Translate this page into:
Microvascular and macrovascular complications in non-obese/overweight and obese/overweight type 2 diabetes mellitus
*Corresponding authors: Digvijay Chavan, Department of General Medicine, Government Medical College, Aurangabad, Maharashtra, India. drdigvijaymd@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Chavan D, Lomte N, Bhattacharya M, Singh A, Sonavale R. Microvascular and macrovascular complications in non-obese/overweight and obese/overweight type 2 diabetes mellitus. Indian J Med Sci 2023;75:156-60.
Abstract
Introduction:
Obesity is defined for the Asian population as a body mass index (BMI) >25 kg/m2, while overweight is a BMI between 23 kg/m2 and 24.9 kg/m2. Both obesity and type 2 diabetes are major independent risk factors for cardiovascular disease according to previous literature. The data on the risk of obesity on diabetic complications are scarce, which is why this study was conducted. This study is designed to study the hypothesis that complications of diabetes are more in obese/overweight than in non-obese patients.
Materials and Methods:
We conducted an observational cross-sectional study in a tertiary care center. Patients with known type 2 diabetes mellitus admitted to our center were serially selected and BMI was calculated and patients were divided into non-obese/overweight and obese/overweight categories according to the World Health Organization recommendations for the Asian population. Patients were assessed for diabetes control and duration of diabetes. Each patient was also evaluated for microvascular and macrovascular complications of diabetes according to the American diabetes association guidelines. Complications in obese/overweight diabetics and diabetics with normal BMI were compared. SPSS version 23 software was used for statistical analysis.
Results:
A total of 84 admitted diabetics were included, of the 84 patients 45 (53.57%) were women, and 56 (66.67%) were overweight and obese. About 10.71% of diabetics with normal BMI and 26.79% of overweight/obese diabetics had retinopathy. 8 (28.57%) patients in the normal BMI group, while 26 (46.42%) patients in the overweight/obese group had ischemic heart disease (IHD) (P < 0.05).
Conclusion:
Obesity and overweight are associated with a high risk of complications of diabetes, especially retinopathy and IHD. Glycemic control is also poor among obese/overweight diabetics. Microvascular complications occur earlier in obese/overweight diabetics.
Keywords
Diabetes mellitus type 2
Obesity
Microvascular complications
Macrovascular complications
INTRODUCTION
Obesity is often defined simply as a condition of abnormal or excessive fat accumulation in adipose tissue, to the extent that health may be impaired.[1] It is proven that obesity increases the risk of certain diseases and other related health problems. Obesity is a serious worldwide health epidemic and about 30–65% of Indian adult urban population is obese or overweight.[2] Obesity and type 2 diabetes mellitus (DM) are closely linked. Both obesity and type 2 DM are major causes of morbidity and also mortality from atherogenic macrovascular and microvascular diseases, and both are independent risk factors for cardiovascular disease according to previous literature. The majority but not all patients with DM type 2 are overweight or obese.[3]
Body mass index (BMI) provides the most useful measure of obesity.[4] High BMI is also found to be associated with increased endothelial dysfunction, which is a major factor in atheroma plaque formation and the development of thrombosis.
The risk of obesity on diabetes microvascular complications is not well known and data on the same are scarce; hence, this study has been conducted. The present study is designed to study the hypothesis that complications of diabetes are more in obese than non-obese patients. More data on this public health issue would provide evidence-based knowledge to develop guidelines and policies on this common health issue. The primary objective of this study was to study the prevalence of microvascular and macrovascular complications in obese/overweight and non-obese/overweight type 2 DM, whereas secondary objectives were to study the relation of duration of type 2 DM with microvascular and macrovascular complications and to study the glycemic status in obese/overweight and non-obese/overweight type 2 DM patients.
MATERIALS AND METHODS
This is an observational cross-sectional study of 84 known type 2 DM admitted patients, which was carried out in the Department of General Medicine at a tertiary care center after getting approval from an Institutional Ethics Committee. Diagnosed patients (age >20 years) of diabetes as per the American diabetes association (ADA) guidelines[3] were included in this study. Patients who were not willing to give consent and patients with age below 20 years of age were excluded from the study.
After obtaining written informed consent, patients were included in the study. Data were collected by preformed pro forma.
The body weight and height of each patient were measured, and BMI was calculated.
Height was measured using a standard stadiometer in centimeters in a standing position with back straight, arms at the side, and feet close to each other, and weight was measured using a standard analog weighing machine in kilograms in a standing position.
BMI is defined as the weight of a person in kilograms divided by the square of the height of a person in meters (kg/m2). For adults over 20 years old from Asian populations, BMI falls into one of the categories as showed in [Table 1].
| BMI | Nutritional status |
|---|---|
| 18.0–22.9 kg/m2 | Normal |
| 23.0–24.9 kg/m2 | Overweight |
| >25 kg/m2 | Obese |
BMI: Body mass index
Each patient was evaluated for the status of glycemic control. Controlled diabetes was defined according to ADA guidelines if fasting glucose is 80–130 mg/dL; postprandial glucose is <180; and HbA1C <7.0.[3]
Along with glycemic control, all patients were also evaluated for microvascular and macrovascular complications of type 2 DM as per ADA guidelines.[3] Collected data were analyzed using the criteria for overweight, obesity, diabetes, and its complications. Microvascular and macrovascular complications in nonobese/overweight and obese/overweight type 2 diabetics were compared with appropriate statistical tests.
Microvascular complications
Eye diseases: Retinopathy and macular edema were assessed by ophthalmologists at our tertiary care center.
Neuropathy: Sensory, motor, and autonomic neuropathy;
Assessment for distal symmetric sensory polyneuropathy was done by a careful history and simple clinical tests as follows:
Small-fiber function assessment by pinprick and temperature sensation
Large-fiber function assessment by vibration perception and 10-g monofilament
Protective sensation assessment by 10-g monofilament.[3]
(Monofilament test was considered positive when patients were not able to sense four out of ten stimulations over the bilateral soles.)
Diabetic autonomic neuropathy was diagnosed if a patient had hypoglycemia unawareness, resting tachycardia, orthostatic hypotension, gastroparesis, constipation, diarrhea, fecal incontinence, erectile dysfunction, neurogenic bladder, and sudomotor dysfunction with either increased or decreased sweating.[3]
c. Nephropathy: Diabetic kidney disease diagnosis was made based on the presence of albuminuria and/or reduced estimated glomerular filtration rate (eGFR) without signs or symptoms of other primary causes of kidney damage.[3] eGFR was calculated from the CKD-EPI creatinine equation (2021) equation with the help mobile application based on plasma creatinine, age, race, and gender.[6]
Blood sugar levels and serum creatinine were assessed by fully automatic and semi-autoanalyzer ERBA TransAsia machines with respective kits based on the principle of spectrophotometric methods available at the biochemistry department of the study center.
Macrovascular complications
Coronary heart disease was assessed by detailed history, clinical examination, and changes on electrocardiogram
Cerebrovascular disease was assessed by detailed history, clinical examination, and non-contrast computed tomography brain whenever indicated.
Data was collected with the help of preformed proforma, was entered in SPSS software version 23, and was analyzed with appropriate statistical tests.
RESULTS
Among 84 diabetic patients studied, 39 were male and 45 were female. Out of 39 male patients, the maximum number of patients (53.85%) were from the age group of 40–60 years and 33.33% had age more than 60 years, whereas only 12.82% were from the age group <40 years. Moreover, out of 45 female patients’, the maximum number of patients belonged to the age group of more than 60 years, whereas 35.6% and 11% of total female diabetics were from the age group of 40–60 years and <40 years, respectively [Figure 1].
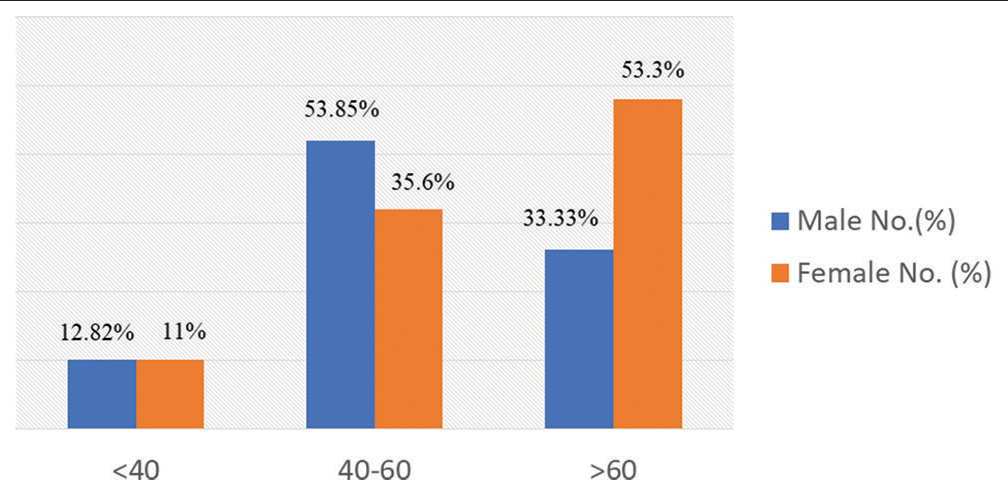
- Sex and age-wise distribution of the study population.
About 41.66% of normal BMI patients and 58.34% of overweight and obese patients had uncontrolled diabetes, this difference was found to be statistically significant (P = 0.01) [Figure 2].
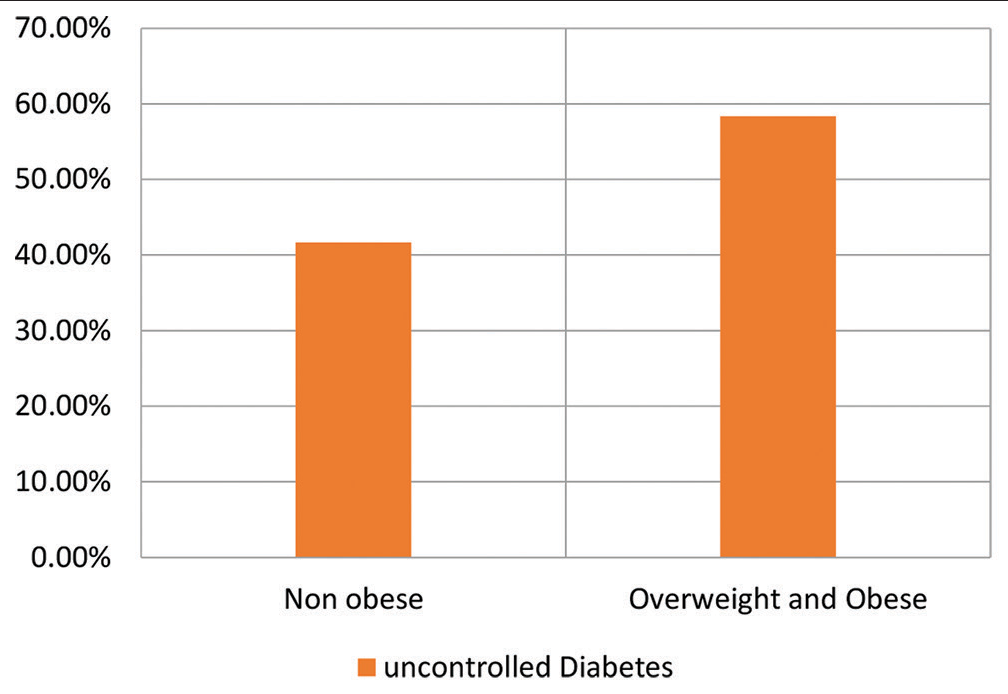
- The proportion of non-obese and overweight/obese patients having uncontrolled diabetes.
Among the total of 84 randomly selected type 2 diabetic patients of the study population, 33.33% had a normal BMI while 66.67% of the patients were obese and overweight. The mean age of non-obese/overweight patients was 54.64 years while the mean age of obese/overweight patients was 57.23 years which is comparable in both groups. About 53.57% of normal BMI patients and 42.86% of overweight and obese patients were male while 46.43% of normal BMI patients and 57.14% of overweight and obese patients were female. About 10.71% of normal BMI patients and 26.79% of overweight and obese patients had diabetic retinopathy this difference was found to be statistically significant (P = 0.05). The mean creatinine of the group of normal BMI patients was 1.4 and of the group of overweight and obese patients was 2.12 (P = 0.001). The mean eGFR was found to be >60 (69.57) in normal BMI diabetic patients and <60 (57.91) in overweight and obese patients. About 35.71%, 53.27%, 14.28%, and 28.57% of normal BMI patients while 46.43%, 51.79%, 12.5%, and 46.42% of overweight and obese patients had diabetic nephropathy, neuropathy, heart disease, and cerebrovascular disease respectively. The mean duration of diabetes before the development of macrovascular complications was found to be 5.56 years in the group of normal BMI patients compared to 5.74 years in overweight and obese patients. On the other hand, the duration of diabetes before the development of microvascular complications in the normal-weight patient group (8.56 years) was found to be statistically significantly longer than the overweight and obese group (6.48 years), (P = 0.05) [Table 2].
| Category | Non-obese/overweight (%) | Overweight/obese (%) | Total | P-value |
|---|---|---|---|---|
| Total (%) | 28 (33.33) | 56 (66.67) | 84 | 0.03 |
| Mean age (years) | 54.64 | 57.23 | NA | 0.2 |
| Males | 15 (53.57) | 24 (42.86) | 39 | 0.06 |
| Females | 13 (46.43) | 32 (57.14) | 45 | 0.07 |
| Retinopathy | 3 (10.71) | 15 (26.79) | 18 | 0.05 |
| Mean creatinine | 1.4 | 2.12 | NA | 0.001 |
| Mean estimated glomerular filtration rate | 69.57 | 57.91 | NA | NA |
| Nephropathy | 10 (35.71) | 26 (46.43) | 36 | 0.4 |
| Neuropathy | 15 (53.27) | 29 (51.79) | 44 | 0.8 |
| Cerebrovascular accident | 4 (14.28) | 7 (12.5) | 11 | 0.7 |
| Ischemic heart disease | 8 (28.57) | 26 (46.42) | 34 | 0.05 |
| Average duration of diabetes mellitus (years) | ||||
| Macrovascular complications | 5.56 | 5.74 | NA | 0.2 |
| Microvascular complications | 8.56 | 6.48 | NA | 0.05 |
Diabetes was poorly controlled in 65% of non-obese/overweight patients compared with 72% of obese/overweight patients with microvascular complications. Diabetes was poorly controlled in 60% of non-obese/overweight patients compared with 74% of obese/overweight patients with macrovascular complications [Table 3].
| Poor glycemic control in diabetic patients with complications | Non-obese/overweight | Obese/overweight |
|---|---|---|
| Microvascular complications | 65% | 72% |
| Macrovascular complications | 60% | 74% |
DM: Diabetes mellitus
DISCUSSION
In the present study, 42% of patients in the non-obese/overweight and 58% of patients in the overweight/obese group had poor diabetes control. A similar finding of more uncontrolled diabetes in the obese group was found in the Sonmez et al. study.[7]
In the present study, the prevalence of retinopathy was 21.4% that were comparable with Chawla et al. (21.2%).[8] When we compare the prevalence of nephropathy in our study (42.8%) that was similar to other studies worldwide 30–50%, a sensitive urine albumin creatinine ratio test was not done for all patients in our study groups due to financial reasons; hence, the proportion of patients with nephropathy could have been more in our diabetic patients.[9] The prevalence of neuropathy was higher in the present study population (55%) as compared with Duby et al. (30%).[10] The prevalence of IHD in our patients was more than Framingham study, this difference could be explained by the fact that Indians are at high risk of cardiac diseases [Table 4].[13]
| Various DM complications | Name of study | Prevalence (%) |
|---|---|---|
| DM retinopathy | Chawla et al.[8] | 21.2 |
| Present study | 21.4 | |
| DM nephropathy | Various studies[9] | 30–50 |
| Present study | 42.8 | |
| DM neuropathy | Duby et al.[10] | 30 |
| Present study | 55 | |
| IHD | Framingham study[11] | 33.1 |
| Present study | 40 | |
| CVA | Masod et al.[12] | 7.3 |
| Present | 13.09 |
DM: Diabetes mellitus, IHD: Ischemic heart disease, CVA: Cerebrovascular accident
As per standard literature, microvascular complications in diabetes develop after one decade of DM, but, in our study, it developed before one decade in both the groups.[8] Microvascular complications were developed early in the obese and overweight (6.5 years) group as compared with the non-obese/overweight (8.5 years) group which means obesity/overweight which is a major risk factor for microvascular complications.
In the present study, the prevalence of retinopathy was significantly higher in the obese and overweight group (26.7%) as compared with non-obese/overweight group (10.7%) which was similar to De Block et al. study.[14]
The mean serum creatinine of the obese and overweight group (2.12 mg/dL) was higher than the non-obese/overweight group (1.4 mg/dL) and similar findings were seen by Tomić et al.[15]
As opposed to De Block et al. study, when we compared neuropathy in obese/overweight (52%) and non-obese/overweight (53%) groups, it was comparable which could be due to the more vegetarian population in our region.
IHD was more common in the obese/overweight (46%) group as compared with the non-obese/overweight group (28%) in the present study that could be due to two things [Figure 3], Indians are more prone to IHD and obesity itself is a risk factor for IHD.[16]
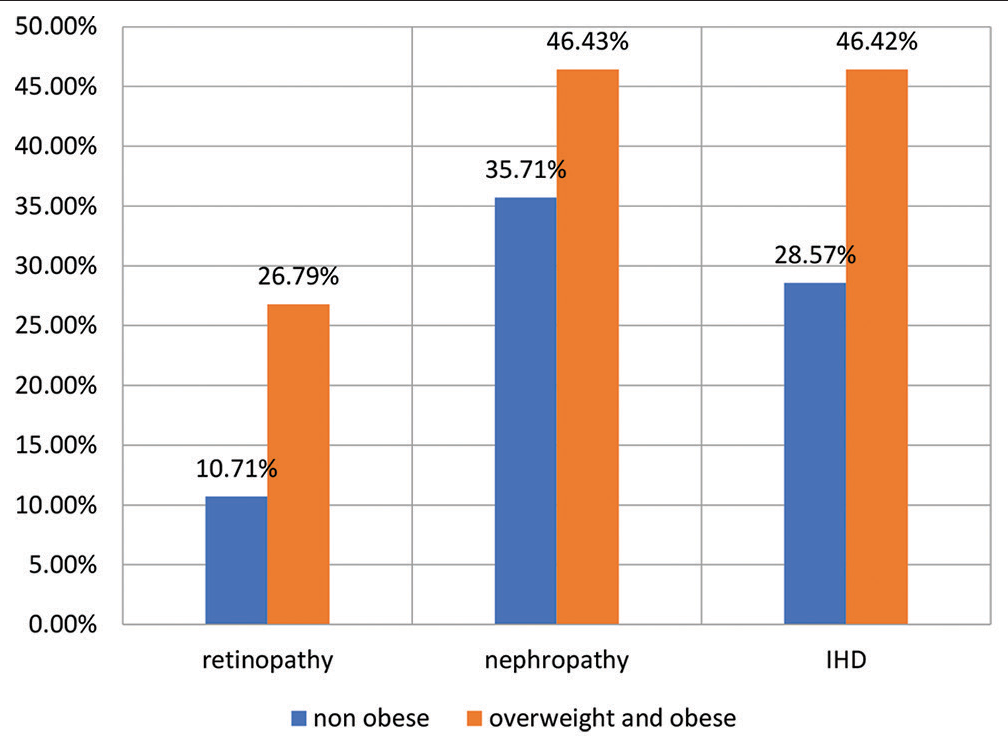
- Proportion of non-obese and overweight/obese patients with retinopathy, nephropathy and ischemic heart disease.
Limitations of our study are the small sample size, and non-availability of urine albumin creatinine test to detect nephropathy earliest. All study population is admitted patients so this might not reflect the true problem of the general population; so the prevalence of micro- and macrovascular complications in the present study might be slightly higher than the true prevalence.
CONCLUSION
Obesity is associated with a high risk of microvascular as well as macrovascular complications of diabetes, especially retinopathy, nephropathy, and IHD. It has been also observed that glycemic control is poor among obese/overweight diabetic patients. Obesity and overweight are strong risk factors for the early development of microvascular complications in type 2 DM patients. Hence, there is an unmet need to give early adequate attention to obesity/overweight management in diabetes patients.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Distribution and prevalence of major risk factors of noncommunicable diseases in selected countries: The WHO Inter-health Programme. Bull World Health Organ. 1997;75:99-108.
- [Google Scholar]
- Obesity and the metabolic syndrome in developing countries. J Clin Endocrinol Metab. 2008;93:S9-30.
- [CrossRef] [PubMed] [Google Scholar]
- Standards of Medical Care in Diabetes-2018. Available from: https://www.academia.edu/35718960/standards_of_medical_care_in_diabetes_2018 [Last accessed on 2023 Jul 22]
- [Google Scholar]
- Overweight, underweight, and mortality. A prospective study of 48,287 men and women. Arch Intern Med. 1996;156:958-63.
- [CrossRef] [PubMed] [Google Scholar]
- Consensus statement for diagnosis of obesity, abdominal obesity and the metabolic syndrome for Asian Indians and recommendations for physical activity, medical and surgical management. J Assoc Physicians India. 2009;57:163-70.
- [Google Scholar]
- Estimating GFR using the CKD Epidemiology Collaboration (CKD-EPI) creatinine equation: More accurate GFR estimates, lower CKD prevalence estimates, and better risk predictions. Am J Kidney Dis. 2010;55:622-7.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of obesity on the metabolic control of Type 2 diabetes: Results of the Turkish Nationwide survey of glycemic and other metabolic parameters of patients with diabetes mellitus (TEMD obesity study) Obes Facts. 2019;12:167-78.
- [CrossRef] [PubMed] [Google Scholar]
- Microvascular and macrovascular complications in diabetes mellitus: Distinct or continuum? Indian J Endocrinol Metab. 2016;20:546-51.
- [CrossRef] [PubMed] [Google Scholar]
- Diabetic kidney disease: World wide difference of prevalence and risk factors. J Nephropharmacol. 2015;5:49-56.
- [Google Scholar]
- Diabetic neuropathy: An intensive review. Am J Health Syst Pharm. 2004;61:160-73. quiz 175-6
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of coronary risk factors in Type 2 diabetics without manifestations of overt coronary heart disease. J Assoc Physicians India. 2009;57:135-42.
- [Google Scholar]
- Long-term complications of diabetes and co-morbidities contributing to atherosclerosis in diabetic population of Mirpur, Azad Kashmir. J Pak Med Assoc. 2013;63:1383-6.
- [Google Scholar]
- Cardiovascular disease risk factors in Asian Indian population: A systematic review. J Cardiovasc Dis Res. 2013;4:222-8.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of overweight on chronic microvascular complications in Type 1 diabetic patients. Diabetes Care. 2005;28:1649-55.
- [CrossRef] [PubMed] [Google Scholar]
- Obesity-a risk factor for microvascular and neuropathic complications in diabetes? Diabetol Croat. 2003;32:73-8.
- [Google Scholar]
- Obesity and cardiovascular disease: Pathophysiology, evaluation, and effect of weight loss: An update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2006;113:898-918.
- [CrossRef] [PubMed] [Google Scholar]






