Translate this page into:
Fat graft myringoplasty: A clinical study and review of literature
*Corresponding author: Ritesh Mahajan, Department of Otorhinolaryngology, GMC, Kathua (J&K), India. ritesh54mahajan@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mahajan R, Mahajan N, Kour B. Fat graft myringoplasty: A clinical study and review of literature. Indian J Med Sci 2021;73:340-2.
Abstract
Objectives:
There are numerous surgical techniques that have been demonstrated and utilized to repair small perforations in the tympanic membrane (TM) with various graft materials such as veins, perichondrium, periosteum, and others. In our study, fat was taken as the graft material and the main aim of the study was to evaluate the success rate of graft uptake, assessment of hearing improvement, and complications of the operative procedure.
Material and Methods:
In this single-center study, 46 patients underwent fat myringoplasty, 52 ears were operated from October 2016 to September 2017 for a period of 1 year. A detailed history, general physical, and a through ear, nose, and throat examination were done. Audiometric assessment was done using pure tone audiometry. Patients between the age group of 15 and 50 years were included in the study.
Results:
A total of 46 patients were included in the study who met the inclusion criteria. Six patients had bilateral perforations and 40 patients had unilateral perforation, a total of 52 perforations were operated. Forty-three (82.69%) patients had successful graft uptake and graft failure was seen in 9 (17.30%) patients. Maximum gain in hearing was seen in in patients with hearing loss between 20 and 30 dB, that is, 24 patients (46.1%).
Conclusion:
Fat myringoplasty is a methodized, precise, inexpensive, mini-invasive, and cosmetic outpatient procedure for small perforations of TM. It can be done under local anesthesia and has a good success rate if the patient selection is done appropriately.
Keywords
Fat myringoplasty
Chronic suppurative otitis media
Tympanoplasty
Chronic suppurative otitis media
INTRODUCTION
Chronic suppurative otitis media (CSOM) is a common entity and frequently encountered in routine practice. Tympanic membrane (TM) perforations are most often associated with recurrent ear discharge and conductive hearing loss. Conditions such as trauma to ear, infections like acute and CSOM, post-grommet insertion perforation, residual perforation after ear surgery, and other idiopathic causes can lead to permanent TM perforation. Many of the times, most of the perforations heal by themselves. Surgical repair is indicated when a perforation becomes permanent and is associated with complications such as recurrent ear discharge, hearing loss, tinnitus, and various other complications. There are many any surgical techniques and various graft materials have been demonstrated and utilized over the years to repair the TM perforations. In a study by Ringenberg and Fornato in 1962, they reported primary closure of perforation of TM using fat graft in 86% of patients.[1] Every surgical procedures have its merits and demerits, but the main advantages of fat graft myringoplasty are that it is a minimally invasive, systematized, relatively safe, cost effective, time saving, and office-based/day care procedure which can be done under local anesthesia. The main aim of the study was to evaluate the success rate of graft uptake, assessment of hearing improvement, and complications of the operative procedure.
MATERIAL AND METHODS
A prospective clinical study was carried out in a tertiary care center from October 2016 to September 2017 for a period of 1 year. Our study used the clinical criteria published by Fiorino and Barbieri [Table 1], to include the patients for fat graft myringoplasty.[2] Those patients who did not fulfill these criteria were excluded from our study. A total of 46 patients were included in the study and 52 perforations were operated, patients were informed about the surgical procedure and informed written consent was taken following which a detailed history, general physical, and a through ear, nose, and throat examination were done. Patients between the age group of 15 and 50 years were included in the study. The evaluation of hearing was done preoperatively and in the 3rd post-operative month. The amount of closure of the air bone gap (ABG) at 500, 1 K, 2 K, and 4 K Hz was the parameter of hearing improvement. Acute infections such as upper respiratory tract infections, acute rhinosinusitis, and CSOM (active mucosal type) were treated appropriately before surgery.
| 1. Time elapsed from previous surgery longer than 6 months 2. Perforation of the pars tensa no larger than 5 mm 3. Non-marginal localization of perforation 4. Absence of calcific plaques adjacent to the perforation 5. Normal appearance of mucosa in tympanic cavity 6. Absence of any acute inflammation 7. Absence of middle ear discharge in the past 3 months 8. No evidence of cholesteatoma 9. mNo planned ossicular reconstruction 10. Absence of major Eustachian tube dysfunction |
Technique: All the procedures were performed under local anesthesia. Under all aseptic conditions, the patient was draped and local infiltration was given with 2% xylocaine with 1 in 100,000 adrenaline. The ear lobule was infiltrated in the posterior aspect and the ear canal skin was also infiltrated in four quadrants. The edges of the perforation were refreshed by sickle knife. A 1–1.5 cm incision was given in the posteroinferior portion of ear lobule with no. 15 blade, the fat was harvested and the incision was closed with 5–0 absorbable sutures. The fat was shaved and with the help of microcup forceps, it was kept on the TM perforation and was gently negotiated in an hour glass formation using a straight pick. Caution was taken as oversized fat plug can further traumatize the perforation margins leading to atrophy or necrosis later on and undersized fat plug should be avoided to prevent dehiscence in grafting.[3] After proper adjustment of fat graft, small pieces of gelfoam were placed around the graft to support it and the ear canal was filled with gelfoam soaked with antibiotic drops and an antibiotic ointment coated wick was placed in outer external ear canal. Ear dressing was done and the patient was discharged with appropriate medicines. Follow-up was done in the 1st, 3rd, and 6th post-operative months. Failure cases were counted when the relapsing perforation occurs and persists until the end of the 3rd month postoperatively. Descriptive and inferential statistical analysis has been carried out in the present study, and Microsoft Word and Excel have been used to generate graphs and tables.
RESULTS
A total of 46 patients were included in the study who met the inclusion criteria. Six patients had bilateral perforations and 40 patients had unilateral perforation, a total of 52 perforations were operated. Out of 46 patients, 22 were female and 24 were male patients. Patients in the age group of 15–50 were included in the study, maximum number of patients was in the age group between 30 and 40 years. The causes for the TM perforations were CSOM (24), trauma (14), post-grommet extraction (5), post-myringoplasty residual perforation (6), and idiopathic (3). There were no major complications encountered during surgery. In our study, a total of 52 ears were operated out of which 43 (82.69%) patients had successful graft uptake and graft failure was seen in 9 (17.30%) patients. In the failure cases, 4 patients (44.4%) had postoperative infection, 3 patients (33.3%) had graft medialized and necrosis, and 2 patients (22.2%) had residual perforation after surgery. The pre- and post-operative ABG is detailed statistically in Table 2. Evaluation of hearing assessment was done with pure tone audiometry, pre-operative and post-operative ABG was calculated from difference of air conduction thresholds and bone conduction thresholds for all four frequencies 500, 1 K, 2 K, and 4 K Hz. Maximum gain in hearing was seen in in patients with hearing loss between 20 and 30 dB, that is, 24 patients (46.1%).
| Air bone gap calculated from average air conduction and bone conduction thresholds at frequencies 500, 1 K, 2 K, and 4 K Hz (dB) | Pre-operative number of patients (%) | Post-operative number of patients (%) |
|---|---|---|
| <10 | 8 (15.3) | 14 (26.9) |
| 10–20 | 18 (34.6) | 28 (53.8) |
| 20–30 | 24 (46.1) | 10 (19.2) |
| 30–40 | 2 (3.8) | - |
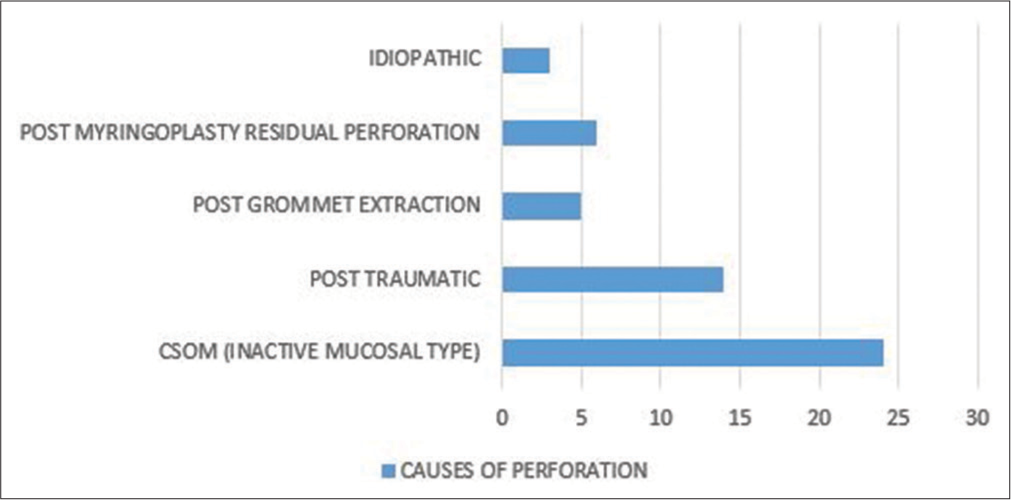
- Causes of perforation
DISCUSSION
The main aim of the fat graft myringoplasty was to repair perforations in pars tensa of TM which is less than 5 mm. This procedure causes minimal pain and there is no trauma to the healthy ear drum due the absence of skin incisions, dissections of meatal flaps and is associated with fewer complications with maximum improvement of the air/bone gap after the surgery.[4] Fat plug myringoplasty was first introduced by Ringenberg and the success rate was reported as 87% for small perforations.[5] In the following studies, the success rate was ranging from 80% to 92% in cases of small perforations including primary procedures.[6,7] In our study, the success rates were 82.69% which are at par with other studies. Afterward, Deddens et al. found the TM perforation size to be an important factor in predicting the success rate of myringoplasty.[6] In our study, we have followed criteria published by Fiorino and Barbieri, in which the size of the perforation is less than 5 mm. According to Kaddour, the size of the perforation should not exceed 30% of the size of the eardrum.[7] Terry et al., who performed fat myringoplasty to correct perforations of various sizes, cited a closure rate of 79.4% if the perforation accounted for <50% of TM and 57.1% if the perforation was larger than that size.[8] The failure rate in our study was 9 out of 52 ears (17.3%) and it was due to intraoperative or post-operative infection, graft size, middle ear infections, and idiopathic causes. Fiorino et al. attributed the failure causes to: Anterior perforations, inadequate graft support, poor vascular supply, or infection; and delayed failures due to TM atrophy, infections, or Eustachian tube dysfunction with the change of TM structure.[2] Hearing assessment was done pre and postoperatively which showed a significant improvement. Post-operative hearing assessment was done in the 3rd month which showed majority of the patients who were operated had <20 dB loss (80.7%). The previous studies showed Saliba et al., recorded 17 dB as a mean improvement of air/bone gap in his study.[4] Liew et al. recorded improvement in 11 of their 15 patients.[9] Hagemann and Housler et al. showed hearing improvement in 21 of their 44 patients in their study.[10] Limitations of our study were a small sample size and relatively less follow-up period when compared with other similar conducted studies, rest of the results of our study including success rate was at par with other studies.
CONCLUSION
Fat myringoplasty is a methodized, precise, inexpensive, mini-invasive, and cosmetic outpatient procedure for small perforations of TM. It can be done under local anesthesia and has a good success rate if the patient selection is done appropriately. Operative time is less and the patient can continue routine activity after surgery. Our study concludes that fat graft myringoplasty is a guarded procedure and can be used as an alternative to temporalis fascia graft myringoplasty in smaller TM perforations.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- The fat graft in middle ear surgery. Arch Otolaryngol. 1962;76:407-13.
- [CrossRef] [PubMed] [Google Scholar]
- Fat graft myringoplasty after unsuccessful tympanic membrane repair. Eur Arch Otolaryngol. 2007;264:1125-8.
- [CrossRef] [PubMed] [Google Scholar]
- Fat myringoplasty-a prospective clinical study. Egypt J Ear Nose Throat Allied Sci. 2013;14:91-5.
- [CrossRef] [Google Scholar]
- Hyaluronic acid fat graft myringoplasty: How we do it. Clin Otolaryngol. 2009;33:610-4.
- [CrossRef] [PubMed] [Google Scholar]
- Adipose myringoplasty in children. Laryngoscope. 1993;103:216-9.
- [CrossRef] [PubMed] [Google Scholar]
- Myringoplasty under local anaesthesia: Day case surgery. Clin Otolaryngol Allied Sci. 1992;17:567-8.
- [CrossRef] [PubMed] [Google Scholar]
- Fat graft myringoplasty-a prospective trial. Clin Otolaryngol Allied Sci. 1988;13:227-9.
- [CrossRef] [PubMed] [Google Scholar]
- Synchronous fat plug myringoplasty and tympanostomy tube removal in the management of refractory otorrhoea in younger patients. Int J Pediatr Otorhinolaryngol. 2002;66:291-6.
- [CrossRef] [Google Scholar]
- Tympanoplasty with adipose tissue. Laryngorhinootologie. 2003;82:393-6.
- [CrossRef] [PubMed] [Google Scholar]






