Translate this page into:
Correlation between serum vitamin D3 and prolactin levels in pre-menopausal women with uterine fibroids
*Corresponding author: Manoj Kumar, Department of Translational and Clinical Research, School of Chemical and Life Sciences, Jamia Hamdard, New Delhi, India. yadavmk4@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Ahmad A, Ahmad M, Bhoi NR, Kumar M. Correlation between serum vitamin D3 and prolactin levels in premenopausal women with uterine fibroids. Indian J Med Sci. doi: 10.25259/IJMS_246_2024
Abstract
Objectives:
Uterine fibroids (UFs) (leiomyomas) are common benign tumors affecting approximately 70% of women of reproductive age. Low serum vitamin D3 levels may promote fibroid growth and disease progression. In addition, fibroids can secrete prolactin (PRL), leading to hyperprolactinemia, which is associated with reproductive disorders and infertility. This study investigates the correlation between serum vitamin D3 (1,25-hydroxyvitamin D3) and PRL levels with fibroid number and size in premenopausal women.
Materials and Methods:
A cross-sectional study was conducted at Indira in vitro fertilization (IVF) Hospital and Fertility Clinics in India from April 15 to November 30, 2022. It included 160 premenopausal women: 80 with fibroids and 80 healthy controls. Cases were women with UFs ≥2 cm in size, diagnosed through transvaginal ultrasonography, compared to healthy controls.
Results:
The mean serum vitamin D3 and PRL levels in the case and control groups were 10.85 ± 3.34 ng/mL versus 19.64 ± 5.50 ng/mL and 27.79 ± 8.19 ng/mL versus 13.96 ± 4.09 ng/mL, respectively. Serum vitamin D3 was significantly lower (P < 0.001), and serum PRL was significantly higher (P < 0.001) in the case group compared to the control group. A strong correlation was observed between serum vitamin D3, PRL, and the number of fibroids in the case group (P < 0.0001). Serum vitamin D3 showed a negative correlation with fibroid number (r = −0.513), while serum PRL showed a positive correlation (r = 0.453), indicating that lower vitamin D3 and higher PRL levels are associated with an increased number of fibroids.
Conclusion:
Our study concluded that women with UFs had significantly lower serum vitamin D3 and higher PRL levels compared to healthy controls. These findings suggest that low vitamin D3 and high PRL levels are associated with increased fibroid number, growth, and disease progression. Thus, serum vitamin D3 and PRL may serve as important biomarkers for the management of UFs.
Keywords
Ectopic prolactin and infertility and biomarkers
Leiomyoma
Premenopausal
Serum prolactin
Serum vitamin D3
Uterine fibroids
INTRODUCTION
Leiomyomas, or uterine fibroids (UFs), are the most common benign tumors in women of reproductive age.[1] These non-cancerous monoclonal tumors originate from uterine smooth muscle cells.[2] UFs affect 70–80% of women, with clinical diagnosis in 25–50% by age 50.[3] Their prevalence varies by factors such as age, race, body mass index (BMI), infertility, premenopausal status, nutrition, and family history.[4] In India, UFs are highly prevalent, especially in women aged 30–40 but can occur at any age, posing a significant burden on women’s health and the healthcare system.[5] UFs can cause reproductive problems, including infertility, miscarriage, adverse pregnancy outcomes, and reduced quality of life.[6]
1,25-dihydroxy vitamin D3, the active form of vitamin D3, suppresses the proliferation of both normal and malignant cells.[7] A study by Sharan et al. (2011) in female Eker rats showed that 1,25-dihydroxy vitamin D3 treatment reduced uterine leiomyoma, partly by regulating genes involved in apoptosis and proliferation. It also decreases fibronectin and collagen type-1 expression, key extracellular matrix proteins.[8] Vitamin D3 reduces the effects of transforming growth factor beta-3 on fibrosis in fibroid cells. Vitamin D3 deficiency may increase the risk of fibroids, with serum levels inversely correlated to their incidence.[9]
Prolactin (PRL) is a polypeptide hormone produced by the anterior pituitary gland,[10] playing a role in mammary gland development and lactogenesis. While primarily a pituitary hormone, PRL is also expressed in tissues such as uterine leiomyomas.[11] Studies suggest that UFs may act as an extra-pituitary source of PRL.[12] Elevated serum PRL levels, resulting from ectopic production by fibroids, may contribute to infertility.[13] The literature review reveals no studies assessing the simultaneous association of vitamin D3 and PRL with UFs. Therefore, this study aims to evaluate the relationship between serum vitamin D3, PRL, and the number and size of UFs in premenopausal women.
MATERIALS AND METHODS
The study data were reported following the strengthening the reporting of observational studies in epidemiology guidelines.[14]
Study design
This is a cross-sectional observational study.
Study setting
The study was conducted at different sites of Indira IVF Hospital and Fertility Clinic in Udaipur, Allahabad, and Kolkata, India, from April to November 2022.
Eligibility criteria
Women were eligible if they were premenopausal, aged 18–50, had at least one UFs ≥2 cm on ultrasound, and were willing to participate. Exclusions were a history of abortion or miscarriage in the past 6 months, previous fibroid surgery, recent use of vitamin D3 or hormonal treatments, pregnancy or lactation, and medications raising serum PRL levels. Additional exclusions were hypothyroidism, chronic renal failure, diabetes mellitus, pituitary disorders, or psychiatric illnesses.
Sample size
The primary efficacy parameters, serum vitamin D3 and PRL, were used to determine the sample size. The calculation was based on a 5% significance level (α), a 95% confidence interval, and 90% power for the calculation. A total of 160 subjects were included, with 80 assigned to each group (case and control).
Research participants
Women visiting the outpatient department of the Reproductive Medicine Department at Indira IVF Hospital and Fertility Clinics were screened for eligibility. Of 510 women assessed, 160 patients meeting the eligibility criteria were recruited and informed consent was obtained. The recruitment process is detailed in Figure 1. All women underwent a two-dimensional transvaginal scan to detect UFs. Women with fibroid lesions ≥2 cm were categorized as cases (n = 80), while those without fibroids were controls (n = 80) and the data were transcribed. The control group was selected to match the study group in terms of age, BMI, and lifestyle factors, ensuring comparability and minimizing confounding variables.
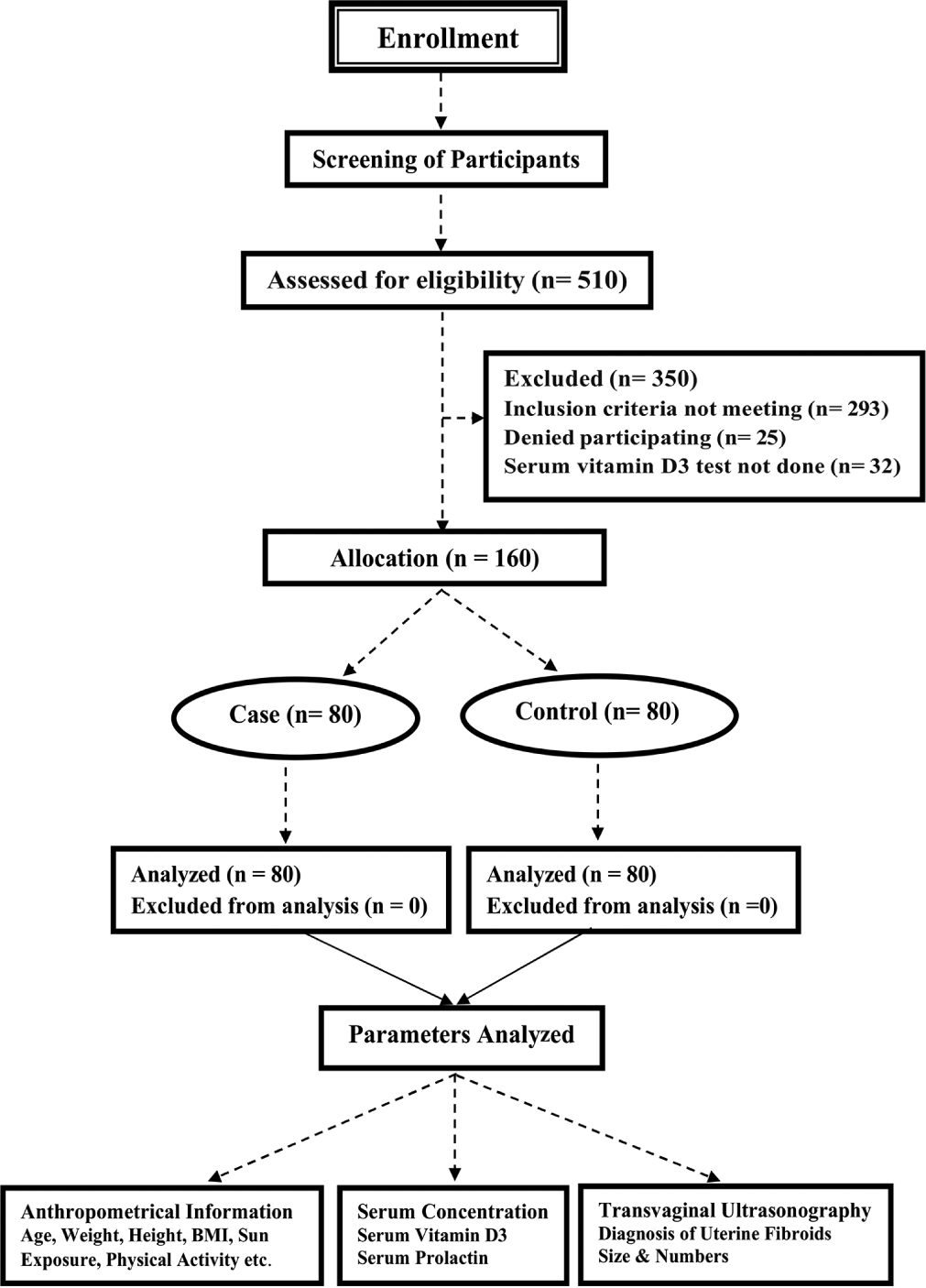
- Flow diagram of the study enrollment, screening, assessment, allocation, and analysis. BMI: body mass index.
Enrolled women provided a 5 mL overnight-fasted blood sample, to extract serum. The samples were then sent to the laboratory at Indira IVF Hospital for the estimation of serum vitamin D3 (1,25-dihydroxy vitamin D3) and PRL levels. The 1,25-vitamin D3 levels were measured directly from the serum to ensure accuracy and specificity using the enzyme-linked immunosorbent assay, while PRL levels were analyzed using the electrochemiluminescence immunoassay. Vitamin D3 status was classified based on the World Health Organization (2003) recommendations: Deficient (<10 ng/mL), Insufficient (10–19.9 ng/mL), and Sufficient (≥20 ng/mL).[15] PRL levels were categorized as normal (≤23.3 ng/mL) or high (>23.3 ng/mL). Anthropometric data include height, weight, BMI, age, and age of menarche. Additional information, such as daily physical activity, sun exposure, family history of UFs, diet, and menstrual cycle regularity, was gathered through interviews and medical record reviews.
Ethical consideration
The study adhered to the International Council for Harmonization of Technical Requirements for Pharmaceuticals for Human Use (ICH) “Guidance for Good Clinical Practices,” ICMR “Guidelines for Biomedical Research on Human Participants,” the Declaration of Helsinki (2013), and applicable regulatory guidelines. The protocol received approval from the Institutional Ethics Committee of Indira IVF Hospital Pvt. Ltd. on March 7, 2022 (study code: IIHPLUDR/P/06_2021) and also registered with Clinical Trial Registry-India (Registration No. CTRI/2022/09/045404).
Statistical analysis
Data were entered into MS Excel and analyzed using the Statistical Package for the Social Sciences version 16.0. Continuous data were expressed as mean ± standard deviation and categorical data as frequency and percentage. The association between cases and controls and relevant risk factors was assessed using Chi-square and independent t-tests. Pearson correlation for linear relationships and Spearman for non-parametric data were used. A P < 0.05 was considered statistically significant.
RESULTS
A total of 510 women were assessed for eligibility, and 160 women meeting the criteria were included in the study (80 cases and 80 controls). The mean age was 34.96 ± 5.15 years, and all participants were premenopausal and of reproductive age. The highest percentage (63.75%) of UFs was found in women aged 31–40 years, while the lowest percentage (16.25%) was in women aged ≤30 years, as shown in Table 1.
| Characteristics | Case (n=80) | Control (n=80) | Total (n=160) | P-value |
|---|---|---|---|---|
| Age (years), (Mean±SD) | 35.67±5.06 | 34.26±5.15 | 34.96±5.15 | 0.08* |
| ≤30, n (%) | 13 (16.25) | 15 (18.75) | 28 (17.5) | 0.87** |
| 31–40, n (%) | 51 (63.75) | 51 (63.75) | 102 (63.75) | |
| >40, n (%) | 16 (20) | 14 (17.5) | 30 (18.75) | |
| Age at menarche (year), (Mean±SD) | 12.82±1.52 | 13.02±1.45 | 12.92±1.49 | 0.40* |
| Body mass index (kg/m2) (Mean±SD) | 25.24±3.54 | 24.76±3.28 | 25.00±3.42 | 0.37* |
| Normal (18.5–24.9 kg/m2), n (%) | 40 (50) | 48 (60) | 88 (55) | 0.44** |
| Overweight (25–29.9 kg/m2), n (%) | 33 (41.25) | 26 (32.5) | 59 (36.87) | |
| Obese (30–34.9 kg/m2), n (%) | 7 (8.75) | 6 (7.5) | 13 (8.12) | |
| Menstrual cycle status | ||||
| Irregular, n (%) | 10 (12.5) | 5 (6.25) | 15 (9.37) | 0.17** |
| Regular, n (%) | 70 (87.5) | 75 (93.75) | 145 (90.62) | |
| Physical activity status (No. of hrs/week) | ||||
| <1 h., n (%) | 34 (42.5) | 49 (61.25) | 83 (51.87) | <0.001** |
| 1–2 h., n (%) | 20 (25) | 7 (8.75) | 27 (16.87) | |
| >2 h., n (%) | 26 (32.5) | 24 (30) | 50 (62.5) | |
| Duration of sun exposure (No. of h/day) | ||||
| Low (<1 h.), n (%) | 59 (73.75) | 22 (27.5) | 81 (50.62) | <0.001** |
| Medium (1 h.), n (%) | 11 (13.75) | 36 (45) | 47 (29.37) | |
| High (>1 h.), n (%) | 10 (12.5) | 22 (27.5) | 32 (20) | |
| Diet | ||||
| Vegetarian, n (%) | 41 (51.25) | 28 (35) | 69 (43.12) | 0.03** |
| Non-vegetarian, n (%) | 39 (48.75) | 52 (65) | 91 (56.87) |
The general characteristics of the women were presented in Table 1. The mean age, age at menarche, and BMI in the case and control groups were 35.67 ± 5.06 and 34.26 ± 5.15 years, 12.82 ± 1.52 and 13.02 ± 1.45 years, and 25.24 ± 3.54 and 24.76 ± 3.28 kg/m2, respectively. There were no significant differences observed between the study groups in terms of age, age at menarche, BMI, and menstrual cycle status. However, concerning other general characteristics such as physical activity, duration of sun exposure, and diet, a statistically significant difference was observed between the study groups (P < 0.05).
Table 2 shows the distribution of women based on serum concentration of vitamin D3 and PRL levels in the case and control groups. The mean serum concentration of vitamin D3 and PRL levels in both the case and control groups was 10.85 ± 3.34 ng/ml and 19.64 ± 5.50 ng/mL and 27.79 ± 8.19 and 13.96 ± 4.09 ng/mL, respectively. A highly statistically significant difference was observed between the study groups (P < 0.001).
| Characteristics | Case (n=80) | Control (n=80) | Total (n=160) | P-value |
|---|---|---|---|---|
| Serum Vitamin D3 (ng/mL), (Mean ± SD) | 10.85 ± 3.34 | 19.64 ± 5.50 | 15.25 ± 6.31 | <0.001* |
| Deficient (<10 ng/mL), n (%) | 37 (46.25) | 5 (6.25) | 42 (26.25) | <0.001** |
| Insufficient (10–19.9 ng/mL), n (%) | 43 (53.75) | 27 (33.75) | 70 (43.75) | |
| Sufficient (≥20 ng/mL), n (%) | 0 (0) | 48 (60) | 48 (30) | |
| Serum Prolactin (ng/mL), (Mean ± SD) | 27.79 ± 8.19 | 13.96 ± 4.09 | 20.87 ± 9.47 | <0.001* |
| Normal (≤23.3 ng/mL), n (%) | 19 (23.75) | 79 (98.75) | 98 (61.25) | <0.001** |
| High (>23.3 ng/mL), n (%) | 61 (76.25) | 1 (1.25) | 62 (38.75) |
Table 3 shows the correlation between serum vitamin D3 and PRL levels in the case group, expressed as numbers and percentages. No significant difference was observed (P > 0.05).
| Characteristics | Serum Vitamin D3 | Total | P-value | |
|---|---|---|---|---|
| Deficient (<10 ng/mL) | Insufficient (10–19.9 ng/mL) | |||
| Serum prolactin | ||||
| Normal (≤23.3 ng/mL), n (%) | 7 (36.84) | 12 (63.15) | 19 | 0.34** |
| High (>23.3 ng/mL), n (%) | 30 (49.18) | 31 (50.81) | 61 | |
| Total | 37 (46.25) | 43 (53.75) | 80 | |
Table 4 presents the correlation between serum vitamin D3, PRL levels, and the number and size of fibroids in women. A negative correlation was observed between serum vitamin D3 levels and the number of fibroids (r = −0.513), with lower vitamin D3 levels associated with a higher number of fibroids (P < 0.0001). Conversely, serum PRL levels showed a positive correlation with the number of fibroids (r = 0.453), indicating that higher fibroid numbers were associated with higher PRL levels (P < 0.0001).
| Characteristics | r/P-value | Serum Vitamin D3 (ng/mL) | Serum prolactin (ng/mL) | Numbers of fibroid | Size of fibroids |
|---|---|---|---|---|---|
| Serum vitamin D3 (ng/mL) | r | −0.099 | −0.513*** | 0.006 | |
| P-value | 0.383 | <0.0001 | 0.961 | ||
| Serum prolactin (ng/mL) | r | −0.099 | 0.453*** | 0.154 | |
| P-value | 0.383 | <0.0001 | 0.172 | ||
| Numbers of fibroids | r | −0.513*** | 0.453*** | 0.215 | |
| P-value | <0.0001 | <0.0001 | 0.056 | ||
| Size of fibroids | r | 0.006 | 0.154 | 0.215 | |
| P-value | 0.961 | 0.172 | 0.056 |
Figure 2 shows the distribution of serum vitamin D3 levels in the case and control groups. The box plot illustrates individual data points, interquartile ranges Q1 (25%) to Q3 (75%), and whiskers representing the minimum and maximum values. A line across the box indicates the median (Q2, 50%), while dots beyond the whiskers signify outliers. Serum vitamin D3 levels were significantly lower in the case group than in the control group (P < 0.001).
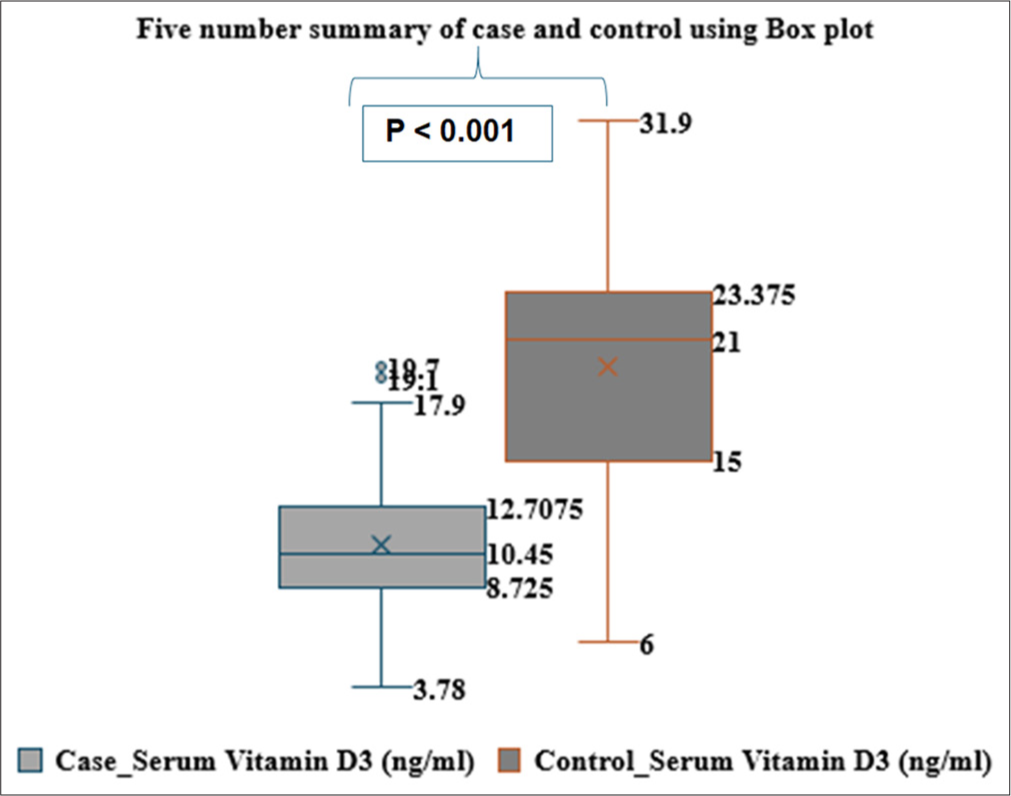
- Box Plot represents the distribution of vitamin D3 levels in case and control groups.
Figure 3 shows the distribution of serum PRL levels in the case and control groups. The box plot represents individual data points, interquartile ranges Q1 (25%) to Q3 (75%), and whiskers indicating the minimum and maximum values. A line within the box marks the median (Q2, 50%), while dots beyond the whiskers indicate outliers. Serum PRL levels were significantly higher in the case group than in the healthy control group (P < 0.001).
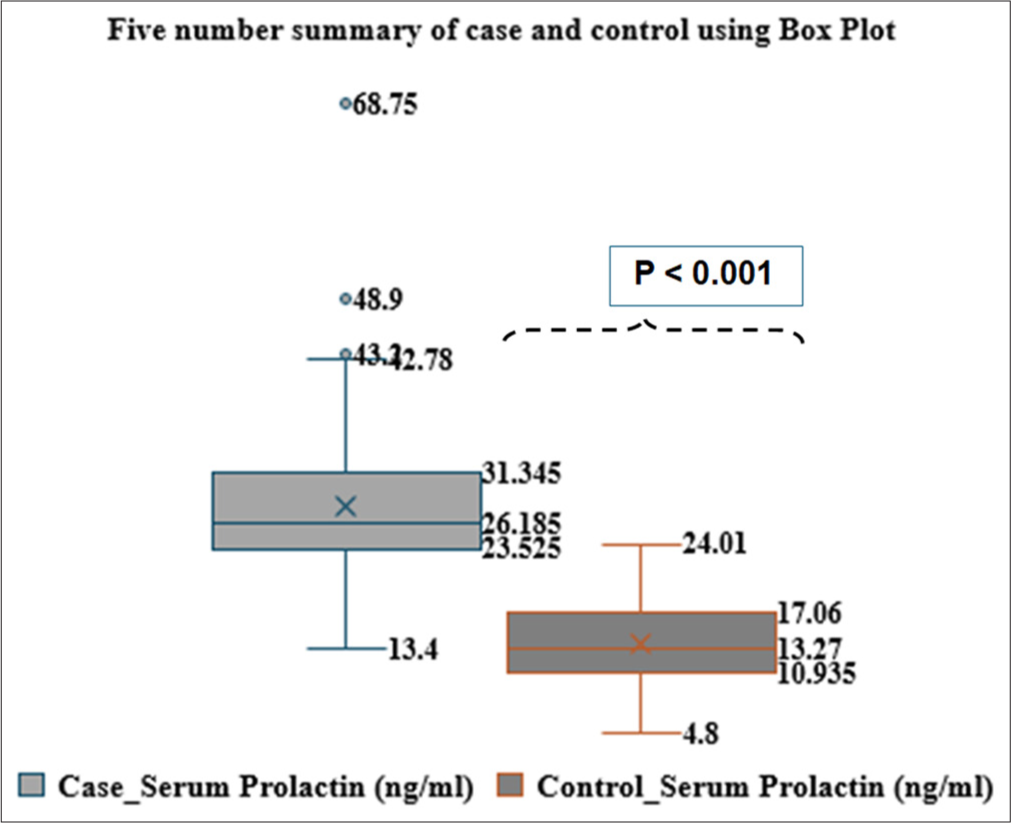
- Box plot represents the distribution of serum prolactin levels in case and control groups.
DISCUSSION
The initial data from our study suggest that the serum vitamin D3 levels were significantly lower in women with UFs compared to healthy controls (10.85 ± 3.34 ng/mL vs. 19.64 ± 5.50 ng/mL), respectively. Among women with deficient serum vitamin D3 levels, approximately (46.25%) were in the case group, whereas only (6.25%) were in the healthy control group. At the insufficient level of vitamin D3, around (53.75%) of women were in the case group, compared to (33.75%) in the healthy control group. However, at the sufficient level of vitamin D3, no women (0%) were found in the case group, whereas (60%) of women in the healthy control group had sufficient levels. Overall, the majority of women with UFs exhibited low serum vitamin D3 levels, and this difference was highly statistically significant (P < 0.001), with a recent case–control study conducted by Srivastava P et al. (2020), at Era’s Medical College and Hospital, Lucknow, India. In that study, 90 patients (45 cases and 45 controls) were included to estimate the levels of 25-hydroxy vitamin D3 in women with and without UFs. 25-hydroxy vitamin D3 was significantly lower in women with fibroids compared to non-fibroid women (15.10 ± 6.09 vs. 26.09 ± 7.90, respectively [P < 0.001]). The study also concluded that vitamin D3 deficiency is significantly associated with the occurrence of UFs.[15]
Similarly, our study findings also suggest that the serum concentration of PRL levels was significantly higher in women with UFs compared to healthy controls (27.79 ± 8.19 ng/mL vs. 13.96 ± 4.09 ng/mL), respectively. At normal (≤23.3 ng/mL) levels of serum PRL concentration, almost (23.75%) of women with fibroids and (98.75%) of healthy control women were observed. However, at higher (>23.3 ng/mL) levels of serum PRL concentration, (76.25%) and (1.25%) of women were seen in cases and healthy controls, respectively. Overall, the highest percentage of women with UFs exhibited elevated serum PRL levels, and this difference was statistically significant (P < 0.001), as shown in Table 2. This is consistent within previous studies conducted by Abdulla MM et al. (2012).[13] In this study, they included 103 women with UFs. They reported that the increase in serum PRL levels was attributed to ectopic production from UFs. Furthermore, their findings indicated that there was no effect or role of this PRL on thyroid hormone function, and infertility could be associated with the presence of PRL -secreting fibroids.[16]
The study also investigated the correlation between serum vitamin D3 and PRL with the number and size of fibroids among women with fibroids. The correlation between serum vitamin D3 and the number of fibroids was found to be negative (r= −0.513), indicating that a decrease in serum vitamin D3 levels was associated with an increase in the number of fibroids. This correlation was highly statistically significant (P < 0.0001). Alternatively, the correlation between serum PRL and the number of fibroids was positive (r = 0.453), suggesting that an increase in the number of fibroids was correlated with an increase in serum PRL levels. This correlation was also highly statistically significant (P < 0.0001), as shown in Table 4. These findings align with the results of a cross-sectional observational study by Sabry M et al. (2013), at the gynecology clinic of Sohag University’s Faculty of Medicine in Sohag, Egypt. In this study, 154 premenopausal women (50 healthy controls and 104 cases) the study reported a significant association between lower serum vitamin D3 levels and the occurrence of UFs (P = 0.01). An inverse correlation was also observed between serum vitamin D3 levels and total fibroid volume within the case cohort (r = −0.31; P = 0.002). Women with larger fibroid volumes had lower serum vitamin D3 levels and vice versa.[9]
In addition, “in vitro” studies have explored the potential role of vitamin D3 in growth UFs and progression. These studies revealed that vitamin D3 inhibits the growth of Human Leiomyoma (HuLM) cells downregulation of proliferating cell nuclear antigen, Cyclin-Dependent Kinase 1 (CDK1), and B-Cell Leukemias (BCL-2) and it suppresses CatecholO-Methyltransferase (COMT) expression and activity in HuLM cells. Vitamin D3 deficiency may be an important risk factor in the growth and progression of fibroids.[11] Vitamin D3 seems to reduce the effects of transforming growth factor beta-3 and fibrosis in human leiomyoma cells. It also limits the aberrant expression of major extracellular matrix-associated proteins. Specifically, 1,25-dihydroxy vitamin D3 is identified as an antifibrotic factor potentially suitable as a new therapeutic approach for the non-invasive treatment of UFs.[17] Recently, a few “Randomized Controlled Clinical Trials” conducted by Vahdat M. et al., (2022), Arjeh S. et al., (2020), and Tanha FD. et al., (2021) have reported that vitamin D3 supplementation prevents fibroid growth. It appears that vitamin D3 supplementation is a simple, safe, and inexpensive inhibiting leiomyoma growth, preventing recurrence, and reducing the size of recurrent UFs.[1,2,4] The study provides the early clinical data on the correlation of serum vitamin D3 and PRL levels with the number of fibroids in premenopausal women, both with and without UFs. The weakness of this study may be its small sample size. However, to provide substantial confirmation of these findings, long-term clinical trials with larger sample sizes are necessary.
CONCLUSION
The study found that serum vitamin D3 levels were significantly lower, while serum PRL levels were significantly higher in women with UFs compared to healthy controls. A negative correlation was observed between serum vitamin D3 levels and the number of fibroids, indicating that lower vitamin D3 levels were associated with more fibroids. In contrast, a positive correlation was found between serum PRL levels and the number of fibroids, suggesting that higher PRL levels were linked to an increase in fibroids. These findings highlight the role of both serum vitamin D3 and PRL in fibroid growth and progression, recommending their monitoring as biomarkers for UFs management.
Acknowledgment:
The authors thank Professor S.M. Hasan, Dean of the Faculty of Pharmacy at Integral University Lucknow, for his technical support and guidance. Thanks also to the Dean of research and development (R&D), Integral University, for assigning manuscript communication reference: IU/R&D/2023-MCN0002110. The authors are grateful to the Institutional Ethics Committee of Indira IVF Hospital Pvt. Ltd., for approving and permitting the conduct of the study. Finally, the authors thank all participants who kindly agreed to take part in the study.
Ethical approval:
The study was approved by the Institutional Review Board at Institutional Ethics Committee of Indira IVF Hospital Pvt. Ltd., number IIHPL-UDR/P/006_2021, dated March 07, 022.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- The effect of vitamin D on recurrence of uterine fibroids: A randomized, double-blind, placebo-controlled pilot study. Complement Ther Clin Pract. 2022;46:101536.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of oral consumption of vitamin D on uterine fibroids: A randomized clinical trial. Complement Ther Clin Pract. 2020;39:101159.
- [CrossRef] [PubMed] [Google Scholar]
- Hypovitaminosis D exacerbates the DNA damage load in human uterine fibroids, which is ameliorated by vitamin D3 treatment. Acta Pharmacol Sin. 2019;40:957-70.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of vitamin D deficiency on overgrowth of uterine fibroids: A blinded randomized clinical trial. Int J Fertil Steril. 2021;15:95.
- [Google Scholar]
- Vitamin D 3 level in women with uterine fibroid: An observational study in eastern Indian population. J Obstet Gynecol India. 2019;69:161-5.
- [CrossRef] [PubMed] [Google Scholar]
- The association between vitamin D and uterine fibroids: A Mendelian randomization study. Front Genet. 2022;13:2529.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of vitamin D3 Supplementation on symptomatic uterine leiomyoma in women with hypovitaminosis D. J Midlife Health. 2021;12:53.
- [CrossRef] [PubMed] [Google Scholar]
- Vitamin D inhibits proliferation of human uterine leiomyoma cells via catechol-O-methyltransferase. Fertili Steril. 2011;95:247-53.
- [CrossRef] [PubMed] [Google Scholar]
- Serum vitamin D3 level inversely correlates with uterine fibroid volume in different ethnic groups: A cross-sectional observational study. Int J Womens Health. 2013;5:93-100.
- [CrossRef] [PubMed] [Google Scholar]
- Prolactin: Structure, function, and regulation of secretion. Physiol Rev. 2000;80:1523-631.
- [CrossRef] [PubMed] [Google Scholar]
- Serum protein and prolactin in evaluation of uterine fibroids. Egypt J Hosp Med. 2019;76:3653-8.
- [CrossRef] [Google Scholar]
- Physicochemical characterization and functional activity of fibroid prolactin produced in cell culture. Am J Obstet Gynecol. 1988;158:846-53.
- [CrossRef] [PubMed] [Google Scholar]
- Role of ectopic prolactin on thyroid hormones level in a sample of Iraqi infertile women with uterine fibroids. Iraqi J Med Sci. 2012;10:334-8.
- [Google Scholar]
- STROBE Statement-checklist of items that should be included in reports of cross-sectional studies. Univ Los Andes. 2020;1:1-2.
- [Google Scholar]
- Evaluation of 25-hydroxy vitamin D3 levels in patients with a fibroid uterus. J Obstet Gynaecol. 2020;40:710-4.
- [CrossRef] [PubMed] [Google Scholar]
- A study to correlate association between vitamin D with fibroid and its supplementation in the progression of the disease. Int J Reprod Contracept Obstet Gynecol. 2020;9:1477-82.
- [CrossRef] [Google Scholar]
- 1, 25-Dihydroxyvitamin D3 reduces TGF-β3-induced fibrosis-related gene expression in human uterine leiomyoma cells. J Clin Endocrinol Metab. 2011;96:E754-62.
- [CrossRef] [PubMed] [Google Scholar]







