Translate this page into:
Compliance on the use of water-soluble contrast agent in adhesional small bowel obstruction
*Corresponding author: Edmund Leung, Department of Surgery, Taranaki Base Hospital, New Plymouth, New Zealand. ed.leung@doctors.org.uk
-
Received: ,
Accepted: ,
How to cite this article: Leung E, Toy I, King J, Ghani Z, Shah A. Compliance on the use of water-soluble contrast agent in adhesional small bowel obstruction. Indian J Med Sci 2023;75:53-8.
Abstract
Objectives:
Small bowel obstruction is associated with significant morbidity and mortality. This study aimed to map outcomes of patients admitted with adhesional small bowel obstruction (ASBO ) with a view evaluating the effectiveness of water-soluble contrast agents (WSCA).
Materials and Methods:
A retrospective review of all emergency admissions coded for operative and non-operative treatment of small bowel obstruction between January 2018 and June 2020. Electronic patient records were utilized to confirm cases of ASBO. Patient demographics, hospital administrative data, treatment and surgery-related data are collected.
Results:
A total of 110 patients were admitted with ASBO initiated with conservative management. Median time to computed tomography (CT) scan was 12 h (Range: 3–115 h). Oral contrast was administered in only 11%; of these, 58% (7/12) resolved spontaneously compared to 52% (51/98) in those without contrast. About 43% (47/110) of all patients necessitated surgical intervention. Median time from admission to surgery was 43.5 h (Range: 10– 288 h). There were one 30-day re-admissions in patients surgically managed compared to two in those conservatively managed.
Conclusion:
Early CT scan facilitates initiation of non-operative management in stable patients with ASBO. In this series, the scant use of WSCA despite international guidelines did not compromise patient outcomes or length of stay.
Keywords
Adhesion
Bowel obstruction
Computed tomography
Oral contrast
INTRODUCTION
Small bowel obstruction accounted for 12,000 emergency operations in England and Wales between 2015 and 2016.[1] Apart from causing abdominal pain and secondary infertility in women,[2] adhesional small bowel obstruction (ASBO) is a common acute complaint necessitating urgent surgical admission.[3,4] Furthermore, ASBO is directly responsible for recurrent hospital admissions in patients who have previously had abdominal and/or pelvic surgery.[2] Surgery for ASBO is associated with prolonged operative time, risk of iatrogenic bowel injury, and significant patient morbidity.[4]
Open lower abdominal surgery is associated with a high relative risk of adhesion-related problems postoperatively.[5] Increased use of minimally invasive techniques in major abdominal and pelvic surgery within the past two decades[6,7] has contributed to the improved adhesion prevention strategies.[2,5]
The important role of imaging, particularly contrast-enhanced computed tomography (CT), in the diagnosis and management of ASBO has been aided by rapid advancements in imaging technology.[8] CT has considerable accuracy in diagnosing small bowel obstruction and in predicting the need for surgical intervention.[9] However, it must be noted that the majority of studies included in the meta-analysis[10] were retrospective studies. Two prospective studies have also demonstrated CT to be highly sensitive in diagnosing or excluding intestinal ischemia in the context of acute small bowel obstruction.[9,11] Therefore, in patients with ASBO or suspected ASBO, early CT scanning has been recommended.[1]
The use of oral water-soluble contrast agents (WSCAs) aids in clinically distinguishing between a high-grade obstruction and a partial obstruction.[8] WSCA use is effective in predicting the need for surgery.[12] The appearance of contrast in the colon within 4 to 24 h after administration of WSCA has a high sensitivity and specificity in predicting the resolution of ASBO. Compared to conventional treatment, it is effective in reducing the need for surgery and shortening hospital stays.[13,14] A recent report recommended that WSCA should “be embedded in clinical management for both prognostic and therapeutic purposes” in those patients not requiring emergency surgery.[1]
The authors’ institution is an English district general hospital. The use of WSCA in ASBO is limited by unavailability due to out-of-hours protocol and discretion of the admitting surgeon on call. In light of recommendations in the literature,[7] the aims of this study were to: (i) map the outcomes of patients admitted with ASBO during the studied period, (ii) to assess whether the availability and use of WSCA impacted patient management and (iii) to develop a pathway for the management of patients admitted with ASBO.
MATERIALS AND METHODS
Patients were identified from coding data pertaining to discharge diagnoses and/or procedure codes incorporating “bowel obstruction,” “small bowel obstruction,” “adhesions,” “laparotomy,” “emergency surgery,” “adhesiolysis,” and “small bowel resection.” Patient data were retrospectively collected for all admissions between January 1, 2018, and June 30, 2020. The data consisted of details pertaining to the patient’s hospital admission (time of admission, mode of referral to surgery, and early warning score on arrival), patient demographic information (age, comorbidities, surgical history, and American Society of Anesthesiologists), and management of ASBO (conservative with or without WSCA, success or failure of non-operative management, findings, and outcomes of those undergoing surgical intervention).
Diagnosis and management plans were correlated by cross-checking the radiological investigations to ensure robustness in data collection regarding the use of WSCA at the time of CT imaging or after diagnosis. The institution’s preferred WSCA at the time of the study was Gastrograffin. Each patient’s hospital admission outcome was recorded with the assistance of the institution’s various electronic patient records, and 30-day re-admissions rates were also monitored. Statistical significance was considered if P < 0.05 when evaluated by analysis of variance one-way analysis.
RESULTS
A total of 110 patients were attributed to ASBO over the 18-month study period. The median age of all patients was 67 years (Range: 19–97 years). More than half of all patients were admitted out-of-hours (between 1730 h and 0800 h).
Following a diagnosis of ASBO, patients were treated in one of three standard ways: (i) trial of conservative management using nasogastric decompression and intravenous fluid replacement therapy without the use of WSCA, (ii) conservative management with the use of WSCA, and (iii) emergency surgical intervention in patients who failed trial of conservative management.
About 89% of all patients admitted with ASBO did not receive oral contrast. About 52% of patients admitted with ASBO resolved spontaneously, while 43% of all patients required surgery. WSCA was administered in only 11% (n = 12) of patients admitted with ASBO [Figure 1]. Of these, WSCA was therapeutic in seven patients (58%). Of the five patients that failed conservative management with WSCA, palliative care was initiated for one patient and the remaining four underwent operative management [Figure 1]. [Table 1] outlines the demographics of the studied patient population.
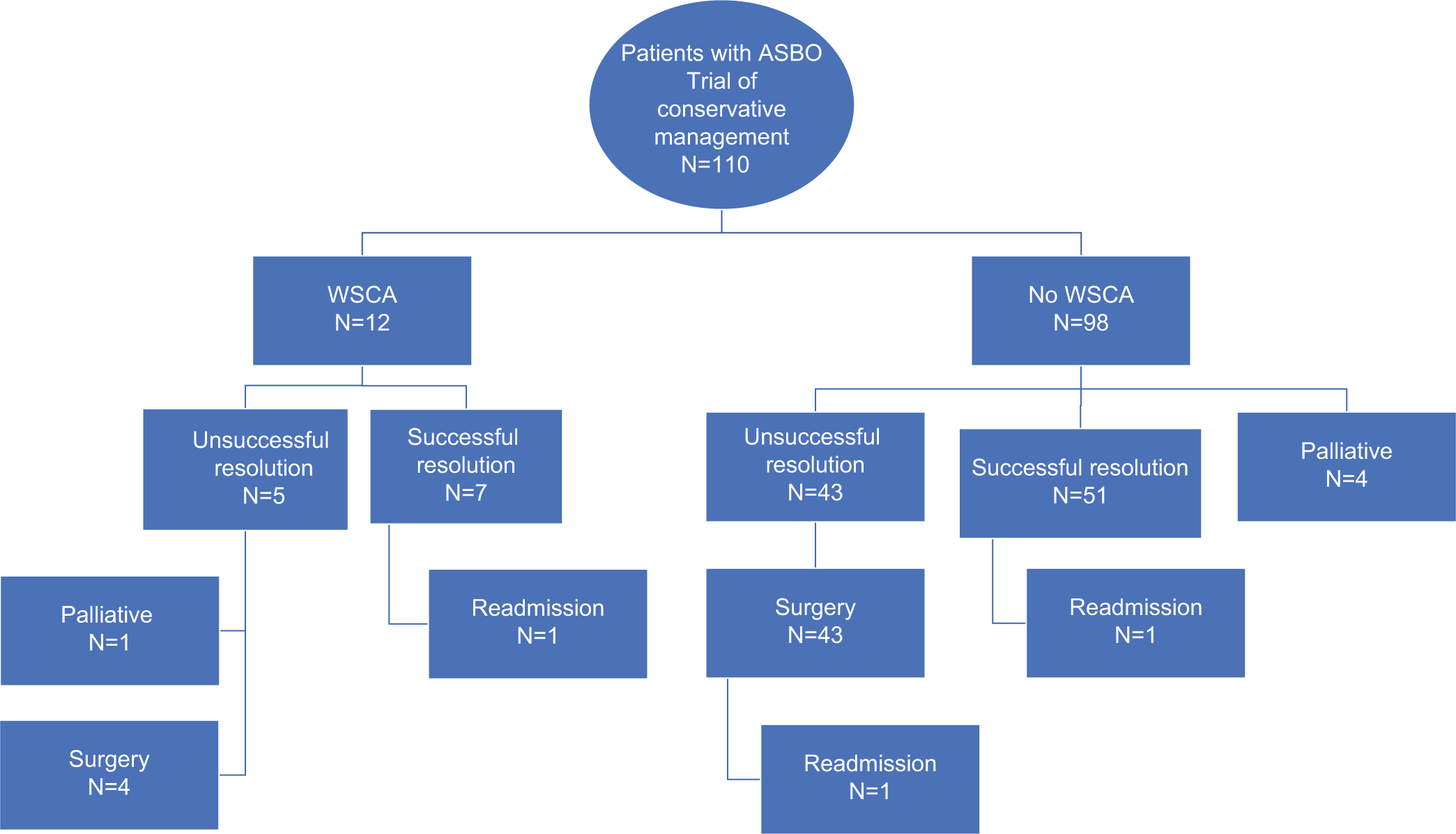
- Flowchart summary of the outcomes of all patients admitted with adhesional small bowel obstruction.
| Number of patients | ||
|---|---|---|
| All patients | 110 | |
| Successful conservative | 51 | |
| management without oral contrast | ||
| Successful conservative | 7 | |
| management with oral contrast | ||
| Patients requiring surgery following trial of | 47 | |
| conservative management | ||
| Palliation | 5 | |
| Median age | ||
| All patients | 67 | |
| Successful conservative | 69 | P=0.16 |
| management without oral contrast | ||
| Successful conservative | 72 | P=0.47 |
| management with oral contrast | ||
| Patients requiring surgery | 69 | P=0.63 |
| following trial of conservative management | ||
| Palliation | 86 | P=0.04* |
| Out-of-hours hospital admission (%) | ||
| All patients | 65% | |
| Successful conservative | 69% | |
| management without oral contrast | ||
| Successful conservative | 58% | |
| management with oral contrast | ||
| Patients requiring surgery following trial of conservative management | 65% | |
| Median time to CT from admission (hours) | ||
| All patients | 12 | |
| Successful conservative | 12 | P=0.84 |
| management without oral contrast | ||
| Successful conservative | 14 | P=0.12 |
| management with oral contrast | ||
| Patients requiring surgery | 11 | P=0.33 |
| following trial of conservative management | ||
| Median time to surgery from admission | ||
| Patients requiring surgery | 43.5 h | |
| following trial of conservative management | (10-288) | |
| Median time to surgery from CT | ||
| Patients requiring surgery | 19 h | |
| following trial of conservative management | (0-284) | |
| Median length of stay (days) | ||
| All patients | 6.5 | |
| Successful conservative | 6 | P=0.21 |
| management without oral contrast | ||
| Successful conservative | 4.8 | P=0.05* |
| management with oral contrast | ||
| Patients requiring surgery | 10.5 | P=0.02* |
| following trial of conservative management 30-day readmission | ||
| All patients | 3 | |
| Successful conservative | 1 | |
| management without oral contrast | ||
| Successful conservative | 1 | |
| management with oral contrast | ||
| Patients requiring surgery | 1 | |
| following trial of conservative management | ||
CT: Computed tomography, *denotes statistical significance
There is no difference of age between cohorts except the palliative care cohort, which is significantly older.
The majority of patients received a CT scan within 24 h of admission [Figure 2]. The median time to CT scan from the time of admission for all patients was 12 h. Patients initially receiving conservative management with oral contrast had a slightly but not significantly longer median time to CT scan of 14 h.
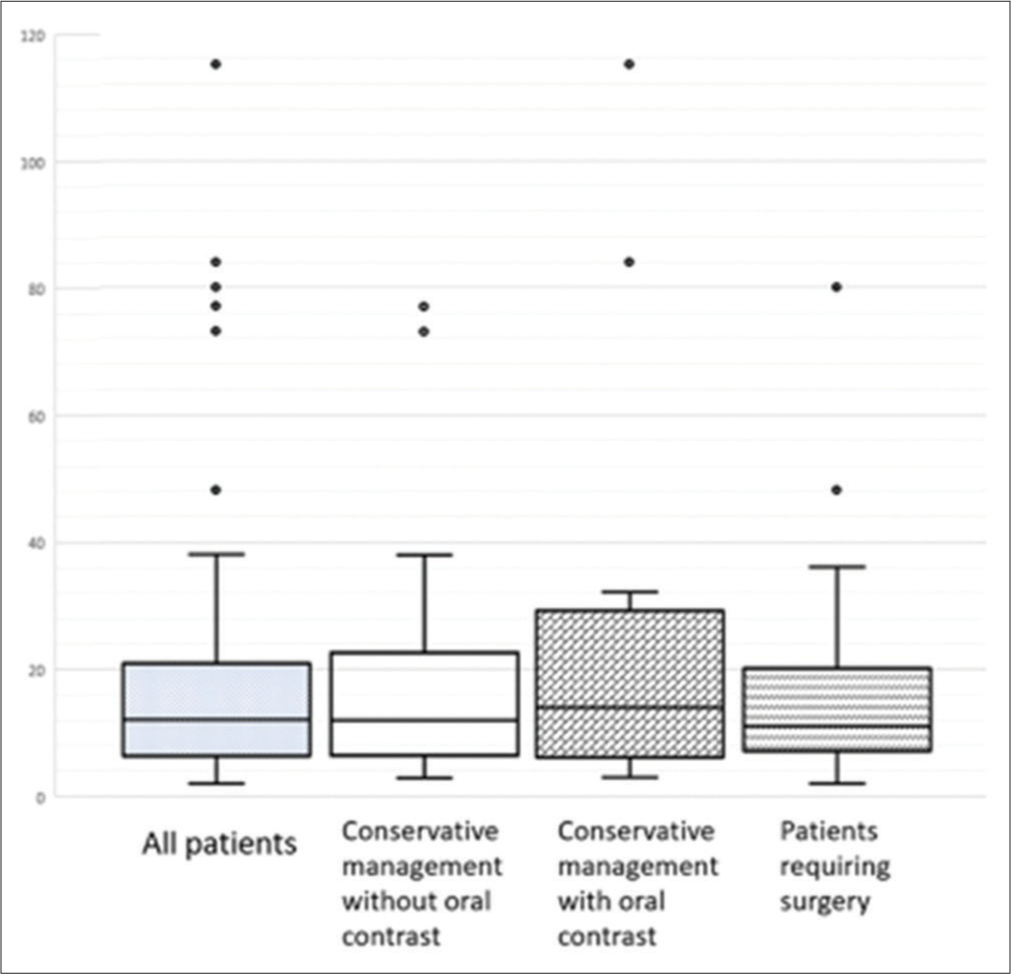
- Box and whisker plot demonstrating the time to computed tomography (CT) scan from admission for all patients and according to the initial management groups; the horizontal lines in each box indicate the median value for time to CT scan, and the outlying values are represented by the dots.
For patients undergoing surgical intervention, the median time to surgery from the time of admission was 43.5 h. The median time from CT scanning to surgery was 19 h. Of note, one patient waited 288 h for surgical intervention from the time of admission. This patient was treated conservatively without WSCA initially and had complete resolution of symptoms, but on the 7th day of the same admission began to redemonstrate symptoms of obstruction.
The length of stay was highest for patients requiring surgery, but this is in keeping with the vast majority proportion of patients failing initial conservative management. There is a significant difference between the two conservatively managed groups of patients: WSCA cohort has a shorter length of stay. Only three patients were re-admitted with small bowel obstruction within 30 days of their initial admission [Table 1]: 1 from each cohort of conservative treatment and 1 from the surgery cohort following unsuccessful conservative measures without WSCA. All three patients resolved without any intervention including further WSCA.
DISCUSSION
This retrospective study was undertaken with the three aims outlined previously. The results have demonstrated several areas of good practice when compared to the results of a national audit,[1] but areas for improvement have also been identified. The results have illustrated prevalent use of CT scan as a diagnostic tool. However, the median time to CT from admission was well above that reported nationally.[1] There was very scant use of WSCA in ASBO during the studied period despite nearly half of all patients being admitted in hours. In contrary to recommendations.[15], the majority did not receive WSCA either at the time of imaging or following diagnosis of ASBO, implicating lack of input from the admitting surgeon.
Utilization of the early CT scanning in acute presentations of small bowel obstruction allows differentiation of mass lesions from adhesions as the cause of obstruction, verification of the presence, or absence of overwhelming metastasis and assists clinicians in identifying closed-loop obstruction. Stable patients with ASBO with no clinical or radiological signs necessitating immediate surgical intervention will undergo a trial of conservative management, as summarized in [Figure 1].
Despite its diagnostic accuracy, early CT scanning in the Emergency Department has not reliably demonstrated the ability to predict failure of conservative management and improve treatment outcomes in patients initially managed nonoperatively for ASBO.[16] It must be noted that Pricolo and Curley’s data were based on portal venous phase CT scan without the use of oral contrast. Our retrospective study has also demonstrated similar results where early CT scanning has not been able to identify patients with ASBO likely to fail conservative management.
Level 1 evidence has previously demonstrated successful conservative treatment in as many as 90% of cases of nonstrangulating ASBO.[17] WSCA was successful in just over half of the small proportion of patients included in this study. In regards to prognostic value of WSCA (and thus importance of early administration, a metaanalysis has previously found that if WSCA reaches the colon within 24 h of its administration, 99% of patients will have a successful outcome with conservative management. On the contrary, if WSCA fails to reach the colon within 24 h, the likelihood of the patient requiring surgical intervention is 90%. The timing and use of WSCA are areas requiring improvements in local guidelines and clinical knowledge and practice.
Lee et al.[18] also advocate the use of WSCA in acute patients with non-strangulated ASBO. Their prospective study of 150 patients concluded that WSCA did not reduce the need for surgical intervention but demonstrated significantly shorter hospital stays favoring the WSCA group. Complications from the use of WSCA include pneumonia, renal failure, anaphylaxis, and even death have been reported.[19] These complications are compared with those resulting from surgical intervention. Avoiding unnecessary delays in the investigation and management of patients with ASBO allows optimization of this group of patients, who may be frail, malnourished, and dehydrated on admission. With careful and frequent clinical monitoring of these patients, only then can successful outcomes of WSCA-induced resolution be determined.
This study has demonstrated no significant difference in the length of stay between the two groups of patients who underwent conservative management, that is, the administration of WSCA agent did not alter length of stay in patients treated conservatively [Table 1]. Similar findings are reported in other studies,[20,21] although reductions in length of stay with the use of WSCA have also been reported.[22] This highlights the importance of daily clinical review, including nursing documentation. However, administration of WSCA assisted in predicting those patients who are likely to need surgical intervention and, therefore, is a useful adjunct in the decision-making process, which is in keeping with recommendations from international guidance.[7]
Surgery in patients with ASBO is associated with higher risk of iatrogenic small bowel injury and the risk of further adhesions. It remains unclear whether surgical intervention for the management of ASBO reduces the risk of future re-admissions for ASBO,[23], especially in an era of minimally invasive surgery.[24]
The study is limited by its retrospective methodology and comparatively small patient sample size: Three groups for a binary outcome leading to a potential type II error. Moreover, it did not compare the time to surgery between the patients receiving WSCA and those who did not. However, key areas of the institution’s practice that are noteworthy include early CT scanning enabling diagnosis and management, a short median time to surgery from admission, and a low 30-day re-admission rate.
CONCLUSION
This retrospective study shares the experience of the management of ASBO from the perspective of an English district general hospital. Early CT allows clinical decision-making for conservative approach. WSCA may also promote quicker resolution of ASBO in a patient who may already be malnourished and dehydrated, but it is also a useful adjunct in the decision-making process when reviewing patients who do not respond to initial conservative management of their ASBO. This study has prompted a multidisciplinary approach to changing local guidelines for the availability of WSCA and management of patients presenting with ASBO.
Research quality and ethics statement
This study was approved by the Institutional Review and Audit Board (Wye Valley NHS Trust). The authors followed applicable EQUATOR Network (https://www.equator-network.org/) guidelines during the conduct of this research project.
Declaration
We also certify that none of the authors is a member of the Editorial board of the Journal of Emergencies, Trauma and Shock.
Declaration of patient consent
Patient’s consent not required as patient identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Report of the National Audit of Small Bowel Obstruction. London: ACPGBI; 2017. p. :1-17.
- [Google Scholar]
- Adhesion-related hospital readmissions after abdominal and pelvic surgery: A retrospective cohort study. Lancet. 1999;353:1476-80.
- [CrossRef] [PubMed] [Google Scholar]
- Intestinal obstruction from adhesions--how big is the problem? Ann R Coll Surg Engl. 1990;72:60-3.
- [Google Scholar]
- Burden of adhesions in abdominal and pelvic surgery: Systemic review and meta-analysis. BMJ. 2013;347:f5588.
- [CrossRef] [PubMed] [Google Scholar]
- Postoperative adhesions: Ten-year follow-up of 12,584 patients undergoing lower abdominal surgery. Dis Colon Rectum. 2001;44:822-9.
- [CrossRef] [PubMed] [Google Scholar]
- Fewer adhesions after laparoscopic surgery? Surg Endosc. 2005;19:862.
- [CrossRef] [PubMed] [Google Scholar]
- Bologna guidelines for diagnosis and management of adhesive small bowel obstruction (ASBO): 2017 update of the evidence-based guidelines from the world society of emergency surgery ASBO working group. World J Emerg Surg. 2018;13:24.
- [CrossRef] [PubMed] [Google Scholar]
- Review of small-bowel obstruction: The diagnosis and when to worry. Radiology. 2015;275:332-42.
- [CrossRef] [PubMed] [Google Scholar]
- Prospective, observational validation of a multivariate small-bowel obstruction model to predict the need for operative intervention. J Am Coll Surg. 2011;212:1068-76.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic utility of CT for small bowel obstruction: Systematic review and meta-analysis. PLoS One. 2019;14:e0226740.
- [CrossRef] [PubMed] [Google Scholar]
- Helical CT signs in the diagnosis of intestinal ischaemia in small-bowel obstruction. Am J Roentgenol. 2000;175:1601-7.
- [CrossRef] [PubMed] [Google Scholar]
- Systematic review and meta-analysis of the diagnostic and therapeutic role of water-soluble contrast agent in adhesive small bowel obstruction. Br J Surg. 2010;97:470-8.
- [CrossRef] [PubMed] [Google Scholar]
- Oral water soluble contrast for the management of adhesive small bowel obstruction. Cochrane Database Syst Rev. 2007;2007:CD004651.
- [CrossRef] [PubMed] [Google Scholar]
- Water-soluble contrast agent in adhesive small bowel obstruction: A systematic review and meta-analysis of diagnostic and therapeutic value. Am J Surg. 2016;211:1114-25.
- [CrossRef] [PubMed] [Google Scholar]
- Small bowel obstruction: A practical step-by-step evidence based approach to evaluation, decision making, and management. J Trauma Acute Care Surg. 2015;79:661-8.
- [CrossRef] [PubMed] [Google Scholar]
- CT findings do not predict outcome of nonoperative management in small bowel obstruction: Retrospective analysis of 108 consecutive patients. Int J Surg. 2016;27:88-91.
- [CrossRef] [PubMed] [Google Scholar]
- Therapeutic effect of oral Gastrograffin in adhesive, partial small-bowel obstruction: A prospective randomized trial. Surgery. 1994;115:433-7.
- [Google Scholar]
- Water soluble contrast follow-through in the management of adhesive small bowel obstruction: A prospective randomized trial. Ann Coll Surg HK. 2004;8:120-6.
- [CrossRef] [Google Scholar]
- Effect of water-soluble contrast in colorectal surgery: A prospective randomized trial. World J Gastroenterol. 2005;11:2802-5.
- [CrossRef] [PubMed] [Google Scholar]
- A protocol for the management of adhesive small bowel obstruction. J Trauma Acute Care Surg. 2015;78:13-9.
- [CrossRef] [PubMed] [Google Scholar]
- Use of water-soluble contrast medium (gastrografin) does not decrease the need for operative intervention nor the duration of hospital stay in uncomplicated acute adhesive small bowel obstruction? A multicenter, randomized, clinical trial (Adhesive Small Bowel Obstruction Study) and systematic review. Surgery. 2017;161:1315-25.
- [CrossRef] [PubMed] [Google Scholar]
- Prospective evaluation of oral gastrograffin in the management of postoperative adhesive small bowel obstruction. Indian J Surg. 2013;75:195-9.
- [CrossRef] [PubMed] [Google Scholar]
- Adhesive small bowel obstruction: Early operative versus observational management. Am Surg. 2015;81:614-20.
- [CrossRef] [PubMed] [Google Scholar]
- Evolving management strategies in patients with adhesive small bowel obstruction: A population-based analysis. J Gastrointest Surg. 2018;22:2133-41.
- [CrossRef] [PubMed] [Google Scholar]







