Translate this page into:
Factors influencing IgG response against SARS-CoV-2: A quantitative serological survey among healthcare workers of a COVID-19 dedicated health facility in India
*Corresponding author: Bijit Biswas, Department of Community and Family Medicine, All India Institute of Medical Sciences, Phulwarisharif, Patna - 801 507, Bihar, India. drbijitbiswas@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mahto M, Biswas B, Banerjee A, Kumar S, Agarwal N, Singh PK. Factors influencing IgG response against SARSCoV-2: A quantitative serological survey among healthcare workers of a COVID-19 dedicated health facility in India. Indian J Med Sci 2021;73(2):147-54.
Abstract
Objectives:
The objectives of the study were to explore the factors influencing serum IgG response against severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) among healthcare workers (HCWs) of a tertiary healthcare facility in India.
Material and Methods:
It was a monocentric, observational study during the month of September 2020. In the study, a cross-sectional quantitative serological assessment of IgG response against SARS-CoV-2 among HCWs of All India Institute of Medical Sciences (AIIMS), Patna, Bihar, was done using a chemiluminescent immunoassay (CLIA) platform named “ADVIA Centaur COV2G.” Statistical Package for the Social Sciences (SPSS) (version 22.0) was used for data analysis.
Results:
Among the study subjects, 761 (82.8%) had detectable serum IgG traces against SARS-CoV-2 with median (interquartile range [IQR]) of 0.03 (0.01–0.08). Those who were male by gender (spearman rho correlation co-efficient [ρ] = 0.08; P ≤ 0.05), technician (ρ= 0.07; P ≤ 0.05), attendant (ρ= 0.19; P ≤ 0.01), and sanitary staff (ρ= 0.13; P ≤ 0.01) by occupation, posted in laboratories (ρ= 0.09; P ≤ 0.01), had prior SARS-CoV-2 infection (ρ= 0.26; P ≤ 0.01), used to take steam inhalation (ρ= 0.10; P ≤ 0.01), preferred non-vegetarian diet (ρ= 0.10; P ≤ 0.01), consumed azithromycin (ρ= 0.13; P ≤ 0.01), zinc (ρ= 0.08; P ≤ 0.05) had significantly higher whereas doctors (ρ= −0.10; P ≤ 0.01), and nurses (ρ= −0.16; P ≤ 0.01) had significantly lower serum IgG response against SARS-CoV-2 compared to others.
Conclusion:
Gender, occupation, place of posting, prior SARS-CoV-2 infection, use of steam inhalation, diet preference, consumption of azithromycin, and zinc emerged as significant attributes of serum IgG response against SARS-CoV-2 among the study subjects.
Keywords
SARS-CoV-2
COVID-19
IgG antibody
Healthcare workers
INTRODUCTION
Coronavirus disease-19 (COVID-19) is creating a havoc menace throughout the world with about 40 million and over a million reported cases and deaths, respectively. In terms of total number of reported COVID-19 cases Southeast Asian region is the third most affected region in the pandemic following Americas and Europe. India is the largest hotspot of COVID-19 in the Asian region as the country has reported over 88% cases from the region.[1] The causative organism of COVID-19 is severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) which mainly gets transmitted by contacts, droplets, and fomites.[2]
Antibody response in a SARS-CoV-2 infected person generally gets triggered after 6–8 days of the illness with median observed seroconversion time of 11 and 14 days for IgM and IgG, respectively. Although SARS-CoV-2 differs from its predecessors (i.e., SARS-CoV-1) in terms of magnitude and longevity of antibody response. As per the existing literature antibody response in SARS-CoV-2 is proportional to the disease severity with reduction and even disappearance documented post 3 months of the disease onset.[3-5]
Serological survey for an infectious disease is generally done for risk quantification in a particular community or group through quantitative and/or qualitative assessment of serum antibody response (especially IgG) of that specific disease. In case of COVID-19 its role becomes more evident as still it is a new disease with uncertainties in immune response. It is also useful for assessment of geographical spread of an infectious disease in a vulnerable community or group as it not only detects protective antibody level in the reported cases but also in missed or unreported ones.[6,7]
Healthcare workers (HCWs) are at utmost risk of contracting SARS-CoV-2 infection due to their job profile. They regularly need to deal with COVID-19 (suspected or confirmed) cases and/or their body fluids. There are very few prior serological surveys on SARS-CoV-2 reported among HCWs with even limited information on the Indian context. Those which existed mainly focused on qualitative serological assessment (i.e., seroprevalence)[8-11] ignoring the quantitative component which is equally important. Thus, the current quantitative serological survey was planned to explore the factors influencing serum IgG response against SARS-CoV-2 among HCWs of a COVID-19 dedicated tertiary care health facility of eastern India.
MATERIAL AND METHODS
It was a monocentric, observational study during the month of September, 2020. In the study a cross-sectional quantitative serological assessment of IgG response against SARS-CoV-2 among HCWs of All India Institute of Medical Sciences (AIIMS), Patna, Bihar, India, was done. AIIMS-Patna is a premier institute which offers quality medical education and patient care. The institute is providing best possible care for the attending COVID-19 patients since the very onset of the pandemic and later deemed to be a COVID-19 dedicated health facility. At present, the institute has approximately 60 intensive care unit (ICU) and 460 general beds with 3150 HCWs dedicated for COVID care.
Assuming the expected maximum standard deviation of serum IgG response against SARS-CoV-2 to be 1.3 (approximately one-fourth of the antibody level range of 1.1–6.2 reported by a prior study conducted among HCWs of USA[5]), adjusting for finite population size of 3150, the final minimum sample size for the study was calculated to be 541 with 95% confidence and a precision of 0.1. The sample size was calculated using “statulator,” an online sample size calculator. During the study period, all the HCWs working in AIIMS-Patna were send individualized study invitation message through short message service (SMS) and/or email. These study invitations also indicated their scheduled date and venue for IgG testing against SARS-CoV-2. On attendance of the designated area of the outpatient department (OPD) for testing, all the HCWs were provided with a structured schedule and consent form for obtaining their background characteristics and informed written consent for participation, respectively. Following this, 5 ml blood sample of the study subjects was collected for estimating their serum IgG response against SARSCoV-2. Test results were made available to the study subjects within 24 h of blood sample collection in a designated report dispensing counter in OPD and the hospitals health management and information system (HMIS). Overall, 967 study subjects participated in the study out of which data of 919 HCWs were finally analyzed. The details of the selection process are depicted in Figure 1.

- Flowchart showing selection of the study subjects.
The structured schedule used for the study contained following items: Socio-demography (age in years, gender [female/ male]), occupational cardinals (occupation [doctor/nurse/ technician/account staff/attendant/sanitary staff/others], place of posting [triage area/wards/ICUs/laboratories/others], whether exposed to confirmed COVID-19 case or their body fluids during duty [no/yes], if yes average duration of exposure in per duty shift [in hours], whether personal protective equipment [PPE] used during duty [no/yes]), personal history (currently smokes [no/yes], consumes alcohol [no/yes], whether suffering from any chronic comorbidity [no/yes], if yes name of comorbidity, diet preference [vegetarian/non-vegetarian], history of prior SARS-CoV-2 infection detected by real-time reverse-transcriptase-polymerase chain reaction [RTPCR] or rapid antigen test for the disease [no/yes], if yes date of first SARS-CoV-2 positive report, history of influenza like illness [ILI] in last 8 months [no/yes], if yes the date of 1st day of initial ILI episode) and practices related to the disease prevention in last 8 months (whether used masks other than workplace [no/yes], sanitizer other than workplace [no/ yes], steam inhalation [no/yes], used to drink hot beverages such as hot water, tea and coffee [no/yes], consumed hydroxychloroquine (HCQ) [no/yes], azithromycin [no/yes], zinc [no/yes], multivitamin [no/yes], Vitamin C [no/yes], and Vitamin E [no/yes]).
Some operational definitions used in the study were as following:
Full PPE: Those who opined that they use N-95 mask, goggles, body gown, double layered gloves, and shoe cover during their duty were considered as using full PPE.
Serum IgG response against SARS-CoV-2: It was measured by a qualitative and semi-quantitative chemiluminescent immunoassay (CLIA) known as “ADVIA Centaur COV2G”. This immunoassay can detect serum IgG response against SARS-CoV-2 between 0 and 20 indices with excellent sensitivity (100.0%) and specificity (99.8%) as reported by the manufacturer.[12]
Ethical issues
The study was conducted abiding by the declaration of Helsinki and after obtaining ethical clearance of the Institutional Ethics Committee (IEC) of AIIMS-Patna (Ref. No. - AIIMS/Pat/IEC/2020/575). Before enrolment of each study subject their informed written consent was taken. Before analysis the study data was intentionally blind-folded to ensure anonymity.
Statistical analysis
IBM Statistical Package for the Social Sciences (SPSS) (Chicago, USA) (version 22) was used for data analysis. At first, either Mann–Whitney U-test or Kruskal-Wallis H test as per degree of freedom of the independent variables was done to find out significant attributes affecting serum IgG response against SARS-CoV-2 among the HCWs. Then to quantify the strength of association between serum IgG response and its various attributes Spearman rho correlation was done. The strength of association was assessed by Spearman rho correlation coefficient (ρ). For all the analysis minimum acceptable confidence level (α) was deemed to be 0.95.
RESULTS
The median age of the participating HCWs in our study was 29 years with interquartile range (IQR) of 26–32 years (range: 20–56 years). Majority of them were nurse by occupation (56.9%) and posted in wards (47.3%). Majority of the study subjects (72.8%) have reported direct exposure to confirmed COVID-19 cases and/or their body fluids during their duty hours with median exposure time per duty shift of 7 h with IQR (6–9 h) (range: 1–12 h). Majority of them have used full PPE during their duty hours (72.6%). About one-tenth of them (8.6%) have reported prior SARSCoV-2 infection with median duration since first SARSCoV-2 positive report of 50 days (IQR: 27–58 days, range: 2–73 days). Similarly, 7.5% of them have reported ILI in past 8 months with median duration since 1st day of initial episode of 37 days (IQR: 16–62 days, range: 0–238 days). Very few of them (4%) reported to have chronic comorbidity with hypothyroidism (2.0%) being the most common, followed by diabetes (0.7%) and hypertension (0.5%). Among the study subjects 761 (82.8%) had detectable serum IgG traces against SARS-CoV-2 with median (interquartile range [IQR]) of 0.03 (0.01–0.08). Gender, occupation, place of posting, prior SARS-CoV-2 infection, use of steam inhalation, diet preference, consumption of azithromycin, and zinc were found to be significantly associated with serum IgG response against SARS-CoV-2 among the study subjects [Figure 2 and Table 1].
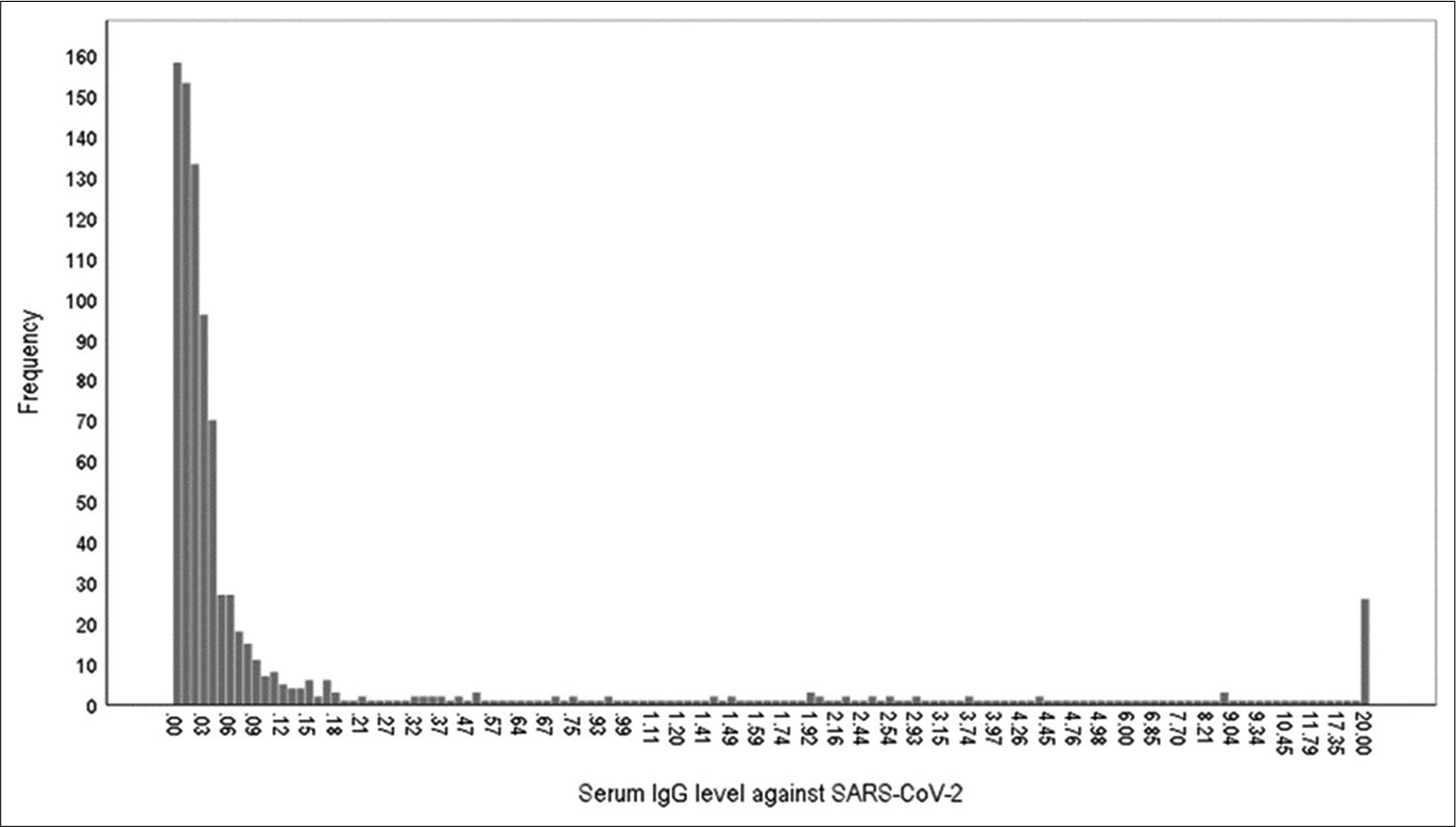
- Bar chart showing the distribution of healthcare workers as per their serum IgG response against SARS-CoV-2: (n=919).
| Variable | Total | Serum IgG response against SARS-CoV-2 | P-value |
|---|---|---|---|
| n(%) | Median (IQR) | ||
| Age in years | |||
| <30 (median 29 years) | 515 (56.0) | 0.03 (0.01–0.07) | 0.284* |
| ≥30 | 404 (44.0) | 0.02 (0.01–0.09) | |
| Gender | |||
| Male | 471 (51.3) | 0.03 (0.01–0.17) | 0.017* |
| Female | 448 (48.7) | 0.02 (0.01–0.06) | |
| Occupation | |||
| Doctor | 124 (13.5) | 0.02 (0.00–0.04) | 0.000# |
| Nurse | 523 (56.9) | 0.05 (0.02–0.05) | |
| Technician | 41 (4.5) | 0.06 (0.01–0.82) | |
| Account staff | 20 (2.2) | 0.04 (0.00–1.89) | |
| Attendant | 118 (12.8) | 0.06 (0.02–1.62) | |
| Sanitary staff | 31 (3.4) | 0.11 (0.03–1.77) | |
| Others | 62 (6.7) | 0.03 (0.01–0.74) | |
| Place of posting: (n=839) | |||
| Triage | 58 (6.9) | 0.02 (0.01–0.08) | 0.047# |
| Wards | 397 (47.3) | 0.03 (0.01–0.08) | |
| ICUs | 249 (29.7 | 0.03 (0.01–0.05) | |
| Laboratories | 42 (5.0) | 0.06 (0.01–2.11) | |
| Others | 93 (11.1) | 0.03 (0.01–0.99) | |
| Exposure to confirmed COVID-19 cases or their body fluids during duty: (Yes) | 669 (72.8) | 0.03 (0.01–0.07) | 0.116* |
| Hours of exposure to confirmed COVID-19 cases or their body fluids during duty: (≥6 hours) (median) (n=669) | 617 (92.2) | 0.03 (0.01–0.07) | 0.163* |
| Used Full PPE: (Yes) (n=840) | 610 (72.6) | 0.02 (0.01–0.07) | 0.105* |
| Had prior COVID-19 infection: (Yes) | 79 (8.6) | 1.01 (0.03–7.70) | 0.000* |
| Days since first COVID-19 positive report: (≥50 days) (median) (n=70) | 38 (54.2) | 0.69 (0.03–8.40) | 0.335* |
| Had ILI in past 8 months: (Yes) | 69 (7.5) | 0.03 (0.01–1.44) | 0.088* |
| Days since 1stday of initial ILI episode: (≥37 days) (median) (n=31) | 16 (51.6) | 0.04 (0.02–1.45) | 0.662* |
| Had comorbidity: (No) | 882 (96.0) | 0.03 (0.01–0.08) | 0.545* |
| Used to smoke: (Yes) | 33 (3.6) | 0.02 (0.00–0.04) | 0.059* |
| Used to drink alcohol: (Yes) | 31 (3.4) | 0.03 (0.01–0.06) | 0.894* |
| Used to drink hot beverages: (Yes) | 808 (87.9) | 0.03 (0.01–0.08) | 0.056* |
| Used to take steam inhalation: (Yes) | 112 (12.2) | 0.03 (0.01–0.90) | 0.003* |
| Used mask other than workplace: (Yes) | 899 (97.8) | 0.03 (0.01–0.08) | 0.197* |
| Used sanitiser other than workplace: (Yes) | 903 (98.3) | 0.03 (0.01–0.08) | 0.242* |
| Diet preference: (n=808) | |||
| Vegetarian | 244 (30.2) | 0.02 (0.01–0.05) | 0.005* |
| Non-vegetarian | 564 (69.8) | 0.03 (0.01–0.09) | |
| Have consumed HCQ: (Yes) | 106 (11.5) | 0.02 (0.01–0.08) | 0.079* |
| Have consumed Azithromycin: (Yes) | 138 (15.0) | 0.05 (0.01–1.59) | 0.000* |
| Have consumed Zinc: (Yes) | 49 (5.3) | 0.05 (0.01–2.56) | 0.019* |
| Have consumed Multivitamin: (Yes) | 96 (10.4) | 0.03 (0.01–0.74) | 0.393* |
| Have consumed Vitamin C: (Yes) | 182 (19.8) | 0.03 (0.01–0.97) | 0.086* |
| Have consumed Vitamin E: (Yes) | 43 (4.7) | 0.04 (0.01–0.80) | 0.112* |
Those who were male by gender (spearman rho correlation co-efficient [ρ] = 0.08; P ≤ 0.05), technician (ρ= 0.07; P ≤ 0.05), attendant (ρ= 0.19; P ≤ 0.01), and sanitary staff (ρ= 0.13; P ≤ 0.01) by occupation, posted in laboratories (ρ= 0.09; P ≤ 0.01), had prior SARS-CoV-2 infection (ρ= 0.26; P ≤ 0.01), used to take steam inhalation (ρ= 0.10; P ≤ 0.01), preferred non-vegetarian diet (ρ= 0.10; P ≤ 0.01), consumed azithromycin (ρ= 0.13; P ≤ 0.01), zinc (ρ= 0.08; P ≤ 0.05) had significantly higher whereas doctors (ρ= −0.10; P ≤ 0.01), and nurses (ρ= −0.16; P ≤ 0.01) had significantly lower serum IgG response against SARS-CoV-2 compared to others. No significant effect of days since SARS-CoV-2 positive report and initial ILI episode on serum IgG response against the disease was observed [Figures 3 and 4; Table 2].
| Variable | Correlation Co-efficient (ρ) | P-value |
|---|---|---|
| Age in years: (Increasing) | −0.03 | 0.416 |
| Gender: Females versus Males | 0.08* | 0.017 |
| Occupation | ||
| Others versus Doctors | −0.10** | 0.003 |
| Others versus Nurses | −0.16** | 0.000 |
| Others versus Technicians | 0.07* | 0.032 |
| Others versus Account staffs | 0.03 | 0.426 |
| Others versus Attendants | 0.19** | 0.000 |
| Others versus Sanitary staffs | 0.13** | 0.000 |
| Place of posting: (n=839) | ||
| Others versus Triage | −0.02 | 0.571 |
| Others versus Wards | −0.01 | 0.840 |
| Others versus ICUs | −0.05 | 0.102 |
| Others versus Laboratories | 0.09** | 0.008 |
| Exposure to confirmed COVID-19 cases or their body fluids during duty: (No vs. Yes) | −0.05 | 0.116 |
| Hours of exposure to confirmed COVID-19 cases or their body fluids during duty: (Increasing) (n=669) | −0.01 | 0.986 |
| Used Full PPE: (No vs. Yes) (n=840) | −0.06 | 0.105 |
| Had prior COVID-19 infection: (Yes) | 0.26** | 0.000 |
| Days since first COVID-19 positive report: (Increasing) (n=70) | −0.14 | 0.256 |
| Had ILI in past eight months: (No vs. Yes) |
0.06 | 0.088 |
| Days since first day of initial ILI episode: (Increasing) (n=31) | 0.17 | 0.373 |
| Had co-morbidity: (No vs. Yes) | 0.02 | 0.545 |
| Used to smoke: (No vs. Yes) | −0.06 | 0.059 |
| Used to drink alcohol: (No vs. Yes) | −0.00 | 0.894 |
| Used to drink hot beverages: (No vs. Yes) |
−0.06 | 0.056 |
| Used to take steam inhalation: (No vs. Yes) |
0.10** | 0.003 |
| Used mask other than workplace: (No vs. Yes) | 0.04 | 0.197 |
| Used sanitizer other than workplace: (No vs. Yes) | −0.04 | 0.242 |
| Diet preference: (Vegetarians vs. Non-vegetarians) (n=808) | 0.10** | 0.005 |
| Have consumed HCQ: (No vs. Yes) | −0.06 | 0.079 |
| Have consumed Azithromycin: (No vs. Yes) | 0.13** | 0.000 |
| Have consumed Zinc: (No vs. Yes) | 0.08* | 0.019 |
| Have consumed Multivitamin: (No vs. Yes) |
0.03 | 0.394 |
| Have consumed Vitamin C: (No vs. Yes) |
0.06 | 0.086 |
| Have consumed Vitamin E: (No vs. Yes) |
0.05 | 0.112 |
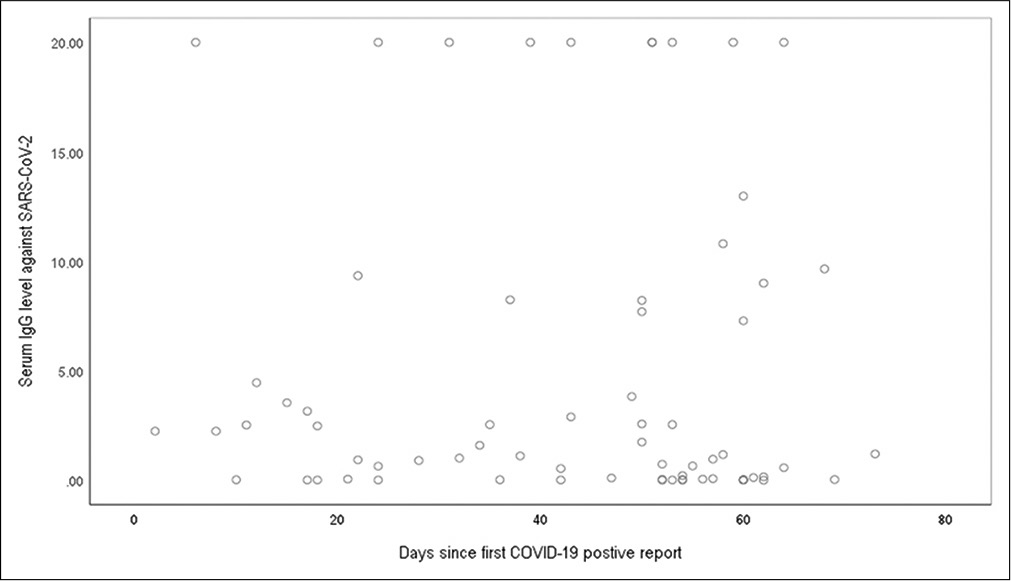
- Scatter plot showing distribution of the COVID-19 positive healthcare workers as per days since first positive report and serum IgG response against SARS-CoV-2: n=70.
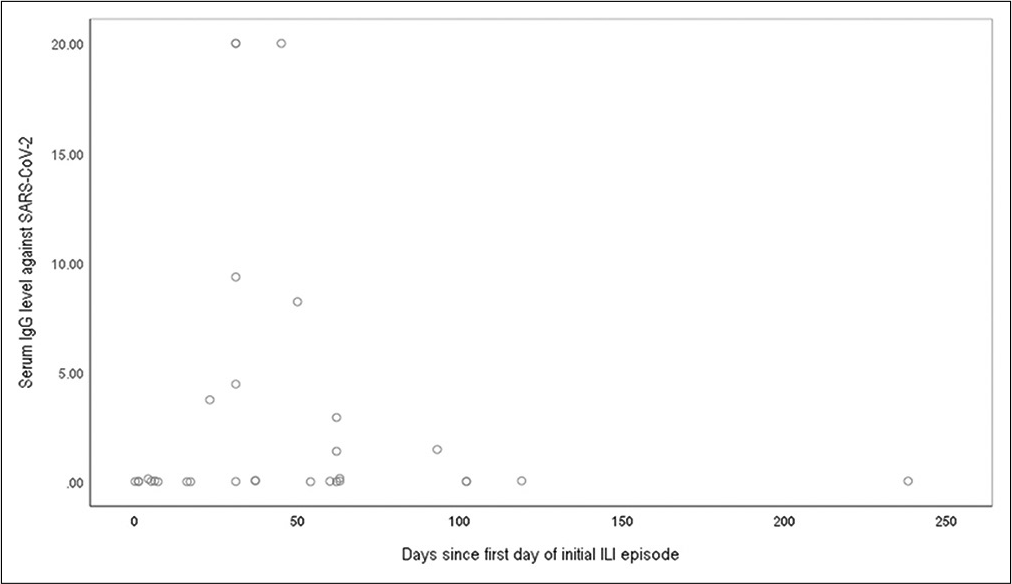
- Scatter plot showing distribution of the healthcare workers as per days since first day of initial influenza like illness (ILI) episode and their serum IgG response against SARS-CoV-2: n=31.
DISCUSSION
We found that males had significantly higher IgG response against SARS-CoV-2 compared to females. This was in concordance with an Italian study by Amendola et al.[10] which reported higher seroprevalence of IgG against SARSCoV-2 among males compared to females. In Indian society, males have more freedom for mobility and they are often involved in various outdoor activities (i.e., purchasing of goods for household needs) in comparison to their female counterparts. These might have increased their chances of contracting SARS-CoV-2 infection and thereby development of immunity against the disease. Moreover, proportion of Indian women suffering from anemia is twice as more in comparison to their male counterparts. Anemia is a known influencer of immune response to any pathogen.[13,14]
Concerning occupation, nurses and doctors were found to have lower whereas technician, attendant, and sanitary staff were found to have higher IgG response against SARS-CoV-2 in comparison to others. Here professional training of the study subjects might have played a role as doctor and nurses are more likely to be trained in infection prevention and control (IPC) measures than others. Thus, doctors and nurses in the present study might have more stringently followed IPC measures than others which reduced their odds for infection and thereby immunity development. We found that those who were deployed in laboratories had higher IgG response against SARS-CoV-2 than others. This was similar with the observations of Amendola et al.[10] which have reported that those who were posted in pediatric intensive care and surgery in that study were more likely to be IgG seropositive against the disease. This might be because those who work in laboratories, intensive care, and surgery units are more likely to be in direct contact of a COVID-19 patient or their body fluids samples (i.e., throat or nasal swab for SARS-CoV-2 testing). Moreover, in these areas’ aerosol generating procedures (i.e., intubation, cardio-pulmonary resuscitation, throat, or nasal swab collection of SARS-CoV-2 testing) are commonly performed which increases the chances of aerosol mediated transmission. This might have increased risk of contracting infection in the HCWs working in these areas in comparison to others.
In our study, prior SARS-CoV-2 infection emerged as a significant influencer of serum IgG response against the disease. A study in Spain by Garcia-Basteiro et al.[8] reported similar observations in which HCWs who were previously diagnosed with COVID-19 by RTPCR have shown more likelihood to be IgM and/or IgG and/or IgA seropositive for the disease. In absence of effective vaccine contracting a disease infection is the only way for immunity development. Thus, this was an obvious observation. We observed that with increase in days since first SARS-CoV-2 positive report the serum IgG level against the disease declined. This was in concordance with a study in USA by Patil et al.[5] which recorded decline in serum antibody level against SARSCoV-2 of seropositive HCWs over 60 days. On the other hand, we did not find any association between history of ILI with serum IgG level against SARS-CoV-2. It was unlike observations in the Spain study[8] which found significant association between history of ILI and IgM and/or IgG and/ or IgA seropositivity. The reason of differences could be due to differences in the measures of outcome. The Spain study[8] determined attributes of IgM and/or IgG and/or IgA seropositivity whereas we investigated factors influencing serum IgG response against SARS-CoV-2. Similarly, we did not find any association between duration since 1st day of initial ILI episode and serum IgG response which might be due to underreporting of that data (only 44.9% persons with ILI history have reported it).
We found that HCWs who used to take steam inhalation had higher IgG response against SARS-CoV-2. Steam inhalation is a commonly used traditional remedy for respiratory conditions all over the world.[15] Although the effect of steam inhalation on immunogenesis is not yet well understood. It maybe through raising of the body temperature (mimics fever in its recipient), which promotes immune response to a pathogen. However, it may be only an incidental finding as those who had respiratory symptoms during the pandemic might have only practiced it. We observed that those who preferred non-vegetarian diet had significantly higher IgG response against SARS-CoV-2 compared to vegetarians.
A prior meta-analysis by Craddock et al.[16] reported that vegetarians have lower serum inflammatory response to a pathogen compared to others. Moreover, non-vegetarians are more likely to consume quality (enriched in essential amino acids) and quantity of protein in comparison to vegetarians which is vital for an individual’s immune response to a pathogen and its integrity. In our study, those who consumed azithromycin had higher IgG response against SARS-CoV-2. Azithromycin is an antimicrobial with known immunomodulatory effects.[17] Similarly, we observed a positive correlation between zinc consumption and serum IgG response against SARS-CoV-2. Zinc is also documented to have immunomodulatory effect in COVID-19 and its deficiency was reported to be associated with severe form of the disease.[18] Although, in our study, positive effect of consumption of azithromycin and zinc on serum IgG response against SARS-CoV-2 might be incidental. There are possibilities that those who were diagnosed with the disease or had prior ILI episode might have only consumed them.
Implications of the study findings
The study investigated quantitative IgG response against SARS-CoV-2 and its various influencers among HCWs of a COVID dedicated tertiary healthcare facility. None of our study subjects were part of any SARS-CoV-2 vaccine trial either during or before the study period. Hence, the research would help policymakers to get an estimate of the naturally acquired immunity level of the HCWs and its various associates in the pre-vaccination era. Further, the study found practice of steam inhalation as beneficial for immunogenesis against the disease. Moreover, non-vegetarians were found to have more IgG response against the disease compared to others. Thus, practice of steam inhalation and inclusion of animal proteins in the diet of the vegetarians (i.e., milk, butter, and ghee) may be promoted among HCWs depending on its feasibility and acceptability. This might help to upkeep immunity level of the valuable healthcare workforce till availability of effective vaccines against the disease.
In limitations; first, the study design was cross-sectional which cannot ascertain causal role of the found correlates with serum IgG response against SARS-CoV-2. Second, the study schedule was self-administered to the study subjects with recall period of 8 months. Hence, there might be reporting, recall, and social desirability related biases. Third, we have invited all the HCWs of our institution for the study. Hence, there are possibilities that those who were working in more high-risk areas (i.e., ICUs) had current or prior SARS-CoV-2 infection and/or ILI symptoms might have more enrolled themselves for the study to know their immunity response against the disease. Finally, we used a semiquantitative method for serum IgG response estimation which can detect serum IgG level between 0 to 20 indices. All these factors limited external generalizability of our study findings to some extent.
CONCLUSION
Gender, occupation, place of posting, prior SARSCoV-2 infection, use of steam inhalation, diet preference, consumption of azithromycin, and zinc emerged as significant attributes affecting serum IgG response against SARS-CoV-2 among the study subjects. Serological surveillance for SARSCoV-2 may be a useful tool for tracking the progress of the COVID-19 pandemic and estimation of immunity response of more vulnerable population such as HCWs against the disease.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- WHO Coronavirus Disease (COVID-19) Dashboard (nd) 2020. Geneva: World Health Organization; Available from: https://www.covid19.who.int [Last accessed on 2020 Oct 29]
- [Google Scholar]
- Transmission of SARS-CoV-2: Implications for Infection Prevention Precautions (nd) Available from: https://www.who.int/news-room/commentaries/detail/transmission-ofsars-cov-2-implications-for-infection-prevention-precautions [Last accessed on 2020 Oct 29]
- [Google Scholar]
- What we know about the COVID-19 Immune Response: The Latest on COVID-19 Immunity and the Current Global Situation. Available from: https://www.who.int/docs/default-source/coronaviruse/risk-comms-updates/update-34-immunity-2nd.pdf?sfvrsn=8a488cb6_2 [Last accessed on 2020 Oct 29]
- [Google Scholar]
- European Centre for Disease Prevention and Control (nd) Available from: https://www.ecdc.europa.eu/en/covid-19/latest-evidence/immune-responses [Last accessed on 2020 Oct 15]
- [Google Scholar]
- Change in antibodies to SARS-CoV-2 over 60 days among health care personnel in Nashville, Tennessee. JAMA. 2020;324:1781-2.
- [CrossRef] [PubMed] [Google Scholar]
- Serology in the Context of COVID-19 (nd) Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/serology-in-the-context-of-covid-19 [Last accessed on 2020 Oct 30]
- [Google Scholar]
- Centers for Disease Control and Prevention Coronavirus Disease 2019 (COVID-19) 2020. Atlanta, Georgia: Centers for Disease Control and Prevention; Available from: https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/geographic-seroprevalence-surveys.html [Last accessed on 2020 Oct 30]
- [Google Scholar]
- Seroprevalence of antibodies against SARS-CoV-2 among health care workers in a large Spanish reference hospital. Nat Commun. 2020;11:3500.
- [CrossRef] [PubMed] [Google Scholar]
- Dynamics of SARS-CoV-2 RT-PCR positivity and seroprevalence among high-risk healthcare workers and hospital staff. J Hosp Infect. 2020;106:102-6.
- [CrossRef] [PubMed] [Google Scholar]
- Low seroprevalence of SARS-CoV-2 infection among healthcare workers of the largest children hospital in Milan during the pandemic wave. Infect Control Hosp Epidemiol. 2020;41:1468-9.
- [CrossRef] [PubMed] [Google Scholar]
- The prevalence of severe acute respiratory coronavirus virus 2 (SARS-CoV-2) Igg antibodies in intensive care unit (ICU) healthcare personnel (HCP) and its implications-a single-center, prospective, pilot study. Infect Control Hosp Epidemiol. 2020;12:1-2.
- [CrossRef] [PubMed] [Google Scholar]
- SARS-CoV-2 Igg Assay (nd) Available from: https://www.siemens-healthineers.com/en-in/laboratory-diagnostics/assays-by-diseases-conditions/infectious-disease-assays/cov2g-assay [Last accessed on 2020 Oct 29]
- [Google Scholar]
- Anaemia among men in India: A nationally representative cross-sectional study. Lancet Glob Health. 2019;7:e1685-94.
- [CrossRef] [Google Scholar]
- Anaemia, iron deficiency and susceptibility to infections. J Infect. 2014;69(Suppl 1):S23-27.
- [CrossRef] [PubMed] [Google Scholar]
- Closing evidence to practice gaps: an end to an attack of the vapours? Br J Gen Pract. 2016;66:118-9.
- [CrossRef] [PubMed] [Google Scholar]
- Vegetarian-based dietary patterns and their relation with inflammatory and immune biomarkers: A systematic review and meta-analysis. Adv Nutr. 2019;10:433-51.
- [CrossRef] [PubMed] [Google Scholar]
- Azithromycin for COVID-19: More than just an antimicrobial? Clin Drug Investig. 2020;40:683-6.
- [CrossRef] [PubMed] [Google Scholar]
- The potential impact of zinc supplementation on COVID-19 pathogenesis. Front Immunol. 2020;11:1712.
- [CrossRef] [PubMed] [Google Scholar]






