was followed telephonically and was also advised to visit nearby primary health center for further follow-up. The patient was being followed up at a primary health center in his village and has recovered.
DISCUSSION
Nocardia spp. is ubiquitous in nature, infection mainly occurs either due to inhalation or by direct inoculation in the skin.[2] They are Gram-positive filamentous bacilli, characterized by aerobic growth. It has long culture cycle; hence, longer incubation is required before discarding culture plate as negative. Since it is difficult to diagnose, and more likely to be neglected in healthy young people.[2] TB lymphadenitis is the most frequent extrapulmonary manifestation of tuberculosis infection. Cervical lymphadenitis, which is also referred to as scrofula, may be manifestation of a systemic tuberculous disease or a unique clinical entity localized to neck.[1] This condition is commonly caused by MTBC as also seen in our case.
Mixed infections with Nocardia and MTBC are rare in immunocompetent person.[3] Our patient, farmer by occupation, may have been exposed to minor trauma with decaying plant matter that he could not recall.
The rarity of co-infections leads to the possibility that the discovery of one pathogen may lower the suspicion of the presence of other pathogens. In our case, we performed the ZN stain using 20% H2SO4 as a decolorizer. In this acid concentration, most of the nocardial infections go unreported, since Nocardia generally appears as acid-fast only when it is decolorized with 1% H2SO4.
Interestingly, in this case, the primary identification of Nocardia spp. was done using 20% H2SO4 as decolorizer. Earlier also in 2011 authors had isolated 20% acid-fast Nocardia brasiliensis from sputum.[4] A study from Jamia Hamdard, New Delhi, reported two cases of nocardiosis from pulmonary and extrapulmonary sites caused by N. asteroides and N. brasiliensis, respectively. Both of these Nocardia isolates were 20% acid-fast.[5]
These findings indicated the need of a more detailed study on the staining character of the Nocardia species.
CONCLUSION
Co-infection with Nocardia is never suspected unless and until there is high index of suspicion. The presence of tuberculosis does not necessarily rule out other infections. Morphological features on microscopic examination may provide additional information with potential clinical relevance and can be suggestive enough to warrant empiric therapy for nocardiosis while awaiting culture result. Laboratory specialists should be aware of occasional rare strain of 20% acid-fast Nocardia spp.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Diagnostic challenges in cervical tuberculous lymphadenitis: A review. North Clin Istanb. 2016;28:150-5.
- [CrossRef] [Google Scholar]
- Updated review on Nocardia species: 2006-2021. Clin Microbiol Rev. 2022;35:e0002721.
- [CrossRef] [Google Scholar]
- Co-infection with Mycobacterium tuberculosis and Nocardia farcinica in a COPD patient: A case report. BMC Pulm Med. 2023;23:136.
- [CrossRef] [Google Scholar]
- Primary pulmonary infection caused by 20% acid fast Nocardia brasiliensis. Indian J Med Microbiol. 2011;29:446-7.
- [CrossRef] [Google Scholar]
- The incidence of nocardiosis at pulmonary and extra-pulmonary sites. J Clin Diagn Res. 2013;7:1427-9.
- [CrossRef] [Google Scholar]






