Translate this page into:
Flaky paint dermatosis in two adult patients of malnutrition
*Corresponding author: M. Ramam, Department of Dermatology, All India Institute of Medical Sciences, New Delhi, India. mramam@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Swarnkar B, Bhari N, Ramam M. Flaky paint dermatosis in two adult patients of malnutrition. Indian J Med Sci. doi: 10.25259/IJMS_251_2023
Abstract
Protein-energy malnutrition (PEM) is a state of undernutrition with various cutaneous manifestations. It is widely studied in children but is common yet neglected in adults. We report two adult cases of flaky paint dermatosis due to PEM, along with a description of their dermoscopy features. This paper intends to create awareness about these cutaneous changes amongst physicians and our fellow dermatologists for early recognition of PEM in adults.
Keywords
Protein-energy malnutrition
Flaky paint dermatosis
Dermoscopy
Adult
INTRODUCTION
Kwashiorkor is a form of protein-energy malnutrition (PEM) where a protein deficit is noted in spite of adequate caloric intake. Cutaneous manifestations of Kwashiorkor include xerosis, atrophy, desquamation, and dilution of pigment in skin and hair. Although quite extensively documented in children, it is often a neglected entity in adults. We report two adult cases of malnutrition presenting with peeling paint/flaking paint dermatosis.
CASE REPORTS
Case 1
A man in his 30s was admitted to the gastroenterology department for the evaluation of an increase in the passing of undigested food during defecation and recurrent episodes of diarrhea with the differential diagnoses of ulcerostricturing disease of small intestine with protein-losing enteropathy, Crohn’s disease, and Bechet’s disease. He has been a known case of celiac disease for the past 12 years. He had lost approximately 45 kg weight in the past 1 year and had frequent hospital admissions for anasarca and anemia. A dermatology opinion was requested for asymptomatic to mildly pruritic, hyperpigmented lesions over the trunk and bilateral buttocks for the past 3–4 days. The patient gave a history of a similar rash in the past, which resolved spontaneously in 1–2 weeks. On examination, there were irregular, reticular, and hyperpigmented scales over the back and bilateral buttocks [Figure 1]. The removal of the scale revealed a moist erythematous base. He had a low body mass index, anemia, hypoalbuminemia, hypocalcemia, low serum transferrin, iron, total iron binding capacity, and a deranged thyroid profile [Table 1].
| BMI and investigations (normal range) |
Case 1 | Case 2 |
|---|---|---|
| BMI (18.5–24.9) | 11.7 | 18.9 |
| Hemoglobin (12–15 g/dL) | 7.0 | 9.0 |
| Serum total protein (6.4–8.3 g/dL) | 4.0 | 4.6 |
| Serum total albumin (3.4–5.4 g/dL) | 1.5 | 1.0 |
| Serum calcium (8.6–10 mg/dL) | 7.1 | 5.8 |
| Serum phosphate (2.5–4.5 mg/dL) | 2.2 | 5.4 |
| Serum transferrin (200–360 mg/dL) | 103 | 30 |
| Serum iron (59–158 ug/dL) | 14 | 49 |
| Serum ferritin (30–400 ng/mL) | 26.1 | 1843 |
| Serum total iron binding capacity (250–450 ug/dL) | 152 | 57 |
| Serum TSH (0.27–4.2 uIU/ml/T3 (80–200 ng/dL)/T4 (5.1–14.1 ug/dL) | 6.6/109/4.0 | 4.67/59/2.3 |
| C-reactive protein (<0.5 mg/dL) | – | 6.7 |
BMI: Body mass index, TSH: Thyroid-stimulating hormone

- Irregular, reticular, and hyperpigmented scales on the back.
Case 2
A man in his 30s who lived alone was brought to the hospital by neighbors when they found him lying unconscious outside his house. He was admitted to the medical intensive care unit and diagnosed as a case of disseminated Koch’s with sepsis with disseminated intravascular coagulation. A dermatology consultation was requested for the hyperpigmented skin lesions over the body. On examination, there was generalized xerosis. There were irregular, hyperpigmented scales, with the majority of them showing a moist, erythematous base over the trunk and bilateral upper and lower limbs [Figure 2a and b]. He had anemia, hypoalbuminemia, hypocalcemia, low serum transferrin, iron, total iron binding capacity, deranged thyroid profile, and elevated C-reactive protein [Table 1]. Serum zinc level could not be tested due to non-availability.
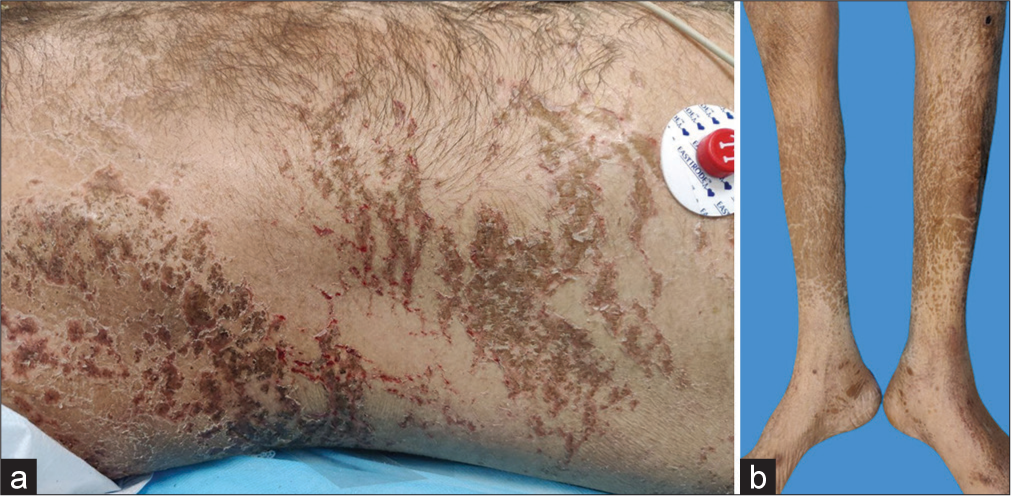
- (a) Irregular, hyperpigmented scales on the trunk, with many showing a moist, erythematous base, and (b) irregular, hyperpigmented scales over bilateral lower limbs.
There was no evidence of angular cheilitis, glossitis, flag hair sign, thin, soft nails, or flag nail sign in either case. Dermoscopy in both cases showed irregular areas of hyperpigmentation with a surrounding halo of light brown pigmentation. There were areas of superficial whitish scales over the skin [Figure 3]. The first patient denied skin biopsy, while the second patient had an early demise, so a biopsy could not be done.
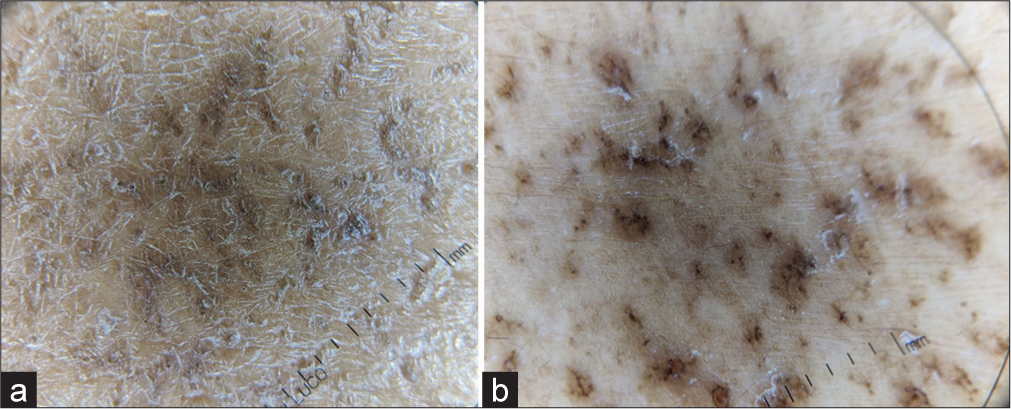
- Irregular areas of hyperpigmentation with a surrounding halo of light brown pigmentation. There were areas of superficial whitish scales over the skin (Using hand-held polarized dermatoscope IDS1100, ILLUCO, KOREA). (a) Non-polarized mode (scales are more prominent) and (b) polarized mode (pigmentary changes are more prominent).
Based on history, examination, and investigations, we considered the diagnosis of nutritional dermatosis in both patients. Asteatotic eczema, zinc deficiency, and pellagra were considered in the differential diagnoses. Absence of significant itching, lack of winter aggravation, aggravation post increased episodes of diarrhea (in case 1), and the clinical picture was more in favor of nutritional dermatosis. Asteatotic eczema usually presents with dry skin with superficial fissuring rather than thick scales with underlying erosions/hypopigmentation as was seen in our cases. Zinc deficiency usually presents with the predominant periorificial and acral distribution of eczematous or psoriasiform plaques. Flexures may also get involved. In pellagra, acute sunburn-like lesions or scaly plaques are preferentially photo-distributed. These features were lacking in our patients; however, malnutrition patients also have associated micronutrients and vitamin deficiency in the majority of the cases.
Both of them were started on appropriate calorie-protein diets with slow increases in the calorie and protein intake, starting with small frequent meals and daily calorie intake of 2000–3000, and protein intake of 2 g/kg body weight, iron and calcium supplements, and multivitamins including zinc along with the management of the underlying illnesses and were also advised liberal emollient application over the body. The lesions resolved within 2 weeks in the first patient [Figure 4], while the second patient succumbed to his illness on the second day of admission.

- Resolution of lesions over the back in the first patient.
DISCUSSION
Based on National Family Health Survey-4 (2015–2016), approximately 20% of adult males and 23% of adult females were underweight.[1] Undernutrition occurs due to decreased intake of nutrients, increased demand than supply, or increased loss from the body. Various predisposing factors in adults include malabsorption disorders,[2] infections,[3] chronic illnesses like malignancy,[4] and psychiatric illness.[5]
The cutaneous clinical manifestations of PEM include “peeling paint/flaky paint dermatosis,” as was seen in our patients, ichthyosiform dermatosis, exfoliative erythroderma, hypopigmentation, hyperpigmentation, fissures, erosions, hyperkeratotic plaques, petechiae, mucosal, nail, and hair changes.[6] Various mechanisms that have been hypothesized to cause these cutaneous changes include the decreased activity of sebaceous glands, deficiency of protein essential fatty acids, free radical damage to the skin, and dysmaturation of keratinocytes.[7] Dermoscopy showed scaling, accentuated pigmentary network, and perifollicular hypopigmentation in a case report.[3] The histopathological evaluation shows a pale epidermis, hyperkeratosis, and parakeratosis with foci of vacuolation in the granular cell layer.
Laboratory evaluation may reveal anemia, low serum protein and albumin, deranged blood sugar, and electrolytes. Treatment includes fluid resuscitation, correction of electrolyte imbalance and hypoglycemia, nutritional replacement with a slow increase in calorie intake to around 3000 kcal/day, and liberal moisturization of the skin. Oral nutritional supplements can be added which provide both macro- and micronutrients in the form of ready-to-eat semi-solid/solid/liquid food. They can be added to meals or taken separately for food fortification and according to experts, they should provide around 400 kcal energy and 30 g of protein per day. The parenteral mode of nutrition is reserved for people who are not able to meet their nutritional requirements by enteral means. A low-protein diet is preferred over a high-protein diet (16.4% of total energy) due to a lower mortality rate and accelerated loss of edema in kwashiorkor cases. A low-protein diet also delivers low energy in the initial phase of treatment, decreasing the risk of refeeding syndrome. Refeeding syndrome is a potentially fatal shift in electrolytes and fluid that may be seen in malnourished individuals after artificial refeeding. These occur due to metabolic and hormonal (high insulin) changes causing complications such as hypokalemia, hypophosphatemia, abnormal sodium, and fluid balance. To prevent this, baseline electrolytes should be checked, any abnormalities should be treated, and low-calorie diet (0.0418 MJ/kg/day) should be initiated, and calorie intake should be increased slowly over 4–7 days.[8,9]
Dermatosis is associated with poor prognosis and is a strong predictor of death.[10]
CONCLUSION
Dermatologists and physicians need to be aware of the cutaneous manifestations of PEM for early evaluation and management of such patients. The delay in the diagnosis might have catastrophic repercussions, including death.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- The double burden of malnutrition in India: Trends and inequalities (2006-2016) PLOS One. 2021;16:e0247856.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous manifestations of kwashiorkor: A case report of an adult man after abdominal surgery. An Bras Dermatol. 2011;86:1174-7.
- [CrossRef] [PubMed] [Google Scholar]
- Kwashiorkor-like condition: Dermoscopic illustration in an adult with chronic kidney disease. J Pak Assoc Dermatol. 2021;31:138-9.
- [Google Scholar]
- Peeling paint dermatosis in a leukemia patient. JAAD Case Rep. 2020;6:354-6.
- [CrossRef] [PubMed] [Google Scholar]
- Kwashiorkor and an acrodermatitis enteropathica-like eruption after a distal gastric bypass surgical procedure. Endocr Pract. 2007;13:277-82.
- [CrossRef] [PubMed] [Google Scholar]
- Nutritional dermatoses in the hospitalized patient. Cutis. 2020;105:296, 302-8;E1;E2;E3; E4;E5
- [Google Scholar]
- New views on the pathogenesis of Kwashiorkor: Methionine and other amino acids. J Pediatr Gastroenterol Nutr. 1995;21:130-6.
- [CrossRef] [PubMed] [Google Scholar]
- Management of malnutrition in older patients-current approaches, evidence, and open questions. J Clin Med. 2019;8:974.
- [CrossRef] [PubMed] [Google Scholar]
- Refeeding syndrome: What it is, and how to prevent and treat it. BMJ. 2008;336:1495-8.
- [CrossRef] [PubMed] [Google Scholar]
- Dermatosis in children with oedematous malnutrition (Kwashiorkor): A review of the literature. J Eur Acad Dermatol Venereol. 2014;28:995-1001.
- [CrossRef] [PubMed] [Google Scholar]






