Translate this page into:
Four-phase safety checklist for health care providers in COVID-19 hospitals: A practical tool for survival!

*Corresponding author: Dheeraj Kapoor, Department of Anaesthesia and Intensive Care, Government Medical College and Hospital, D Block, 5th Floor, Sector 32, Chandigarh, Chandigarh, India. kapoor.dheeraj72@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kapoor D, Singh M, Sharma M, Kumar V. Four-phase safety checklist for health care providers in COVID-19 hospitals: A practical tool for survival! Indian J Med Sci 2020;72(3):170-2.
Abstract
Pandemic of coronavirus disease 2019 (COVID-19) has generated immense viral exposure risk among frontline health care providers (HCPs), especially due to aerosol-generating events and procedures. This further increased the risk of serious mental health disorders amongst them. Hitherto, there is lack of any specific safety protocol specially during the pre- and post-exposure period for HCPs, who provide direct clinical care to patients suffering from COVID-19. We propose a four-phase checklist approach, which may help them in mental preparedness as well as organizing themselves prior and following virus exposure in clinical postings and may enhance the safety standards. The checklist comprises simple steps and may work as a documented track record of precautionary and preventive measures which must be followed by HCWs working in dedicated COVID-19 hospitals.
Keywords
COVID-19
SARS-CoV-2
Health care providers
Checklist
Aerosol generating events
INTRODUCTION
Recent pandemic of “severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), commonly called COVID-19, imposes a huge risk among health care providers (HCPs) of getting exposed to viral infection and further transmission to their close contacts and family members.[1] It certainly generates a significant level of mental health issues which include overwhelming situations, complete disruption of social life, feeling of vulnerability, constantly being at risk of getting infected, and fear of transmitting the disease to families and loved ones.[2]
Most of the frontline HCPs all over the world at present are facing enormous pressure, including a risk of infection and inadequate protection from contamination, overwork, frustration, discrimination, isolation, negative emotions, a lack of contact with their families, and over exhaustion.[3] These unprecedented circumstances have significantly increased the risk of mental health disorders such as post-traumatic stress disorder (PTSD) or depression, anxiety-related disorders, substance abuse, and suicidal tendencies.[3]
Recent studies observed that frontline health care workers possess more than ten-fold higher risk of testing positive with SARS-CoV-2 when compared with the general population.[4] Further, the risk increases further by nearly 25% due to inadequate access to personal protective equipment (PPE) and other protective gear.[4] According to initial estimates in developed countries, HCPs may account for nearly 10% of all diagnosed cases which might be further high in developing nations due to limited resources.[5] The spread of infection is predominantly common in HCPs who are exposed to aerosol-generating events, where certain incidents and procedures are believed to generate aerosols and droplets as a source of respiratory pathogens.[6]
There are many guidelines published to prevent transmission through aerosol-generating events and procedures.[6-8] However, till now, there is a lack of literature on systematic approach for frontline HCPs working in hospital settings, particularly where direct clinical care is provided to patients suffering from COVID-19. Keeping in line with the aforementioned issues, we propose a four-phase checklist approach which may help them in mental preparedness as well as organizing themselves prior and following their virus exposure in clinical postings and may enhance the safety standards. The proposed checklist is simple steps to follow by HCPs by reducing the ambiguity about the actions required in the aforementioned hospital settings. The four-phase approach comprises “Pre-hospital Pre-Donning,” “In-Hospital Pre-Donning,” “In-Hospital Post-Doffing,” and “Out-of-Hospital Post-Doffing” phase, respectively. The “Pre-hospital Pre-donning” phase is particularly highlighted and focused on the mental preparedness of HCPs before the start of high-pressure duties in COVID-19 wards and critical care settings. It includes an organized checklist of actions and conducts essential for relieving mental stress. Special attention is paid to isolation rooms for HCPs working in COVID-19 setups during their off-hours. These simple isolation rooms can be made in hostels or home place to ensure minimum contact with other hostel mates or family members. Basic facilities such as access to separate washrooms, provisions of sanitizers, and separate entry and exit passage for HCPs remain a primary requisite during their off-hours. This will certainly minimize the exposure to other people living with them and provides a sense of relief and assurance for the HCPs. The checklist also includes actions such as provisions for high-quality sleep, balanced nutrition, protective care of clothes and other accessories, and care taken during commuting to hospital. The “In-Hospital Pre-Donning” and “Post-Doffing” phase includes some basic actions taken in addition to the universal precautions recommended while wearing protective gear and PPE. The “Pre-Donning” phase includes special emphasis targeted on the size, integrity, and labeling of PPE along with care and storage of clothes and other accessories before wearing-dedicated scrubs. The focal point of the “In-Hospital Post-Doffing” phase includes the provision of sanitizing facilities coupled with fresh scrubs and face masks in the hospital. In the “Out-of-Hospital Post-Doffing” phase, weightage is given to suitable disposal of the cap, mask, and clothes, washing, and bathing facilities together with provisions of fresh clothing’s and mask.
CONCLUSION
The proposed checklist may work as a documented track record of precautionary and preventive measures which must be followed by HCPs working in dedicated COVID-19 hospitals [Figure 1]. Each item is checked off as it is completed, verified, identified, and answered by placing a mark in a designated space. This will draw a sense of responsibility and provides intense amounts of mental satisfaction and assurance in their over-all conduct. The checklist highlights the essential criteria that must be considered in a particular area and it also helps the user to remember important criteria, achieves standardization of a process, and enhances an assessment’s objectivity and reproducibility with significantly increased efficiency.[9]
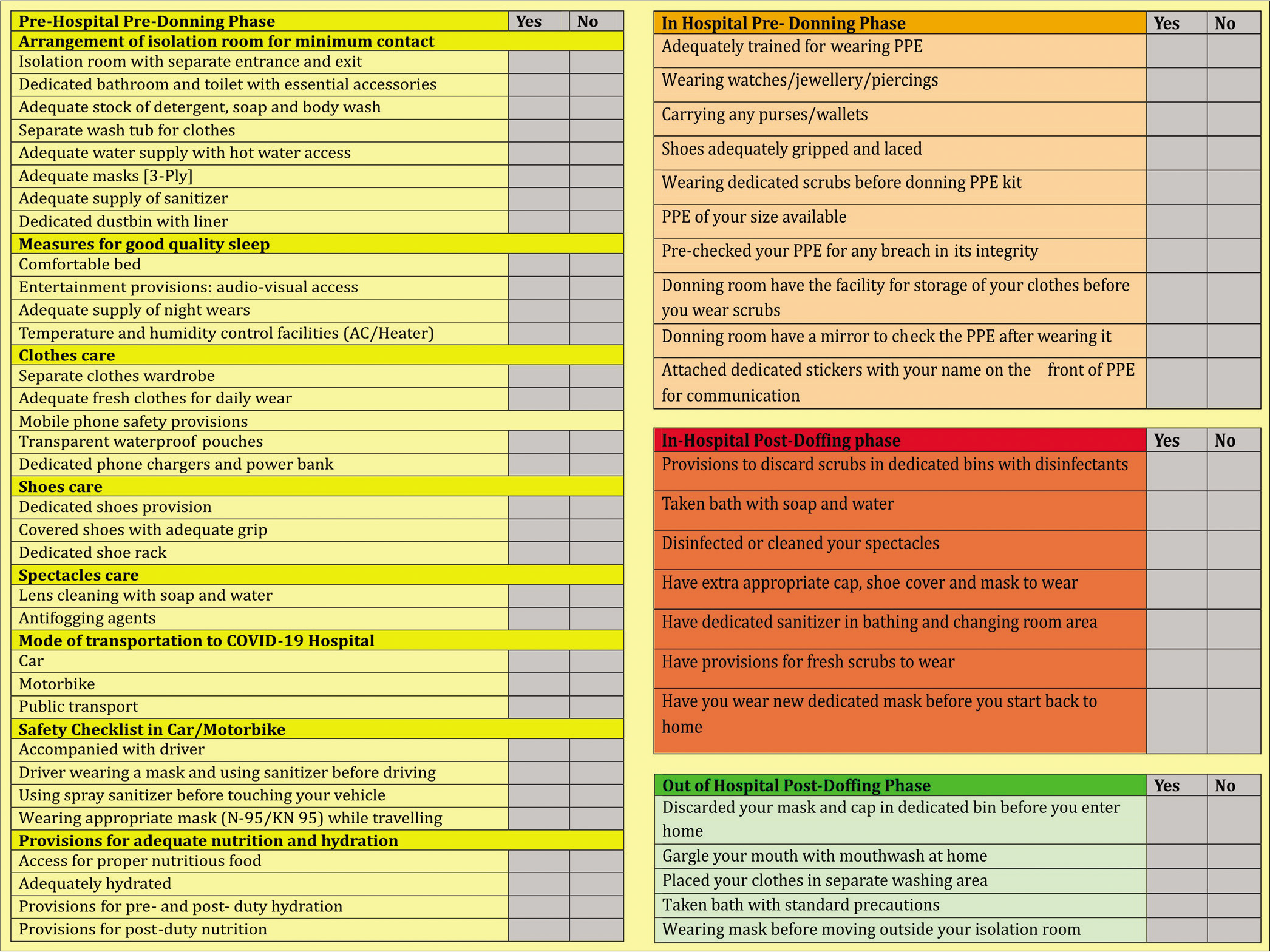
- Four-phase safety checklist for health care providers in COVID-19 hospitals.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Nil.
References
- The psychological impact of COVID-19 pandemic on health care workers in a MERS-CoV endemic country. J Infect Public Health. 2020;136:877-82.
- [CrossRef] [PubMed] [Google Scholar]
- Occupational risks for COVID-19 infection. Occup Med (Lond). 2020;70:3-5.
- [CrossRef] [PubMed] [Google Scholar]
- The mental health of medical workers in Wuhan, China dealing with the 2019 novel Coronavirus. Lancet Psychiatry. 2020;73:e14.
- [CrossRef] [Google Scholar]
- Risk of COVID-19 among frontline healthcare workers and the general community: A prospective cohort study. Lancet Public Health. 2020;5:e475-83.
- [CrossRef] [Google Scholar]
- COVID-19: The case for health-care worker screening to prevent hospital transmission. Lancet. 2020;395:1418-20.
- [CrossRef] [Google Scholar]
- All India difficult airway association (AIDAA) consensus guidelines for airway management in the operating room during the COVID-19 pandemic. Indian J Anaesth. 2020;64:S107-15.
- [CrossRef] [PubMed] [Google Scholar]
- Consensus guidelines for managing the airway in patients with COVID-19. Anaesthesia. 2020;75:785-99.
- [CrossRef] [PubMed] [Google Scholar]
- Surviving sepsis campaign: Guidelines on the management of critically Ill adults with Coronavirus disease 2019 (COVID-19) Crit Care Med. 2020;48:e440-69.
- [CrossRef] [PubMed] [Google Scholar]
- Development of medical checklists for improved quality of patient care. Int J Qual Health Care. 2008;20:22-30.
- [CrossRef] [PubMed] [Google Scholar]






