Translate this page into:
Physician burnout: Quo vadimus?

*Corresponding author: Varun Agrawal, Division of Nephrology and Hypertension, Larner College of Medicine, University of Vermont, 1 South Prospect Street, Burlington, Vermont 05401, United States. agrawalvarun1996@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Menon V, Agrawal V, Joshi S, Ghosh AK. Physician burnout: Quo vadimus? Indian J Med Sci 2020;72(3):211-6.
Abstract
Burnout is a syndrome of emotional exhaustion, loss of meaning at work, feeling of ineffectiveness, and a tendency to view people as objects rather than as a human being. Physician burnout leads to dissatisfaction at work and suboptimal patient care. Various causes of burnout at the individual, work environment, and health system levels have been identified. In this review, we initially focus on the burden of burnout. Subsequently, we describe the determinants of this problem in India and the West, while drawing on relevant literature. Finally, we provide evidence based practical suggestions to deal with physician burnout. Strategies suggested to deal with burnout need to be implemented based on locally available resources. Repeated assessment of burnout constructs using validated questionnaires can evaluate the effectiveness of an intervention. Hospitals, educational institutions, and physician societies need to collaborate with practicing physicians to address burnout and invest in physician well-being to continue providing high-quality medical care in the future.
Keywords
Burnout
Emotional distress
Well-being
Mental health
Depression
Work–life balance
Career satisfaction
INTRODUCTION
The term “burnout” was coined by psychologist Herbert Freudenberger in the 1970s and gained prominence in the research literature after American psychologist Christina Maslach developed the Maslach Burnout Inventory (MBI) in 1981.[1] Burnout is a syndrome of emotional exhaustion, loss of meaning at work, feelings of ineffectiveness, and a tendency to view people as objects rather than as human beings.[2] The three domains of emotional health assessed in the MBI include emotional exhaustion (“I feel emotionally drained from my work”), depersonalization (“I have become more callous toward people since I took this job”), and reduced sense of personal accomplishment (“lack of feeling that I am positively influencing people’s lives through my work”).[3] Physician burnout is associated with adverse effects at the personal (relationship difficulties, substance abuse, depression, and suicide) and professional levels (decreased productivity, work and career dissatisfaction, suboptimal patient care, and physician turnover).[4] Due to these negative spinoffs, physician burnout is considered a public health crisis and also a threat to future medical practice worldwide.[5]
BURDEN OF PHYSICIAN BURNOUT
The prevalence of burnout amount attending physicians in the United States (US) is about 55% when all specialties were considered.[2] Burnout is also prevalent among medical trainees (medical students, residents, and fellows) and has been associated with self-reported medical errors and suboptimal patient care.[3] On an international level, burnout was also reported in many countries, including India [Table 1].
| Author and year of publication | Physician group | Response rate | Location | Setting | Questionnaire instrument used | Prevalence of burnout |
|---|---|---|---|---|---|---|
| Bhugra et al., 2008[9] | Private allopathic practitioners | 80% | Yamuna Nagar | Community | MBI | 5% – EE, 1% – DP, 41% - PA |
| Jugale et al., 2016[10] | Dental practitioners | 58.6% | Bangalore | Community | MBI | 5.15% |
| Langade et al., 2016[11] | Medical practitioners | 5% | Nationwide sample | Community | Abbreviated MBI and burnout clinical subtype questionnaire | 45.0% – high EE, 66.0% – high DP, 87.1% – low PA |
| Ratnakaran et al., 2016[12] | Interns and residents | 77.4% | Thiruvananthapuram | Academic institute based | CBI | 55.2% – personal burnout, 34.8% – work burnout, 35.1% – patient-related burnout |
| Chepuru et al., 2018[8] | All clinicians working in the institute | 96.9% | Vishakhapatnam | Academic institute based | MBI | 15% – high EE, 9% – high DP, 18% –low PA |
| Grover et al., 2018[13] | Residents and faculty of the institute | 27.7% | Chandigarh | Academic institute based | MBI | >90% reported some degree of burnout |
MBI: Maslach Burnout Inventory, CBI: Copenhagen Burnout Inventory, EE: Emotional exhaustion, DP: Depersonalization; PA Personal accomplishment
At present, the most widely used and validated instruments to measure burnout include the MBI, Mini-Z survey, and the Copenhagen Burnout Inventory (CBI). The MBI is the reference standard in medical research to measure burnout in various work settings. The full-length MBI is a 22-item questionnaire covering domains of emotional exhaustion, depersonalization, and personal accomplishment. Licenses need to be purchased for the use of the MBI for work-related or research use. An abbreviated two-item version developed by the Mayo Clinic has been validated and used in numerous physician surveys.[3]
The Mini-Z survey is used by the American College of Physicians, which is shorter than the MBI and free to use.[6] In addition, the Mini-Z survey is more applicable to physician settings as it includes questions on time constraints for documentation and time spent on electronic medical records at home. The CBI[7] is a psychometrically robust 19-item questionnaire that assesses burnout in three domains; personal (six items), work-related (seven items), and client-related burnout (six items). Thus, it focuses more on personal exhaustion. The CBI is free to use.
The literature on correlates of burnout from India is comparatively sparse, and the available data are inconsistent. A total of six studies have evaluated this issue [Table 1].[8-13] Of these, five have been published in the past 3 years, perhaps indicative of the growing trend, and greater interest in studying burnout. The comparison of findings across studies is limited by heterogeneity in terms of participant characteristics (internists vs. residents vs. practicing physicians) and instruments employed to assess burnout. Nevertheless, the findings are striking.
In one of the earliest studies of its kind from India, Bhugra et al.[9] reported a very low level of burnout among private practitioners in Yamuna Nagar. The authors attributed their findings to the greater degree of flexibility, control overwork, and better work-life balance than private practice provides. More recent studies, however, have contested these findings. In a nation-wide survey of medical practitioners,[11] the investigators noted high (45%–87%) prevalence of burnout across domains of emotional exhaustion and personal accomplishment. Nearly 90% of the respondents (both medical residents and faculty) in an online survey from a state-funded university hospital in Chandigarh reported concerning levels of burnout (with nearly 75% of them being at moderate or severe risk of burnout).[13]
Two studies from teaching hospitals in Vishakapatnam and Thiruvananthapuram[8,12] surveyed attending doctors and residents, respectively. Both found that nearly one-third of the respondents endorsed high burnout. Furthermore, high personal burnout was reported by more than half of the participants (51.8%).[12] Interestingly, research surveys among dental practitioners[10] have indicated lower rates of burnout (5.15%).
DETERMINANTS AND MEDIATORS OF PHYSICIAN BURNOUT
The drivers of burnout include a host of personal and work-related factors. As physicians going through rigorous medical training, compulsivity and attention to detail are a personality trait developed in us. Among physicians, culture, and values include a sense of “patient comes first” and a culture of endurance in difficult situations. This may lead to professional isolation, especially when there is no safe space to retreat or lack of social support at work. Increasing workload, varying job demands, as well as changing physician-patient dynamics and interactions have lately been contributing to emotional distress at work. Lack of control over the work schedule, inflexibility at work, and loss of autonomy based on the employer-employee relations are potential drivers of burnout.[14,15] Pressures of increased documentation time, especially using electronic medical records, and the resulting decreased face-to-face time with limited efficiency and resources add to burnout.[16] It is to be noted that burnout is not the same as depression, though interestingly, the diagnosis of physician burnout was recently added to the ICD-10 codebook.[17] Depression has a well-established process of diagnosis and treatment. A high correlation exists between burnout and depression, and it is speculated that drivers of severe burnout may lead to depression.[18]
The majority of the available Indian studies support a high prevalence of physician burnout.[8,11-13] Two studies showed a positive association between burnout and female gender,[8,11] while a couple of others did not support this association.[12,13] Positive correlates of burnout include working in clinical departments, especially surgical departments, number of years spent in residency,[8,12] and personality traits such as sociability as well as the self-control and emotionality subconstructs of emotional intelligence (EI),[19] decreased participation in recreational activities, negative encounters with patient or attendants, and lack of perceived support and empathy from senior doctors.[13]
Three major changes related to the health-care scenario in India appear to contribute to the increasing trend of physician burnout. First, the mushrooming of multispecialty corporate hospitals, which have been likened to “shopping malls,”[20] due to their offer of the entire bouquet of health services ranging from simple consultations to complex procedures such as organ transplants, all under one roof. These hospitals have a wide recruitment net, and, as a result, it has become commonplace to find doctors working outside their home state.
The earlier system of provision of care by the local family physician, who would enjoy a better rapport and understanding of the local culture and needs, has been gradually replaced by the corporate hospital culture which places a premium on patient volumes and is manned by physicians who do not share the same language and culture. This, in turn, has led to a diminution in clinician autonomy as well as reduced connectedness with patients, both of which are key drivers of burnout.[21,22]
The second issue is the supply and demand mismatch of health-care resources. This is especially true of public sector hospitals which, in India, attract high patient volumes due to the provision of subsidized health care. The available infrastructure, both in terms of workforce as well as physical infrastructure, is woefully inadequate to cater to the extant patient load. Over time, this leads to burnout due to poor working conditions.[14]
The third issue is the inequitable distribution of available health-care resources. Multispecialty hospitals and even public sector teaching hospitals are mostly located in urban areas. As the rural-urban divide in the concentration of doctors’ increases, more and more doctors practicing in urban centers are forced to compete against each other for clientele. Consequently, they often end up doing freelancing in multiple hospitals to earn better. Even private practitioners and family physicians are not spared from this phenomenon. The result is long working hours, decreased family and social time, loneliness, and eventual burnout.[23]
Given the close links between burnout and risk of cardiovascular disease,[24,25] we propose an integrated model [Figure 1] which assists in conceptualizing the above determinants of burnout from a basic cardiovascular physiology perspective. Many of these factors may operate in combination and at multiple levels to abet burnout.
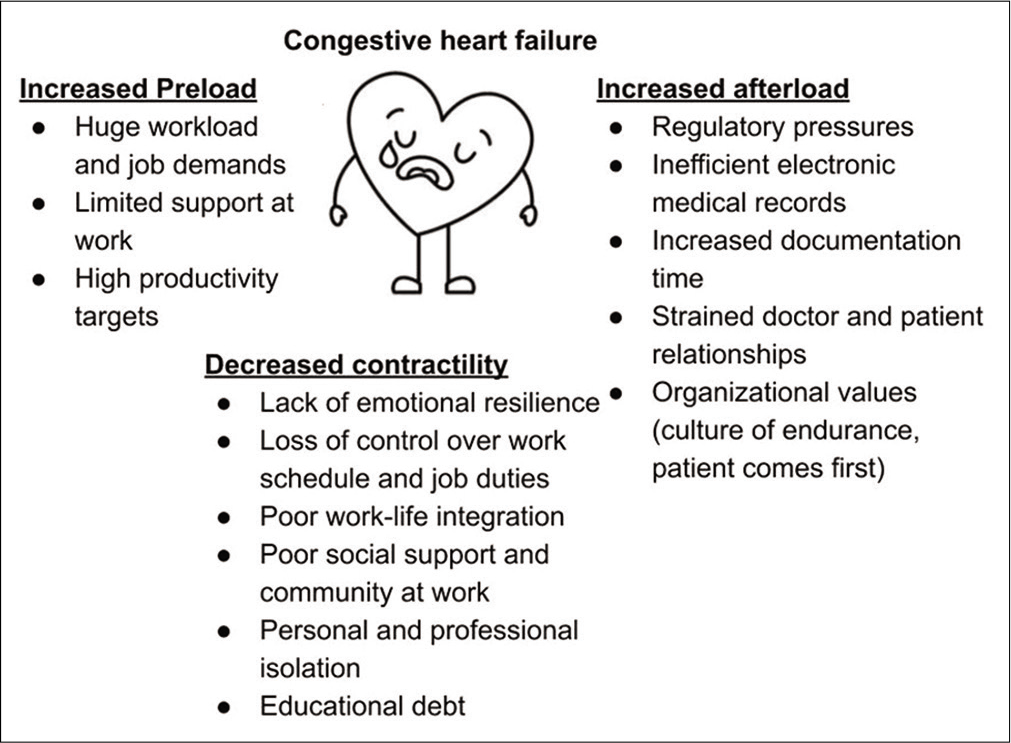
- Understanding burnout syndrome from a basic cardiovascular physiology standpoint.
STRATEGIES TO MANAGE BURNOUT
While numerous strategies have been proposed in the research literature, a strategy that may work at a certain center may not work at another institution. Thus, it is best to work collaboratively with physician leaders and a wellness committee to identify local resources to address physician well-being. Below, we give a few suggestions to improve physician well-being, from an individual and systemic perspective:
Develop work schedules to maintain work–life balance
It is important for a physician leader to acknowledge the value of the physician’s time with patients; it is equally important too to understand their need to be with their families. Life events such as disability, death or illness in the family, and maternity lead to the need for other physicians to provide coverage and may not be perceived as being cost effective. It is important to recognize that life events are inevitable. Preemptive planning and ensuring that adequate full-time staffing is available can help tide over difficult times. Flexible or part-time work may offer adequate work–life balance and are being increasingly sought by physicians.[26]
Right size documentation-related work
Clinicians are overwhelmed about the need to establish and maintain connections with patients while time may be short, and the productivity may be affected. Offloading non-clinical work such as order entry or use of scribes or medical assistants may relieve some of the pressure and improve the quality of the physician-patient interaction.
Electronic medical records have changed the way; we interact with our patients, documents, and billing. Organizations should be deliberate with electronic medical record training. The use of auto-text and auto-population for certain documentation needs and having pre-defined order sets for common diagnosis would help to improve efficiency.
Make physician wellness a priority
It is often stated that if an employer takes care of their employees and remains invested in their well-being, employees will perform better with their clients. For organizations to maintain the workforce and prevent physician turnover, it is important to make wellness a priority as this will lead to a favorable patient, provider, and financial outcomes.
It is important for the physician to be able to take adequate care of himself or herself to facilitate optimal discharge of duties. This includes eating healthy meals, exercising regularly, having an adequate sleep, mindfulness training, yoga, meditation, practicing relaxation techniques, and positive psychology, having diverse social interests, and building resilience. A physician needs to set limits to work and should not feel guilty to decline additional responsibilities, especially when having other demands at work or their personal lives.
Develop stellar leaders
It is important for an organization to have leaders who value and model well-being and, at the same time, can engage and inspire physician employees. Having a strong leader who is invested in physician well-being is an important deterrent to burnout. There is a need to destigmatize depression, especially for medical trainees, as many medical students and residents do not utilize professional mental health services when needed[27,28] and instead, prefer informal “corridor” consultations. This is undesirable and may set the tone for the trivialization of their own health issues later in life. Programs emphasizing physician well-being, leadership, and resource management skills ought to be a part of undergraduate and postgraduate training.
Mentorship programs for early career teaching faculty
Medical teachers are unique in having to juggle between the exacting demands of practicing medicine and teaching and researching. In most centers in India, there is no protected time for research activities, and it has to be squeezed into the daily grind. This may engender feelings of professional stagnation. Evidence points to low levels of perceived achievement as a risk factor for burnout.[29,30] From this standpoint, it would help to have personalized mentorship programs for junior faculty. For resource-constrained settings in low- and middle-income countries, hybrid needs driven mentoring model that incorporates matched and motivated mentor-protégé dyads, where available as well as facilitated regular peer group mentorship meetings have been described.[31]
Systems approach to the prevention of burnout
In a recent commentary based on their decade long experience with physician wellness programs, authors affiliated with the Mayo Clinic have highlighted nine organization-based strategies for the prevention of physician burnout.[4] These include admitting and acknowledging the problem, harnessing the power of leadership, developing and implementing targeted interventions for specific drivers of burnout, enhancing peer support by cultivating work communities, incentivization of productivity among physicians, and promoting flexibility at the workplace so that physicians can adjust their timings to meet personal and professional obligations, implementing organizational programs that foster physician resilience and self-care and institutional investment in sustained programs.
Of these, workplace flexibility is a key issue in most of the Indian medical schools, which come under the ambit of the Medical Council of India. These institutions have to maintain biometric attendance records for faculty, which are reviewed during periodic inspections by the national body. A late login means half a day’s leave that is deducted while a late logout due to exigencies of work gives little extra credit. As a result, there is little to no flexibility in work timings or incentivization of productivity. It is no wonder then that the focus is more on logging in and out at the correct time than being productive at the workplace.
In India, the extant physician culture is one of being available and responsible for patients 24×7. This mindset of self-sacrifice must be replaced with a culture that equally values physician self-care and wellness. Doubtless, medicine is a service-oriented profession, but unless a physician is healthy, he/she cannot function optimally. It is not going to be easy to change attitudes and cultures, and for this to happen, change must begin at the top.
In resource-constrained settings like India, strict on-duty and off-duty hours as well as limiting workload of residents may be difficult to implement. A more workable and evidence-based solution could be to design interventions that enhance emotional intelligence (EI) and, potentially, prevent burnout. Inclusion of EI abilities in the curriculum, use of simulated patients to improve EI, and regular workshops to enhance EI, communication skills, and emotion self-regulation[32] have all been suggested. EI is trainable and brief training programs have been found to induce sustainable changes in levels of EI.[33]
In summary, a combination of institutional and individual strategies is required, given the lack of evidence of superiority for any particular intervention in reducing burnout.[34]
CONCLUSION
“Quo vadimus” refers to the process where we ask ourselves the question, “where do we go from here?.” Burnout is a growing problem in the practice of medicine and is best considered a long-term reaction to stress. Various predictors have been identified, such as diminished clinician autonomy, poor medical infrastructure, impaired work–life balance, reduced sense of personal accomplishment, and lack of support and empathy from senior colleagues. However, physician burnout is not inevitable. Understanding the predictors of burnout, implementing locally relevant strategies based on locally available resources, and reassessing physician well-being can go a long way in addressing physician burnout and emotional well-being. We owe this effort to our physician brethren and our patients.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Burnout: A short socio-cultural history. Burnout, Fatigue, Exhaustion: An Interdisciplinary Perspective on a Modern Affliction 2017:105-27.
- [CrossRef] [Google Scholar]
- Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90:1600-13.
- [CrossRef] [PubMed] [Google Scholar]
- Concurrent validity of single-item measures of emotional exhaustion and depersonalization in burnout assessment. J Gen Intern Med. 2012;27:1445-52.
- [CrossRef] [PubMed] [Google Scholar]
- Executive leadership and physician well-being: Nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. 2017;92:129-46.
- [CrossRef] [PubMed] [Google Scholar]
- Potential impact of burnout on the US physician workforce. Mayo Clin Proc. 2016;91:1667-8.
- [CrossRef] [PubMed] [Google Scholar]
- Worklife and wellness in academic general internal medicine: Results from a national survey. J Gen Intern Med. 2016;31:1004-10.
- [CrossRef] [PubMed] [Google Scholar]
- The Copenhagen burnout inventory: A new tool for the assessment of burnout. Work Stress. 2005;19:192-207.
- [CrossRef] [Google Scholar]
- Burnout among clinicians in tertiary care setting. Int J Community Med Public Health. 2018;5:1157.
- [CrossRef] [Google Scholar]
- Burnout and stress among doctors and dentists in North India. Int J Cult Ment Health. 2008;1:24-9.
- [CrossRef] [Google Scholar]
- Burnout and work engagement among dental practitioners in Bangalore City: A cross-sectional study. J Clin Diag Res. 2016;10:ZC63-7.
- [CrossRef] [PubMed] [Google Scholar]
- Burnout syndrome among medical practitioners across India: A questionnaire-based survey. Cureus. 2016;8:e771.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of burnout and its correlates among residents in a tertiary medical center in Kerala, India: A cross-sectional study. J Postgrad Med. 2016;62:157-61.
- [CrossRef] [PubMed] [Google Scholar]
- Psychological problems and burnout among medical professionals of a tertiary care hospital of North India: A cross-sectional study. Indian J Psychiatry. 2018;60:175-88.
- [CrossRef] [PubMed] [Google Scholar]
- Factors related to physician burnout and its consequences: A review. Behav Sci (Basel). 2018;8:98.
- [CrossRef] [PubMed] [Google Scholar]
- Trends and factors associated with physician burnout at a multispecialty academic faculty practice organization. JAMA Netw Open. 2019;2:e190554.
- [CrossRef] [PubMed] [Google Scholar]
- Allocation of physician time in ambulatory practice: A time and motion study in 4 specialties. Ann Intern Med. 2016;165:753-60.
- [CrossRef] [PubMed] [Google Scholar]
- ICD-10 Classifications of Mental and Behavioural Disorder: Clinical Descriptions and Disgnostic Guidelines Geneva: World Health Organization; 1992.
- [Google Scholar]
- Physician burnout is better conceptualised as depression. Lancet. 2017;389:1397-8.
- [CrossRef] [Google Scholar]
- Correlation among perceived stress, emotional intelligence, and burnout of resident doctors in a medical college of West Bengal: A mediation analysis. Indian J Public Health. 2018;62:27-31.
- [Google Scholar]
- Health care becomes an industry: The growing influence of corporate and multi-speciality hospitals In: Dissenting Diagnosis. Gurgaon: Random House Publishers India Private Ltd; 2016. p. :44-59.
- [Google Scholar]
- How to prevent burnout in cardiologists? A review of the current evidence, gaps and future directions. Trends Cardiovasc Med. 2018;28:1-7.
- [CrossRef] [PubMed] [Google Scholar]
- Physician burnout: Contributors, consequences and solutions. J Intern Med. 2018;283:516-29.
- [CrossRef] [PubMed] [Google Scholar]
- Residency as a social network: Burnout, loneliness, and social network centrality. J Grad Med Educ. 2015;7:617-23.
- [CrossRef] [PubMed] [Google Scholar]
- Psychosocial risk factors and cardiovascular disease: Epidemiology, screening, and treatment considerations. Cardiovasc Innov Appl. 2016;1:417-31.
- [CrossRef] [Google Scholar]
- Burnout and risk of cardiovascular disease: Evidence, possible causal paths, and promising research directions. Psychol Bull. 2006;132:327-53.
- [CrossRef] [PubMed] [Google Scholar]
- Part-time doctors-reducing hours to reduce burnout. CMAJ. 2018;190:E1055-6.
- [CrossRef] [PubMed] [Google Scholar]
- Utilization and barriers to mental health services among depressed medical interns: A prospective multisite study. J Grad Med Educ. 2010;2:210-4.
- [CrossRef] [PubMed] [Google Scholar]
- Barriers to healthcare seeking among medical students: A cross sectional study from South India. Postgrad Med J. 2015;91:477-82.
- [CrossRef] [PubMed] [Google Scholar]
- Risk of burnout in Danish GPs and exploration of factors associated with development of burnout: A two-wave panel study. Int J Fam Med. 2013;2013:1-8.
- [CrossRef] [PubMed] [Google Scholar]
- Factors associated with burnout among residents in a developing country. Ann Med Surg (Lond). 2016;6:60-3.
- [CrossRef] [PubMed] [Google Scholar]
- Mentoring for junior medical faculty: Existing models and suggestions for low-resource settings. Asian J Psychiatry. 2016;19:87-8.
- [CrossRef] [PubMed] [Google Scholar]
- Emotional intelligence, perceived stress and burnout among resident doctors: An assessment of the relationship. Natl Med J India. 2013;26:210-3.
- [Google Scholar]
- Increasing emotional intelligence: (How) is it possible? Pers Individ Dif. 2009;47:36-41.
- [CrossRef] [Google Scholar]
- Interventions to prevent and reduce physician burnout: A systematic review and meta-analysis. Lancet. 2016;388:2272-81.
- [CrossRef] [Google Scholar]






