Translate this page into:
Post-donation telephonic interview: A tool for active follow-up of voluntary whole blood donors for analysis of frequency and predisposing factors of adverse reactions
*Corresponding author: Priti Desai, Department of Transfusion Medicine, Tata Memorial Hospital, Homi Bhabha National Institute, Mumbai, Maharashtra, India. dr_priti99@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Navkudkar A, Desai P, Rajadhakshaya S. Post-donation telephonic interview: A tool for active follow-up of voluntary whole blood donors for analysis of frequency and predisposing factors of adverse reactions. Indian J Med Sci 2021;73:317-22.
Abstract
Objectives:
Blood donation experience by most donors is satisfactory; however, a few may encounter adverse reactions. Healthy, altruistic, voluntary blood donors ensure adequate blood supply despite the potential risk of adverse reactions. Post-donation follow-up is crucial to get information about these adverse reactions. This study aimed to evaluate the frequency and type of adverse donor reactions and their correlation with contributory factors if any among the blood donors in a tertiary care oncology center.
Material and Methods:
It was a prospective observational study of 1000 consecutive voluntary whole blood donors who consented to participate in the study. Donors were followed up telephonically on two instances (first after 24 h of donation and second after 2 weeks of donation) and were asked a self-structured donor questionnaire to collect information regarding the adverse donor reactions if any. An appropriate statistical tool was used for analysis (IBM, SPSS software).
Results:
Of the 1000 voluntary whole blood donors, 92.6% (926/1000) responded to telephonic calls on both occasions. Of these 926, 8.5% (79/926) donors experienced adverse reactions. All these donors experienced immediate reactions, that is, within 24 h of donation while none reported fresh adverse reactions beyond 24 h–2 weeks. Of the 79 donors, 60% (49/79) experienced vasovagal reactions (VVR) and 40% (32/79) experienced hematoma including two donors who experienced both. A total of 86% (68/79) of reactions occurred in outdoor blood donation camps while 14% (11/79) occurred in-house (indoor). First time donors, female donors, and donors with weight on the lower side were more prone to immediate VVR (P < 0.05). Of the 49 VVR, 76% (37/49) were mild, 18% (9/49) were moderate, and 6% (3/49) were severe. Most of the hematomas, that is, 90% (29/32) occurred at outdoor blood donation camps while 10% (3/32) occurred indoor. Most hematomas (53%) took more than 7 days to recover.
Conclusion:
Post-donation interview proves to be an efficient tool to acquire information about adverse donor reactions. This will help in improving donor safety and satisfaction and will have a positive impact on the national blood supply by improving the donor return rate. Blood transfusion services (BTSs) staff must be trained to promptly identify the donor reactions onsite and manage them to enhance the donation experience of voluntary donors. Post-donation follow-up will aid in getting the donation experience and BTS can develop strategies to enhance it. This will also help in donor hemovigilance in the future for the betterment of donor safety.
Keywords
Whole blood donors
Adverse reactions
Vasovagal reactions
Hematoma
Post-donation telephonic interview
INTRODUCTION
The increasing demands of blood component requirement in any health-care center can be satisfied with whole blood donation by healthy voluntary blood donors. The WHO recommends repeat, voluntary, non-remunerated blood donors to ensure blood safety.[1] Safe blood donation depends on, building a panel of regular, voluntary, and non-remunerated donors as the first step in ensuring a safe and adequate supply of blood. Care of the donor is essential to an effective donation process.[2] Transfusion medicine is concerned not only with patient safety but also with donor safety. Blood donation is considered a safe procedure but some donors may experience adverse reactions.[3,4] In general, donors typically do not require significant medical intervention and readily recover without lasting sequel.[5] It is necessary to monitor donor during and after blood donation. To ensure donor safety, collection staff must also be aware of potential donor reactions and must be trained in procedures for reaction management. Voluntary blood donors are the cornerstone of a safe and adequate supply of blood and blood components. Hence, blood donor safety is of the utmost importance. A healthy donor can donate blood 8–9 ml/kg body weight.[2] The blood donation experience should be pleasant to retain blood donors for regular blood donation. This, in turn, is important to manage the inventory of blood and blood components to meet the increasing demands. Removal of blood during the donation process is physiologically well tolerated by most of the donors; except for a few donors who experience adverse donor reactions. Most of the adverse reactions occur during or within 15 min of blood donation and are managed by simple measures. Adverse donor reactions can be broadly classified as vasovagal and hematoma.[5] Vasovagal reactions (VVRs) occur in 2–7% of blood donations.[6-10] Newman et al. showed the occurrence of VVR in 5–10% donors and hematoma in 0.9–2%.[11] Abhishekh et al. showed the occurrence of VVR in 2–5% and hematoma in 0.88%.[12] The most adverse reaction occurs in the refreshment area while a few reactions occur after the donor has left the donation site. A study by Newman et al. has shown that syncopal reaction is the most common adverse reaction, 60% of which occurs in the refreshment area while 12% occur after the donor has left the donation site.[13] Adverse reactions can also be classified as immediate and delayed adverse reactions (DARs). Reactions that occur during or immediately after blood donations are called immediate adverse reactions (IARs).[3,4,14-17] Reactions that occur after the donor has left the donation site are called DARs.[18-20] Adverse reactions that occur at the collection site are being managed by the donor clinic staff, and they are documented. Hence, information about these reactions is available while minimal information is available regarding DARs. A possible reason could be, as delayed donor reactions are self-limiting hence not informed to blood transfusion services (BTSs) by the donor, and the donor may seek outside medical care. Proactive follow-up of donors for delayed reactions is not done routinely by BTS. The study of adverse donor reactions is important because by analyzing this information, corrective measures can be taken to minimize and avoid adverse donor reactions. Furthermore, donors predisposing to the development of adverse reactions can be identified and additional attention can be given during the post-donation period. In the long run, this will help us in enhancing donor satisfaction and hence donor retention. Tomita et al. and Bruce et al. have studied the effect of donor adverse reactions on donor return rate for repeat donations. According to their findings, pre-syncope and syncope reactions decreased blood donor return rates by 29–37% and 58–78%, respectively.[21,22] Bruise and hematoma which occur after phlebotomy do not prevent donors from donating again.[23] These types of studies are also important to understand the various factors affecting donor experience and donor satisfaction. Therefore, the study aimed to analyze the comprehensive overview of immediate and DARs in whole blood donors. Therefore, the study aimed to analyze the comprehensive overview of immediate and delayed adverse reactions in whole blood donors. Also, to estimate the frequency and type of adverse reactions to study various predisposing factors like age, gender, place of donation, donation status, etc. which may correlate with adverse donor reactions.
MATERIAL AND METHODS
A prospective observational study was conducted over 2 months to evaluate adverse reactions in 1000 whole blood donors. The first 1000 blood donors who consented to participate in the study in the given period were included for the analysis. These blood donors were followed up by a telephonic interview on two occasions; once after 24 h and another after 2 weeks of donation. The study was approved by the Institutional Ethics Committee and enrolled in the Clinical Trials Registry India (CTRI/2016/09/007320). Donor selection, donation procedure, post-donation care, management of adverse donor reactions, and documentation were done as per the standard operating procedure of the department of transfusion medicine. Donors were asked a structured questionnaire and information was documented. Immediate reactions defined in the study were those occurring within 24 h of donation while delayed reactions were those which occurred between 24 h and 2 weeks of donation [Figure 1].
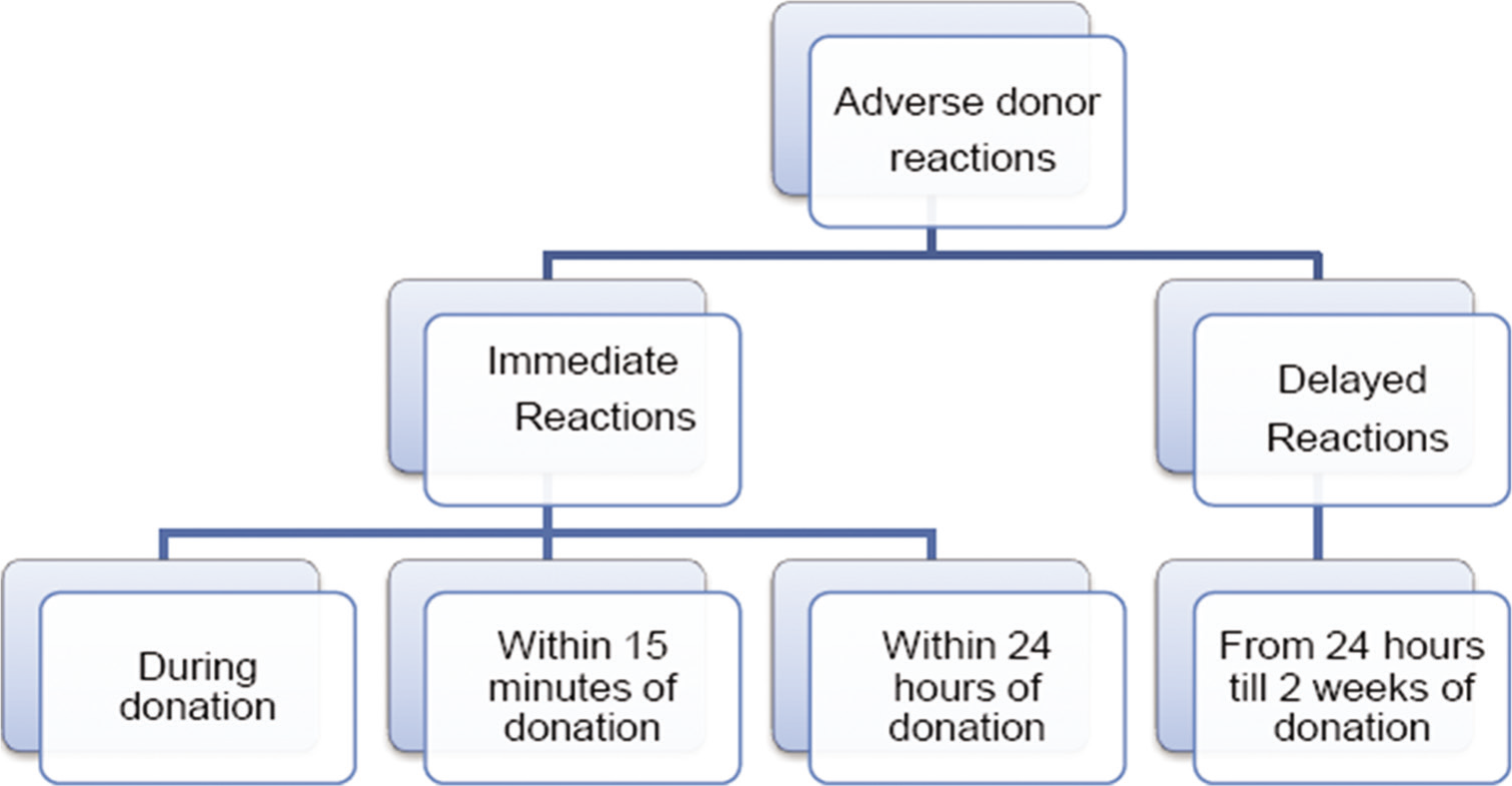
- Categorization of adverse donor reactions.
Statistical analysis
The overall analysis of the data was descriptive with results presented as a percentage for categorical data. Statistical analysis was done using SPSS software. Statistical inferential analysis was carried out on the collected data to ascertain if there were any significant associations or independent factors.
RESULTS
Of the 1000 whole blood donors; 948 donors responded to phone calls on the first occasion, and of the 948 donors, 926 donors responded to the phone calls on both occasions. Evaluation of the final 926 donors was done to study immediate and delayed adverse donor reactions. Demographic details of all blood donors are shown in Table 1. Total 8.5% of donors (79/926) experienced IAR including five donors who had added complaints beyond 24 h [Table 2]. None of the donors experienced DARs. VVRs were experienced by 47 donors (5%) while 32 donors (3%) experienced hematoma symptoms and 2 donors experienced both reactions. Table 3 shows the donor characteristics and types of donor reactions. The adverse reactions in female donors were significantly higher than compared to male donors (25% vs. 6%) (P < 0.001). The adverse reactions in donors of 18–25 years’ age group were higher (10%) as compared to other age group donors, but not statistically significant (P > 0.05). Donors with a lower weight range group (45–60 kg) experienced more adverse reactions (13%) as compared to donors with other weight groups (P < 0.05). First time donors had a vasovagal reaction rate of 8% as compared to 3% in repeat donors (P < 0.05). The rate of adverse reactions was higher in outdoor blood donation camps (9%) as compared to indoor blood donation (5%) (P < 0.05). Of the total VVRs; 76% were mild, 18% were moderate, and 6% were severe with fear, anxiety, and inadequate fluid intake being a few factors for VVR. Of the 49 donors with VVR, 27% of donors complained of fear and anxiety of donation and all these were 1st time donors, 18% gave the history of inadequate water/fluid intake while in 55% of donors, no associated factors were reported. Most of the hematoma (53%) took more than a week to recover.
| Total number of donors | 926 |
|---|---|
| Male donors(%) | 809(87) |
| Female donors(%) | 117(13) |
| Mean age(years)±SD | 30.35±9.7 |
| Mean weight(kg)±SD | 73.2±13.1 |
| Mean systolic BP(mmHg)±SD | 121.5±11.2 |
| Mean diastolic BP(mmHg)±SD | 78.9±5.2 |
| Total number of adverse donor reactions | Immediate adverse donor reactions (reactions within 24 h of donation) | Delayed adverse donor reactions (reactions from 24 h to 2weeks of donation) |
|---|---|---|
| 79(8.5%)(79/926) | 79*(100%) | 0** |
| Donor or donation characteristics | Total number of donors | All reactions | VVRs | Hematoma |
|---|---|---|---|---|
| Overall reactions | 926 | 79(8.5%) | 49*(5%) | 32(3.5%) |
| Gender | ||||
| Male | 809 | 50(6%) | 32(4%) | 18(2%) |
| Female | 117 | 29(25%) | 17*(15%) | 14(10%) |
| P-value | <0.001 | <0.001 | <0.001 | |
| Age group(years) | ||||
| 18–25 | 326 | 32(10%) | 26*(8%) | 7(2%) |
| 26–40 | 454 | 33(8%) | 17*(4%) | 17(4%) |
| 41–50 | 116 | 11(9%) | 5(4%) | 6(5%) |
| 51–65 | 30 | 3(9%) | 1(3%) | 2(6%) |
| P-value | >0.05 | >0.05 | >0.05 | |
| Weight group(kg) | ||||
| 45–60 | 155 | 20(13%) | 10 *(6%) | 12(7%) |
| 61–75 | 422 | 43(10%) | 31(7%) | 12(3%) |
| 76–100 | 324 | 15(4%) | 8(2%) | 7(2%) |
| >100 | 25 | 1(4%) | 0(0%) | 1(4%) |
| P-value | <0.05 | <0.05 | <0.05 | |
| Donation status | ||||
| First | 389 | 39(10%) | 32*(8%) | 9(2%) |
| Repeat | 537 | 40(7%) | 17(3%) | 23(4%) |
| P-value | >0.05 | <0.001 | >0.05 | |
| Donation place | ||||
| Outdoor | 717 | 68(9%) | 41*(6%) | 29(3%) |
| Indoor | 209 | 11(5%) | 8(4%) | 3(1%) |
| P-value | =0.05 | >0.05 | <0.05 | |
| Severity of VVR | ||||
| Mild | 49* | 37(76%) | ||
| Moderate | 9(18%) | |||
| Severe | 3(6%) | |||
| Recovery for hematoma | ||||
| <2days | 32 | 2(6%) | ||
| Up to 1week | 13(41%) | |||
| 1–2weeks | 17(53%) |
DISCUSSION
Blood donation is a safe process. It is important to identify the adverse donor reactions and the risk factors associated with them and manage to improve the blood donation experience. The incidence of adverse reactions in blood donors in different studies ranged from 2% to 7%.[6-10] Most studies analyzed the adverse donor reactions occurring during the blood collection process and did not include a post-donation follow-up of the donor.[4-9] One of the recent Indian studies showed that the post-donation interview increased the detection rate of blood donor adverse reactions to 10.3%.[24] The post-donation telephonic interview approach allowed the blood center to better understand the findings and this could potentially be used to improve comfort and donor safety.[24] In the present study, a total of 79 donors (8.5%) experienced adverse reactions. All 79 donors experienced IARs while exclusively DARs were experienced by none. Five donors experienced immediate reactions and had added complaints beyond 24 h (0.5%). One of the studies of 1000 blood donors interviewed after 3 weeks of the whole blood donation showed that 36% of donors had adverse reactions.[11] The difference in incidence rates of immediate and DARs in the present study and other studies was due to the difference in study design and timing of phone calls. In the present study, the donors were followed-up on two occasions. In a study by Newman et al., the donors were interviewed only on one occasion; directly after 3 weeks of donation to identify any DARs.[11] Adverse reactions were then broadly divided into VVRs and hematoma. In the present study, it was observed that the incidence of VVRs was 5% (49/926) and the hematoma was 3.4% (32/926). Other studies showed the incidence of vasovagal reaction in 2–10% of donors and hematoma in 0.8–2%.[11,12] In the present study, the incidence of adverse reaction rate was 8.5% (79/926); with 60% (49/79) VVRs and 40% (32/79) hematoma reactions; similar to a study by Agnihotri et al.[4] Both VVRs and hematoma categories were further analyzed by categorizing the donors based on age, weight, gender, blood donation status, donation place, education, and occupation.
Subgroup analysis by age
It was observed that total adverse reactions in donors 18–25 years of age group were higher (10%) as compared to other age group donors but without any statistical significance. Newman et al. and Dhidah et al. reported that VVRs were increased in donors who were <30 years old.[11,24] American Hemovigilance Program showed young donors. A study by France postulated that baroreceptor sensitivity is decreased in healthy young individuals when they are physically or psychologically stressed and with increasing age, the body becomes more stable hemodynamically.[25]
Subgroup analysis by weight
The frequency of adverse reactions was analyzed in donors with different weight groups, and it showed a higher frequency (13%) in donors with 45–60 kg weight groups (P < 0.05). The frequency of VVRs decreased as the weight of donor increased from 45 kg to more than 100 kg (P < 0.05). Hematoma also showed a significant difference in donors of 45–60 kg weight group as compared to other groups (P < 0.05). These findings are similar to studies by Agnihotri et al. and Trouern-Trend et al.[4,6] This may be explained by the greater percentage of blood volume lost in smaller donors.[6] The mean weight of the donors who had a vasovagal reaction was less than the mean weight of the total donor population, an observation reported by Kasprisin et al. who also observed lower weight donors may exacerbate hypovolemia.[26]
Subgroup analysis by gender
Higher adverse reactions were observed in females than males (25% vs. 6%) (P < 0.001). Statistical significance was found for both VVR and hematoma in females as compared to males (P < 0.05). Similar results were also observed by Bhardwaj et al.[27] Newman et al. concluded that men were half as likely as women to have an adverse effect (AE) (23% AE vs. 48% AE, P < 0.001).[10] Takanashi et al. showed that VVR group had more female donors.[14]
Subgroup analysis by donation status
Overall adverse reactions in the 1st time donors were higher than repeat donors. VVRs were higher in the 1st time than repeat donors (P < 0.001); while the frequency of hematoma was higher in repeat than 1st time donors. Newman showed that the 1st time donor had a vasovagal reaction rate of 9.4% versus 3.8% in a repeat donor while repeat donors had 60% reduction in their vasovagal reaction rate.[11] Eder et al. showed a correlation of higher syncopal complication rates after whole blood donation in the 1st time donors.[28] Possible reasons could be; 1st time donors are usually apprehensive and anxious about blood donation, they tend to be more conscious of any discomfort post-donation.
Subgroup analysis by place of donation
Adverse reactions at outdoor camps were higher than compared to in-house donations (P < 0.05). VVRs and hematoma reactions at outdoor camps were higher than compared to in-house donations but statistical significance was observed only in hematoma reactions (P < 0.05). Similar results were reported by Mahapatra et al. and Agnihotri et al.[4,29]
Education and occupation and adverse reactions
Educational qualification and occupation had no statistical significance with adverse donor reactions.
Other contributing factors
Some reasons observed in the donors experiencing VVRs were fear or anxiety of donation and inadequate water or fluid intake before the donation. Hematoma or bruise was attributed to strain on the donated arm during travel by public transport in most of the cases as reported by the donors during the telephonic interview. Furthermore, immediate post-donation proper arm care was not taken by many donors, especially in the outdoor blood donation camps of corporate sectors and educational institutes where the donors were always in rush despite being advised otherwise.
Importance of post-donation interview
Donors are encouraged by many blood centers to report the adverse reactions which occur after the donor has left the donation site, but still, only a few donors report the BTS actively. Thus, it remains a challenge to acquire accurate information regarding the DARs. Thus, an active follow-up in the form of a post-donation interview proves to be an effective tool to acquire this information. The information must be utilized in understanding factors contributing to it and thus providing better donor care. The donor’s physical experience has a significant impact on the willingness to return and donate blood. Blood donor return rate is dependent on the type of AE. Various studies have shown that donors who sustained donor reactions are less likely to return.[21,22] Hence, BTS should take some measures to minimize adverse donor reactions.
Some of the suggested recommendations to decrease donor reaction rates include
Information should be provided to each donor regarding post-donation care in the form of pamphlets/leaflets or displayed at the donation site in the form of reading material or standees.
First time donors, low weight donors, and female donors are more prone to get VVRs and hence such donors should be given more attention for a longer time.
-
For VVRs, the following measures should be taken:
Management of adverse reactions should be prompt for reactions that occur at the donation site.
All donor clinic staffs should be well trained in identifying and managing adverse donor reactions. Most of the VVRs are mild. A few donors experience reactions that are moderate to severe.
Anxiety and fear of the donors can be allayed by engaging them in conversations or playing light music to create an ambience for donation.
-
For hematoma reactions, the following measures should be taken:
Staff should be well trained in phlebotomy. Proper instructions to be given to the donor to strictly keep the venepuncture site pressed with dressing for 10– 15 min post-donation.
Donors should be advised to avoid strenuous activity which might cause hematoma in the donated arm.
Donors should be counseled about post-donation arm care at the venepuncture site.
Donors should be given the contact information of the blood center and should be encouraged to report any adverse reactions if experienced by them.
A follow-up call should be made to enquire about any adverse reactions experienced by the donors and to provide appropriate advice.
CONCLUSION
These types of studies are important to understand the various factors affecting donor experience and donor satisfaction, thus improving donor care and eventually helping in donor retention. This will help in improving donor safety and will have a positive impact on the donor return rate. Donor area staff should be trained to enhance the donation experience of voluntary donors. Post-donation follow-up will help in getting donors’ experience about the donation and BTS can develop strategies to enhance it.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Transfusion Medicine Technical Manual. Directorate General of Health Services (DGHS) Ministry of Health and Family Welfare (2nd ed). New Delhi: Government of India; 2003.
- [Google Scholar]
- Adverse reactions in whole blood donors: An Indian scenario. Blood Transfus. 2011;9:46-9.
- [Google Scholar]
- Analysis of adverse events and predisposing factors in voluntary and replacement whole blood donors: A study from north India. Asian J Transfus Sci. 2012;6:155-60.
- [CrossRef] [PubMed] [Google Scholar]
- On-site and off-site adverse donor reactions in voluntary whole blood donors: A study from a tertiary care oncology center. Glob J Transfus Med. 2019;4:28-32.
- [Google Scholar]
- A case-controlled multicenter study of vasovagal reactions in blood donors: Influence of sex, age, donation status, weight, blood pressure, and pulse. Transfusion. 1999;39:316-20.
- [CrossRef] [PubMed] [Google Scholar]
- An analysis of the incidence of “fainting” in 5, 897 unselected blood donors. Br Med J. 1942;1:253-5.
- [CrossRef] [PubMed] [Google Scholar]
- Study of the incidence and characteristics of blood donor “reactors”. Transfusion. 1963;3:76-82.
- [CrossRef] [PubMed] [Google Scholar]
- A study of criteria for blood donor deferral. Transfusion. 1980;20:511-8.
- [CrossRef] [PubMed] [Google Scholar]
- Adverse effects in blood donors after whole-blood donation: A study of 1, 000 blood donors interviewed 3 weeks after whole-blood donation. Transfusion. 2003;43:598-603.
- [CrossRef] [PubMed] [Google Scholar]
- Donor reactions and injuries from whole blood donation. Transfus Med Rev. 1997;11:64-75.
- [CrossRef] [Google Scholar]
- A retrospective study of adverse events in blood donors from Navi Mumbai. J Evol Med Dent Sci. 2013;2:1575-80.
- [CrossRef] [Google Scholar]
- Donor hemovigilance programme in managing blood transfusion needs: Complications of whole blood donation. J Pathol Nepal. 2013;3:459-63.
- [CrossRef] [Google Scholar]
- Complications associated with blood donation in blood bank at an Indian tertiary care hospital. J Clin Diagn Res. 2014;8:JC5-8.
- [Google Scholar]
- Study of adverse whole blood donor reactions in normal healthy blood donors: Experience of tertiary health care centre in Jammu region. Indian J Hematol Blood Transfus. 2015;31:142-5.
- [CrossRef] [PubMed] [Google Scholar]
- Delayed adverse reactions to blood donation: From haemovigilance data to specific studies. Transfus Med. 2005;15:389-94.
- [CrossRef] [PubMed] [Google Scholar]
- Training Module for Blood Bank Nurses, National Aids Control Organisation (NACO), Ministry of Health and Family Welfare Government of India.
- [Google Scholar]
- Delayed adverse reactions to blood donation. Transfusion. 2010;50:556-65.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of whole-blood donor adverse events on blood donor return rates. Transfusion. 2006;46:1374-19.
- [CrossRef] [PubMed] [Google Scholar]
- Complications of blood donation in Morocco (during and immediately after the donation) Transfus Clin Biol. 2007;14:440-5.
- [CrossRef] [PubMed] [Google Scholar]
- Baroreflex sensitivity during noxious stimulation in vasovagal reactors to blood donation. Int J Psychophysiol. 1995;19:13-22.
- [CrossRef] [Google Scholar]
- Moderate and severe reactions in blood donors. Transfusion. 1992;32:23-6.
- [CrossRef] [PubMed] [Google Scholar]
- Adverse donor reactions in whole blood and blood component donors of a tertiary care hospital of Punjab, India. Res J Pharm Biol Chem Sci. 2014;5:306-13.
- [Google Scholar]
- The American red cross donor hemovigilance program: Complication of blood donation reported in 2006. Transfusion. 2008;48:1809-19.
- [CrossRef] [PubMed] [Google Scholar]
- Adverse events in blood donors and adoption of measures to reduce such occurrence. Int J Med Res Prof. 2016;2:62-5.
- [Google Scholar]






