Translate this page into:
Efficacy of neutrophil-lymphocyte ratio, serum lactate, and lactate clearance in predicting mortality in patients with sepsis admitted to a tertiary care hospital: A prospective observational study
*Corresponding author: Puneet Khanna, Department of Anaesthesiology Pain Medicine and Critical Care, All India Institute of Medical Sciences, New Delhi, India. k.punit@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Akshat S, Roy A, Mukkelli VG, Anand RK, Baidya DK, Ray BR, et al. Efficacy of neutrophil-lymphocyte ratio, serum lactate, and lactate clearance in predicting mortality in patients with sepsis admitted to a tertiary care hospital: A prospective observational study. Indian J Med Sci. doi: 10.25259/IJMS_265_2023
Abstract
Objectives:
Neutrophil-to-lymphocyte ratio (NLR), serum lactate, and lactate clearance (LC) are frequently used for rapid bedside assessment of the severity of sepsis. This study aimed to evaluate the individual and combined efficacy of NLR, serum lactate, and LC, measured in the emergency department (ED), in predicting 28-day mortality.
Materials and Methods:
This was a single-center and prospective observational study, conducted in a tertiary care hospital (CTRI/2018/08/015371). The study included adult patients aged 18–80 years, admitted to the ED with sepsis. Along with baseline demographic and hemodynamic variables, NLR, serum lactate, and LC were collected. Patients were followed until death or for a maximum of 28 days.
Results:
Out of 50 patients, 33 survived (66%). Non-survivors had lower systolic, diastolic, mean blood pressure, lower LC, tachycardia, high sequential organ failure assessment score, vasopressors requirement, mechanical ventilation requirement, and high NLR. NLR (≥11.13) was best correlated with 28-day mortality [area under receiver operating curve (AUROC) 0.87], followed by initial lactate (≥3.3, AUROC 0.77) and LC (≤17.07%, AUROC 0.73). Multivariate logistic regression revealed that NLR and LC were independent predictors of mortality, with weak correlation between them. However, their combination did not perform better (AUROC 0.82) than individual markers.
Conclusion:
NLR and LC can be used with moderate certainty in predicting 28-day mortality.
Keywords
Sepsis
Lactate clearance
Neutrophil-lymphocyte ratio
Mortality
Emergency department
INTRODUCTION
Sepsis is a life-threatening organ dysfunction caused by a dysregulated host response to an infection.[1] Other than contributing to significant morbidity and mortality, it has brought forth a substantial health care and economic burden worldwide during the past decade.[2] In hospital, the mortality rate in patients with septic shock is approximated to 30%, making sepsis the second most common cause of death.[1,3,4]
Biomarkers have different diagnostic and prognostic implications in predicting outcomes in patients with sepsis and septic shock.[5] Among different biomarkers, serum procalcitonin (PCT) and C-reactive protein (CRP) have been used since ages in sepsis for different purposes, denoting disease severity, prediction of outcome/death, antibiotic de-escalation, etc. However, both the above parameters have been shown to be raised due to non-infective inflammatory causes; thus, their reliability in predicting disease outcome has been questioned.[6] In postoperative sepsis patients, though serum PCT levels decreased significantly among survivors, CRP levels did not differ.[7] Moreover, due to significant inter-individual variation, no standard cutoff values could be proposed.[7]
The neutrophil-to-lymphocyte ratio (NLR) is a rapid and simple parameter that can be used to predict severity and outcomes in sepsis patients.[6,8] Underlying infection leads to an increase in neutrophil count, whereas inflammatory stress leads to lymphopenia.[9] These factors along with sepsis-induced lymphocyte apoptosis increase NLR, which helps to stratify patients as per disease severity even before a change in total leucocyte count (TLC). Serum lactate levels and lactate clearance (LC) are often used as a surrogate marker for tissue hypoperfusion and also serve to prognosticate patients with sepsis. Presentation at advanced stage of sepsis leads to death within 24 h or may have protracted hospital course, performance of these biomarkers in these clinical scenarios is questionable. Different cutoff values of LC have been proposed, as to denote adequate response to therapy.[10-12] Studies found that persistently elevated lactate and lactate non-clearance are ominous signs associated with worse outcomes in sepsis.
In patients with sepsis admitted to intensive care unit (ICU), both NLR (≥14.08 ng/mL) and serum lactate (≥2.99 mmol/L) predicted 28-day mortality with moderate certainty [area under receiver operating curve (AUROC) ~0.6]; however, their combination performed better (AUROC ~0.7).[13] While individual markers may predict major health-related outcomes with varying reliability across different patient population, their combined values may be more accurate. Rapid bedside prognostic markers are of paramount importance in the emergency department (ED), helping to triage patients and tailor treatment accordingly. Therefore, we aim to evaluate the individual as well as combined efficacy of NLR, serum lactate, and LC, measured on presentation to the ED, in predicting 28-day mortality due to sepsis.
MATERIALS AND METHODS
Study design and setting
This was a single center prospective and observational study, conducted during September 2018 and October 2019. The study protocol was approved by the Institutional Ethics Committee (IECPG-665/January 31, 2018) and prospectively registered in the Clinical Trial Registry of India (CTRI/2018/08/015371).
Selection of participants
We included adult patients with age between 18 and 80 years with sepsis, defined as positive quick sequential organ failure assessment (q-SOFA) with confirmed or presumed infection and an initial lactate value ≥2 mmol/L. Participant informed consent was obtained before including the patients in the study. We excluded the following patients:
Patients with end-stage renal disease, those on hemodialysis, acute kidney injury, acute cerebrovascular accident, acute coronary syndrome, acute pulmonary edema, status asthmaticus, uncontrolled seizure, and trauma, uncontrolled hemorrhage, known liver disease, hematological disease, and those receiving corticosteroid
Patients in who end-of-life care bundle were activated.
Patients were serially included in this study. An investigator who was not aware of the NLR, serum lactate, and LC, followed the patients until death or discharge or until 28 days from recruitment whichever was earlier. Finally, all patients were divided into two groups for analysis based on 28-day survival: (a) The survivor group and (b) the non-survivor group.
Measurements and data collection
Under aseptic precautions, two peripheral venous blood samples were collected from the participants, within 1 h of ED admission and sent for analysis. (i) Blood samples collected in ethylenediaminetetraacetic acid vacutainers were used for measurement of complete blood count, [including hemoglobin, TLC, absolute neutrophil count, absolute lymphocyte count (ALC), and platelet count] by hematology analyzer (Pentra XLR, Horiba Ltd. Kyoto, Japan) and (ii) blood samples collected in heparinized syringes were used for serum lactate measurement by ABG analyzer (ABL800 Flex, Radiometer Medical Aps, Copenhagen, Denmark).
After 6 h from the time of first sample collection, a second blood samples were collected and sent for serum lactate measurement as mentioned above.
LC was calculated by the formula:
NLR was calculated by the formula:
Patient demographics, ideal body weight, comorbidities, initial vital signs, that is, heart rate (HR), respiratory rate (RR), systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial blood pressure (MAP), and the Glasgow coma scale (GCS) were noted. Blood samples were collected for measurement of renal functions (i.e., urea and creatinine) and liver functions (i.e., bilirubin). Patients were treated as per physician’s discretion and as per prevailing standard protocol.[1] We calculated the following composite variables: -
Shock index (SI) = HR/SBP
Total sequential organ failure assessment (SOFA) score
q-SOFA score.
Statistical analysis
We did not calculate any sample size at beginning. Planned to do an interim power analysis after arbitrarily recruiting 50 patients and include patients further (in multiples of 25), if needed. All the data were tabulated in a Microsoft Excel spreadsheet and were subjected to statistical analysis by Statistical Product and Service Solutions (SPSS) statistical software (IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp.). Demographic data were expressed as mean ± standard deviation (SD) or proportions as applicable. Normally, distributed data were analyzed by two way/paired “t”-test. Non-normally distributed data were represented as median (inter-quartile range) and analyzed using Mann–Whitney “U”-test/Wilcoxon rank sum test. Univariate logistic regression was used to evaluate relationship between independent and dependent variable. Multivariate logistic regression was conducted to examine the association between NLR and LC with mortality, while adjusting for confounders. Receiver operating curves were derived against NLR, serum lactate, and LC in predicting mortality. Youden index was used to determine cutoff values for NLR, serum lactate, and LC. Spearman’s correlation coefficient was used to determine correlation between the studied biomarkers. P < 0.05 was considered statistically significant.
RESULTS
Demographic parameters, vitals, and interventions
A total of 87 patients were screened sequentially, throughout the study period and after applying inclusion/exclusion criteria, 50 patients were analyzed [Figure 1]. The mean age of the population was 52.82 (±12.73) (mean [±SD]), 46% were male. Based on 28-day mortality, 64% were survivors.
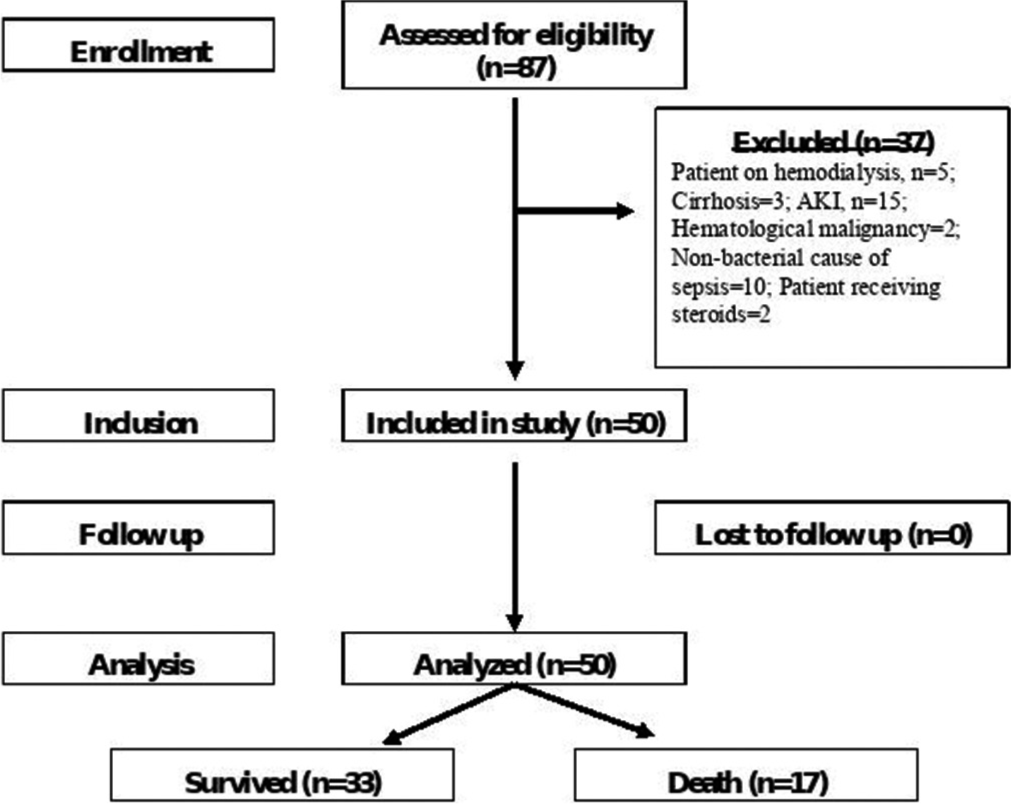
- Flow chart of the study. AKI: Acute kidney injury.
During interim analysis, the AUROCs of variables showed moderate to fair predictive accuracy. Post hoc power analysis was performed, considering survivors (n = 33) and non-survivors (n = 17) as separate groups, based on all three parameters, that is, NLR, LC, and initial lactate, the power analysis showed 97%, 55.6%, and 84% power with respect to NLR, LC, and lactate, respectively. Therefore, no further patients were included after this analysis.
Baseline demographic characteristics as well as status of co morbidities were similar between the two groups [Table 1]. However, survivor group had higher SBP, DBP, MAP, similar RR and GCS, and lower HR than non-survivors, which were both clinically and statistically significant.
| Parameters | Survivors (n=33 [66%]) | Non-survivors (n=17 [34%]) | P-value |
|---|---|---|---|
| Age, (mean±SD) | 51.06±12.95 | 56.24±11.93 | 0.176 |
| Male gender, n (%) | 14 (42.42) | 9 (52.90) | 0.490 |
| Ideal body weight (kg), (mean±SD) | 65.09±12.17 | 68.18±13.86 | 0.422 |
| Cardiovascular disease, n (%) | 11 (33.33) | 8 (26.09) | 0.354 |
| COPD, n (%) | 6 (18.18) | 2 (11.76) | 0.567 |
| Diabetes, n (%) | 10 (30.30) | 3 (15.38) | 0.152 |
| Others (Depression, BPH), n(%) | 2 (6.06) | 0 (0) | 0.059 |
| Systolic blood pressure (mm Hg), (mean±SD) | 103.03±23.69 | 84.12±13.77 | 0.001** |
| Diastolic blood pressure (mm Hg), (mean±SD) | 70.48±24.75 | 48.71±9.48 | 0.001** |
| Heart rate (beats/min), (mean±SD) | 114.09±12.77 | 126.94±8.25 | 0.011** |
| Respiratory rate (breaths/min), (mean±SD) | 32.12±4.78 | 37±4.80 | 0.437 |
| GCS, (mean±SD) | 13.21±2.32 | 11.94±2.60 | 0.086 |
| q-SOFA, median (IQR) | 2 (2–2) | 3 (2–3) | 0.02** |
| SOFA score baseline, media n (IQR) | 5 (4–7) | 11 (6–12) | 0.001** |
| Fluid infused in first 6 h (mL), (mean±SD) | 1432.12±236.09 | 1501.76±273.61 | 0.354 |
| Vasopressors used within 6 h, n (%) | 8 (24.24) | 11 (64.70) | 0.015** |
| Need for mechanical ventilation, n (%) | 36.36 | 76.47 | 0.006** |
Expectedly, the q-SOFA scores were higher for non-survivors as compared to survivors. The survivor group had lesser requirement of vasopressors and mechanical ventilation, had significantly lower SOFA score as compared to non-survivors [Table 1].
Laboratory and derived parameters
The two groups had similar hemoglobin, TLC, platelet count, and creatinine levels. Pneumonia, abdominal sepsis, and urinary tract infection were the three most prevalent sepsis syndromes, and their distribution was also similar between the groups. NLR and initial serum lactate levels were higher, and LC was lower among non-survivors [Table 2].
| Parameters | Survivors (n=33) | Non survivors (n=17) | P-value |
|---|---|---|---|
| Hb (g/dL), (mean±SD) | 10.72±2.72 | 9.90±2.44 | 0.299 |
| TLC (/mm3), (mean±SD) | 16636.06±8009.96 | 17747.06±11603.93 | 0.693 |
| ANC (/mm3), (mean±SD) | 14078±7548.97 | 14718±9404.95 | 0.795 |
| ALC (/mm3), (mean±SD) | 1639.15±1035.77 | 808.12±424.73 | 0.003 |
| Platelet count (/mm3), (mean±SD) | 171212.12±105124.55 | 158235.29±133627.06 | 0.708 |
| Creatinine (mg/dL), (mean±SD) | 1.003±0.17 | 1.07±0.13 | 0.141 |
| Bilirubi n(mg/dL), (mean±SD) | 1.99±0.83 | 4.3±2.95 | 0.0001 |
| LC (%), median (IQR) | 23.07 (17.24–27.27) | 11.11 (4.35–16.66) | 0.02** |
| NLR, median (IQR) | 8.64 (6–12.36) | 16.86 (11.13–35.73) | 0.003** |
| Initial lactate, media n (IQR) | 2.8 (2.4–3.3) | 4.2 (3.1–7.1) | 0.046** |
| Pneumonia, n (%) | 17 (51.51) | 9 (52.94) | 0.926 |
| UTI, n (%) | 11 (33.33) | 6 (35.29) | 0.892 |
| Abdominal sepsis, n (%) | 3 (9.09) | 2 (11.76) | 0.771 |
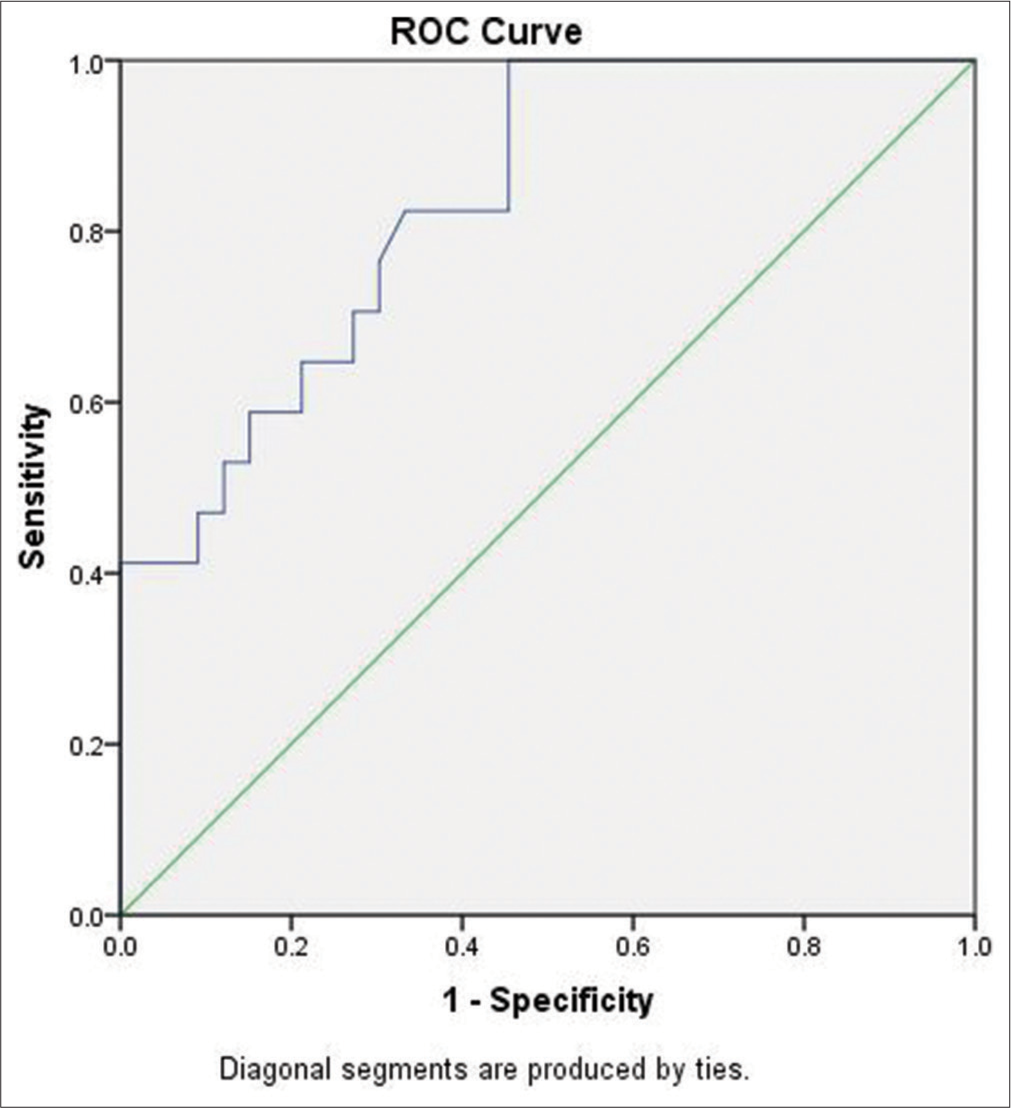
Relationship between NLR, LC, initial lactate, and mortality
NLR, serum lactate, and LC predicted mortality with moderate to good certainty; however, combination of NLR and LC did not increase predictive accuracy. NLR, combination of NLR and LC, and LC had AUROC in descending order [Table 3, Figures 2 and 3]. After adjusting for confounding variables, that is, DBP, SI, and SOFA score, multistep multivariate regression analysis revealed that, both LC and NLR were able to predict mortality independently [Table 3]. NLR, initial lactate, and LC showed weak to modest correlation between them (NLR vs. LC-spearman coefficient, r = 0.358 [P = 0.01] and NLR vs. initial serum lactate-r = 0.313 [P = 0.03]) [Figures 4 and 5].
| Biomarker | AUROC | Optimal cut-off | Sensitivity (%) | Specificity (%) | P-value |
|---|---|---|---|---|---|
| NLR | 0.87 | 11.13 | 76.47 | 69.70 | 0.002** |
| Lactate clearance (%) | 0.73 | 17.07 | 78.79 | 76.47 | 0.001** |
| Initial lactate mmol/L | 0.77 | 3.30 | 70.59 | 72.73 | 0.015** |
| Multivariate analysis1 | |||||
| Biomarker | Odds ratio | Standard error | Z score | P-value | 95% CI |
| NLR | 5.1 | 3.82 | 2.17 | 0.03** | 1.17–22.16 |
| Lactate clearance (%) | 7.4 | 5.49 | 2.7 | 0.007** | 1.79–31.67 |
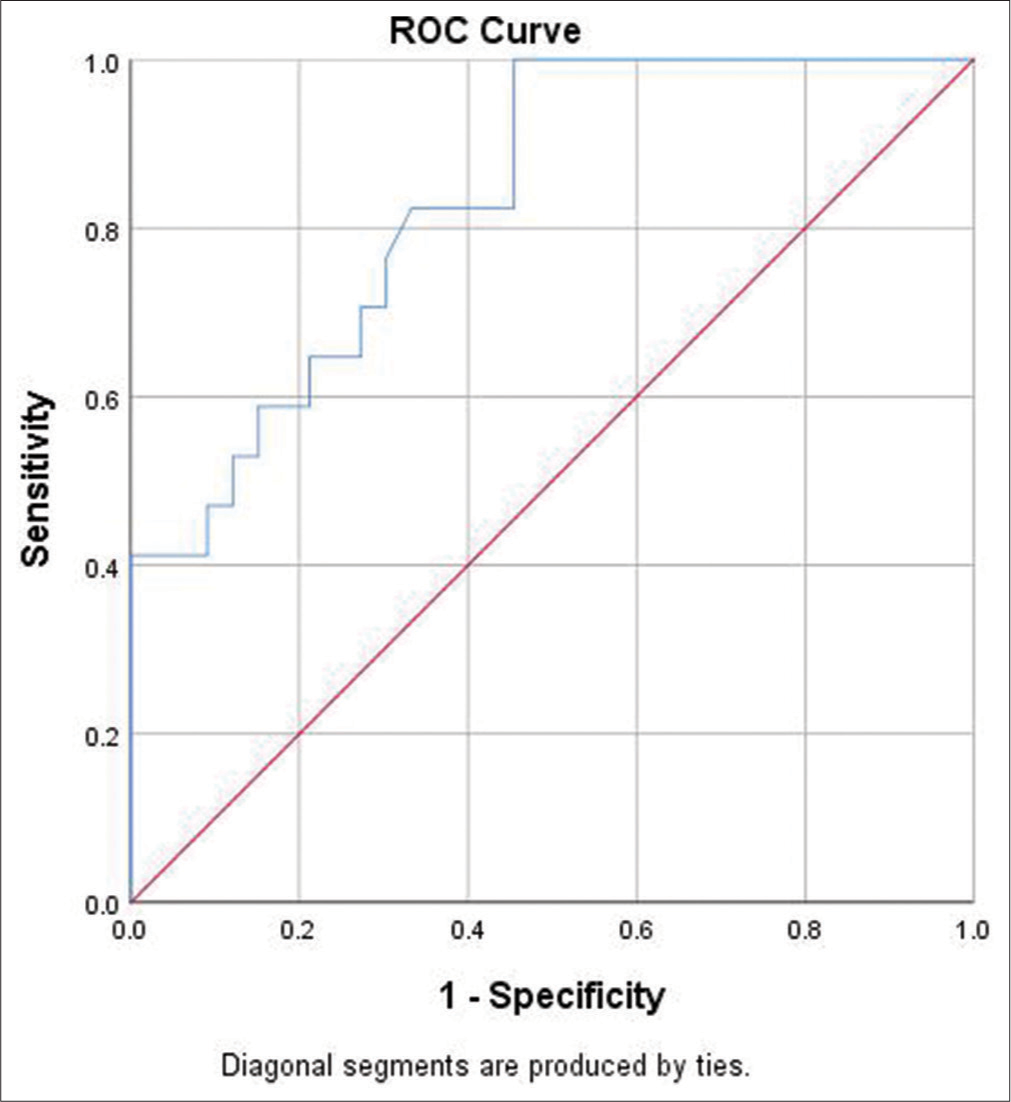
- Receiver operating curve (ROC) of neutrophil-tolymphocyte ratio.
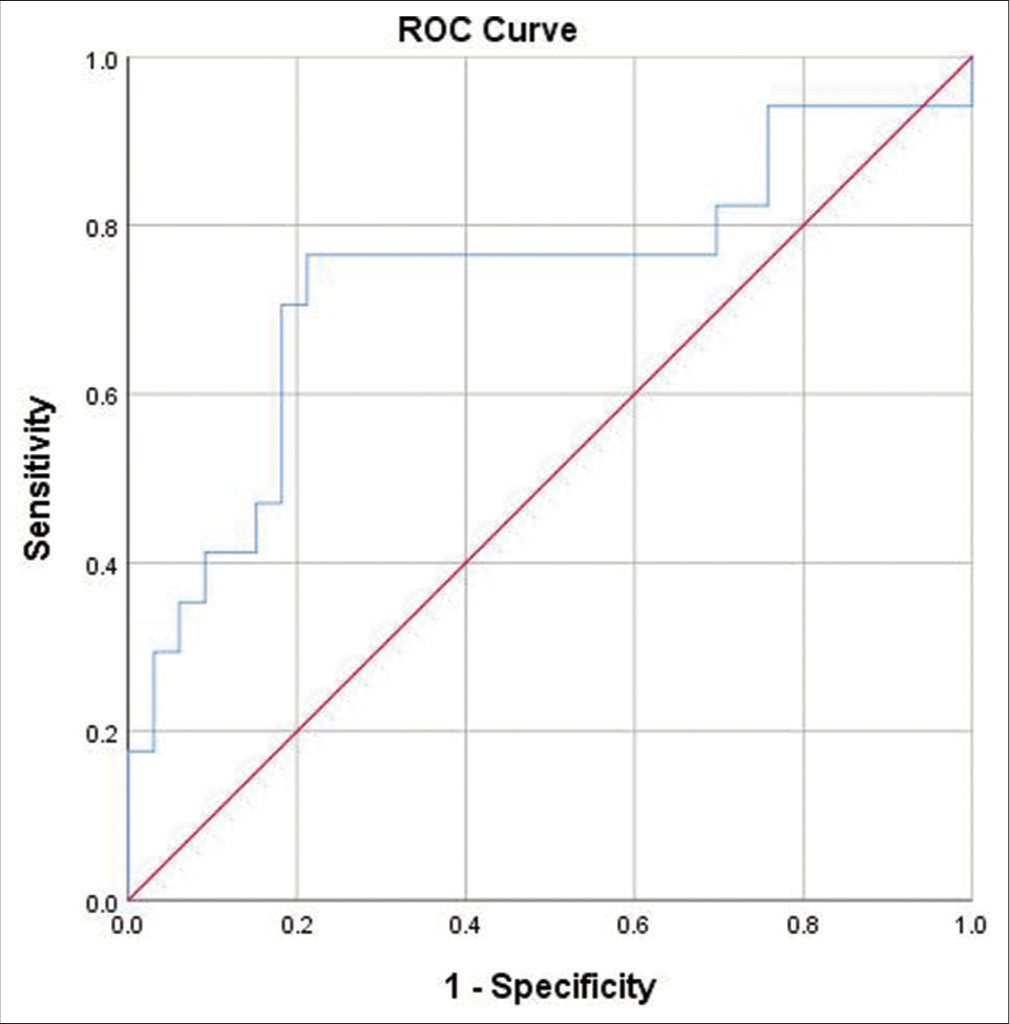
- Receiver operating curve of lactate clearance. ROC: Receiver operating curve.
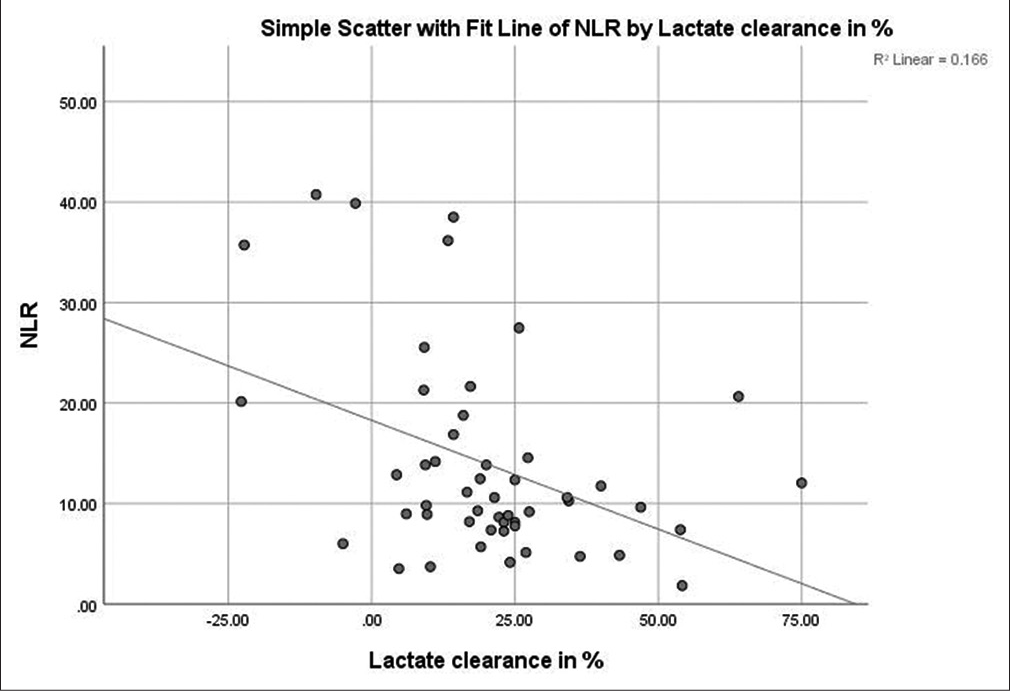
- Correlation between lactate clearance and neutrophil-tolymphocyte ratio (NLR).
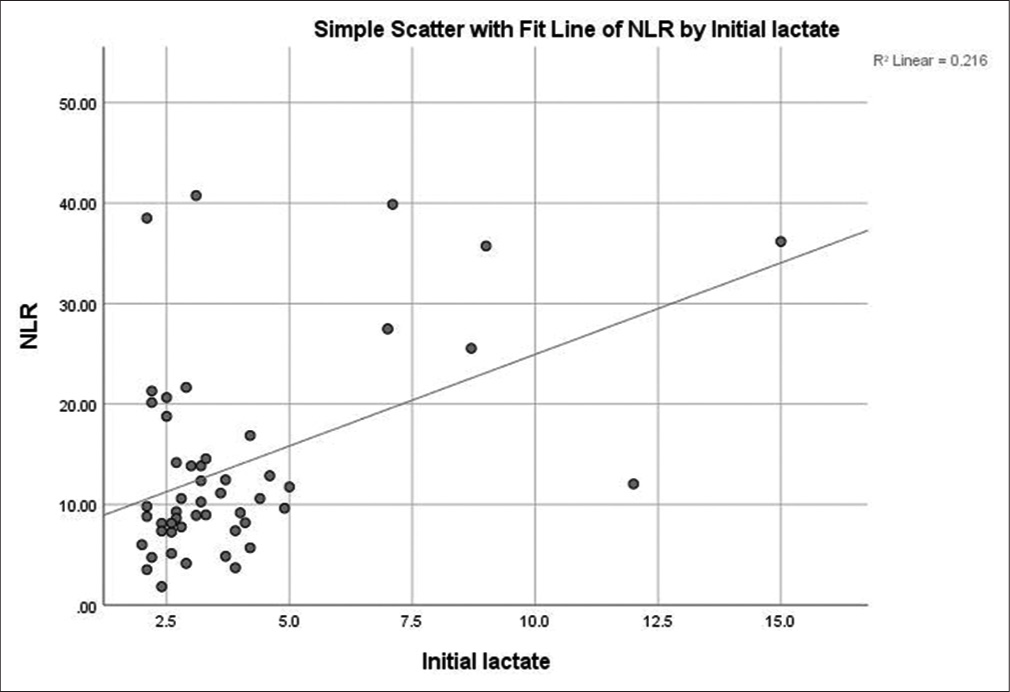
- Correlation between initial lactate and neutrophil-tolymphocyte ratio (NLR).
DISCUSSION
This single center and prospective observational study revealed that NLR and LC predicted 28-day mortality with moderate reliability. Univariate analysis with optimum cutoff value of ≥11.13 for NLR, mortality could be predicted with nearly 71% sensitivity and 72% specificity (AUROC 0.87). Similarly, with a cutoff level of ≥17.07%, LC had 75.8% sensitivity and 76.5% specificity in predicting mortality (AUROC 0.73). However, their combination in multivariate analysis did not offer extra predictive accuracy (AUROC 0.82). NLR and LC were also modestly correlated among themselves. Our study had almost 34% mortality, which was similar to those reported in two other studies.[13,14]
NLR is a simple and rapid tool used to stratify patients according to their disease severity. Due to any physiological stress, for example, sepsis, trauma, catecholamines, and steroids can lead to neutrophilia, both absolute (increased bone marrow production) and relative (peripheral to central migration). Simultaneously, cortisol-induced lymphopenia and sepsis-induced lymphocyte apoptosis cause ALC to fall. Due to the above factors, the NLR rises and the degree of rise correlates with the severity of underlying infection.[8] Higher NLR was associated with worse functional outcome, in patients presenting with intracerebral hemorrhage in the ED, indicating that higher degrees of stress lead to higher NLR (AUROC ~0.8).[15]
One previous study reported that, NLR ≥14.08 was able to predict survival with almost 78% sensitivity and 50% specificity (AUROC 0.634) in sepsis patients.[13] Another study reported higher NLR cutoff ≥23.8 (AUROC 0.695) for predicting mortality. Our study revealed similar finding but with lower cutoff levels (Univariate analysis). Heterogeneity of study population and disease severity could have accounted for such different levels. Despite a lower cutoff, our study revealed similar sensitivity ~71% and even higher specificity ~72%, as compared to Liu et al.[13] Except NLR, difference in age and disease severity also accounted for worse outcome in sepsis patients.[16]
Similarly, in our study, non-survivors had greater disease severity, requirement of mechanical ventilation, and vasopressors support; however, they had similar age distribution. NLR remained an independent predictor of mortality, even after adjustment.
Serum lactate is still used as a surrogate marker of tissue hypoperfusion. Tissue hypoxia leads to anaerobic metabolism and, thereby, increased serum lactate: Pyruvate ratio. Therefore, raised serum lactate and its reduced utilization (lower LC) are ominous signs in patients with sepsis, as it predicts mortality. Elevated serum lactate ≥2.99 mmol/L levels were nearly 83% sensitive and 55% specific in predicting sepsis-related mortality (AUROC 0.7). Raised serum lactate ≥4 mmol/L predicted mortality in patients presenting to ED as well as in ICU.[17,18] The importance of raised serum lactate was highlighted in the earlier definition of “severe sepsis,” where serum lactate ≥4 mmol/L predicted worse outcomes.[19] In our study, non-survivors had significantly higher serum lactate. The cutoff used in our study was somewhere in between the above-mentioned values, that is, 3.3 mmol/L (AUROC 0.77) [Figure 6]. However, a single-elevated serum lactate value can be erroneously interpreted as abnormal, as endogenous catecholamines and liver dysfunction can lead to falsely elevated serum lactate. Therefore, the trend of serum lactate and LC carry somewhat better prognostic significance. While, higher LC was associated with better survival, different cutoff levels have been proposed till date, ranging from 10 to 50%.[10,20] One study reported complete LC, that is, 100% LC as the best predictor of survival.[12] Our study revealed that LC ≤17.07% was best as well as an independent predictor of mortality (AUROC 0.73). A modest correlation existed between NLR versus LC (r = 0.358) and NLR versus serum lactate (r = 0.313), which was similar to the study by Liu et al.[13]
- Receiver operating curve (ROC) of initial lactate. ROC: Receiver operating curve.
Liu et al.,[12] also reported better predictive power with combination of NLR and serum lactate.[13] However, our study failed to demonstrate any benefit of such combination. As such, we used a lower cutoff for NLR, which resulted in greater sensitivity as compared to Liu’s study. Second, we used LC instead of serum lactate for combination with NLR.
Other than being an observational study which is fraught with risk of biases, our study had limited sample size. Despite a small sample size, our study showed fair reliability of various markers in predicting mortality, and better post hoc power (>80%) as compared to Liu et al. (post hoc power 5.6%).[13] Second, we accounted for major confounders related to mortality. It is intuitive to think that other confounders could be present, which if included, could change the result. We evaluated all-cause mortality and not disease or time (early vs. late) specific mortality. Third, data on culture positivity and use of antibiotics were not included. Finally, combined efficacy of NLR and serum lactate in predicting mortality was not evaluated. Indeed, this was a small feasibility study not aimed to detect causality.
CONCLUSION
In patients presenting with features of sepsis in the ED, NLR, serum lactate, and LC were all associated with 28-day survival. Among these, NLR (with cutoff ≥11.13) performed better (AUROC 0.87) than serum lactate (cutoff ≥3.3 mmol/L, AUROC 0.77) and LC (cutoff ≥17.07%, AUROC 0.73) and after adjusting for confounders, NLR and LC independently predicted mortality. Therefore, the above simple and yet rapid markers can predict outcome with fair reliability, which can be used to triage patients and tailor better treatments.
Ethical approval
The research/study approved by the Institute Ethics Committee of All India Institute of Medical Sciences, New Delhi, India, number IECPG-665/January 31, 2018, dated January 31, 2018.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Peripheral blood neutrophil-to-lymphocyte ratio as a predictor of functional outcomes in patients with hemorrhagic stroke. Indian J Crit Care Med. 2022;26:18-22.
- [CrossRef] [PubMed] [Google Scholar]
- Neutrophil to lymphocyte ratio: An emerging marker of the relationships between the immune system and diseases. Int J Mol Sci. 2022;23:3636.
- [CrossRef] [PubMed] [Google Scholar]
- Surviving sepsis campaign: International guidelines for management of sepsis and septic shock 2021. Crit Care Med. 2021;49:e1063-143.
- [Google Scholar]
- The complete blood count to diagnose septic shock. J Thorac Dis. 2020;12(Suppl 1):S16-21.
- [CrossRef] [PubMed] [Google Scholar]
- Hospital incidence and mortality rates of sepsis: An analysis of hospital episode (DRG) statistics in Germany from 2007 to 2013. Deutsch Ärztebl Int. 2016;113:159-66.
- [CrossRef] [PubMed] [Google Scholar]
- Severe hyperlactatemia, lactate clearance and mortality in unselected critically ill patients. Intensive Care Med. 2016;42:202-10.
- [CrossRef] [PubMed] [Google Scholar]
- Early lactate-guided therapy in intensive care unit patients: A multicenter, open-label, randomized controlled trial. Am J Respir Crit Care Med. 2010;182:752-61.
- [CrossRef] [PubMed] [Google Scholar]
- An evaluation of serial blood lactate measurement as an early predictor of shock and its outcome in patients of trauma or sepsis. Indian J Crit Care Med. 2009;13:66-73.
- [CrossRef] [PubMed] [Google Scholar]
- The surviving sepsis campaign: Results of an international guideline-based performance improvement program targeting severe sepsis. Crit Care Med. 2010;38:367-74.
- [CrossRef] [PubMed] [Google Scholar]
- Predictors of survival in sepsis: What is the best inflammatory marker to measure? Curr Opin Infect Dis. 2012;25:328-36.
- [CrossRef] [PubMed] [Google Scholar]
- Prognostic significance of neutrophil-to-lymphocyte ratio in patients with sepsis: A prospective observational study. Mediat Inflamm. 2016;2016:8191254.
- [CrossRef] [PubMed] [Google Scholar]
- Neutrophil-lymphocyte ratio and plasma lactate predict 28-day mortality in patients with sepsis. J Clin Lab Anal. 2019;33:e22942.
- [CrossRef] [PubMed] [Google Scholar]
- Mortality of adult patients due to sepsis and septic shock in South Korea: A systematic review and meta-analysis. Clin Exp Emerg Med. 2023;10:157-71.
- [CrossRef] [PubMed] [Google Scholar]
- Early lactate clearance is associated with improved outcome in severe sepsis and septic shock. Crit Care Med. 2004;32:1637-42.
- [CrossRef] [PubMed] [Google Scholar]
- Whole blood lactate kinetics in patients undergoing quantitative resuscitation for severe sepsis and septic shock. Chest. 2013;143:1548-53.
- [CrossRef] [PubMed] [Google Scholar]
- Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368-77.
- [CrossRef] [PubMed] [Google Scholar]
- Serum lactate as a predictor of mortality in emergency department patients with infection. Ann Emerg Med. 2005;45:524-8.
- [CrossRef] [PubMed] [Google Scholar]
- Predictive value of procalcitonin, interleukin-6, and C-reactive protein for survival in postoperative patients with severe sepsis. J Crit Care. 2011;26:54-64.
- [CrossRef] [PubMed] [Google Scholar]







