Translate this page into:
Psychological impact of COVID-19 pandemic on health-care professionals in India – A multicentric cross-sectional study

*Corresponding author: Preethi Selvaraj, Department of Community Medicine, Assistant Professor, SRMMCH and RC, SRM Institute of Science and Technology, Kancheepuram, Tamil Nadu, India. preenessy@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Selvaraj P, Muthukanagaraj P, Saluja B, Jeyaraman M, Anudeep TC, Gulati A, et al. Psychological impact of COVID-19 pandemic on health-care professionals in India – A multicentric cross-sectional study. Indian J Med Sci 2020;72(3):141-7.
Abstract
Objectives:
The world is grappling with an ongoing COVID-19 pandemic that has shaken the mankind to the core and disrupted the lives of everyone. The aim of the study was to assess the presence of psychological distress, depression, anxiety, stress, and insomnia experienced by the Indian healthcare workers.
Material and Methods:
A cross-sectional study was conducted in India among 777 doctors to evaluate the mental health of doctors working in Corona wards from April 2020 to May 2020 using a pre-designed, pre-tested validated, semi-structured DASS-21 questionnaire, and the Insomnia Severity Index. Continuous variables between the groups were measured using the Mann–Whitney U-test and the Kruskal–Wallis H test.
Results:
Among the doctors working for the pandemic, around 55% of medical officers in the study reported having moderate levels of depression. With respect to anxiety, it was found that among men as many as 52% reported experiencing severe anxiety and 24% had moderate levels of anxiety whereas females reported as high as 68% and 48% of moderate and severe anxiety, respectively. In our study, around 30% and 44% of male doctors reported mild and moderate levels of stress, respectively, whereas 70% and 56% of female doctors reported mild and moderate levels of stress, respectively. It was also observed that among female doctors the rates of moderate insomnia were especially high (65%), whereas a high level of male participants reported sub-threshold insomnia (52%).
Conclusion:
Early screening targeting the medical workforce and the implementation of psychological interventions is essential for protecting and maintaining the functionality of the health-care system.
Keywords
Pandemic
Corona virus disease-19
Mental health
Healthcare workers
Depression
Anxiety
INTRODUCTION
The world is grappling with an ongoing COVID-19 pandemic that has shaken the mankind to the core and disrupted the lives of everyone. As of August 10, 2020, India stands third in the world with 2,215,074 cumulative cases and death rate of 2% (44,396 deaths).[1] SAARC regions includes over 21% of the total population which stays vulnerable toward COVID-19. The Member States have revealed 3,019,961 cases, an aggregate of 58,162 deaths in the locale, and 2,162,165 recovered cases.[2] The World Health Organization has announced COVID-19 a Global Public Health Crisis.[3] It has not only bought life to a standstill personally and professionally, but has also cast its impact on the psychological well-being of everyone around the globe thereby hampering the psychological resilience and coping abilities of individuals. This has presented the health-care systems worldwide with a novel and catastrophic risk for which presently no breakthrough has been discovered leading to further anxiety and fear of this never ending uncertainty. Doctors and nurses who are considered as the frontliners for dealing with this pandemic at point blank range are the most vulnerable to develop mental health concerns. The gruelling working schedule amidst pandemic has predisposed them to witness psychological distress while providing direct care to the patients, being informed about the spike in cases or due to the mandatory requirements of isolation or quarantine.[4-6] Paradoxically, those treating and helping others are in the greatest need of psychological help something which is currently not available in full swing due to their continuous working hours and lack of self-care. Some even distance themselves emotionally alongside social isolation with the fear of either contracting or spreading this infection to their loved ones which, in turn, fuels anxiety, hypertension, stress, panic, uncertainty, apprehension, phobia, depression, insomnia etc. It is seen that during such periods of disturbances, ones coping styles, cognitive, affective, and behavioral expressions to the pandemic plays a major role in determining one’s emotional and psychological health.
Innumerable factors directly and indirectly affect the psychological health including the stigma the medical staff faces, social ostracism faced by some, juggling between personal and professional lives, overburdening of work, and experiencing burnout due to increased pressure, lack of safety equipment such as PPE and masks, and trauma of watching large number of patients dying alone in the isolation ward, among other factors. Notably, working exhaustively may not imply that these health-care staff is immune to psychological effects. They may have similar level of vicarious traumatization as that of general public.[7] The aforementioned is relatable to their increasing concerns for patients with disease, colleagues at risk, their families, and themselves.[7] The shortage of health-care facilities and no proven vaccine makes this situation even grimmer. The discovery of COVID-19 requires time and is even costly. Hence, healthcare workers are not getting tested due to cost incurred.[8] As of August 10, 2020, in India average of 18.36 COVID-19 tests are performed per 1 million population.[1]
Many healthcare workers have been infected and lost their lives due to coronavirus. Recently, Bacillus Calmette–Guérin (BCG) has been hypothesized as a potential protection from COVID-19. Cross-protection against COVID-19 by the BCG immunization has been speculated in India.[9] Coronavirus has the potential of instilling a sense of fear among other health-care professionals regarding their own lives. The current norm of social distancing also conflicts with their professional duty to treat others and also at the same time to maintain their own personal well-being.[10] Such kind of a cognitive dissonance can also lead to heightened levels of stress, worry, anxiety, depression, and reduced sleep, among other various issues that can take a toll on their psychological health. A 360 degree shift in the present lifestyle further fuels stress and anxiety thereby depleting the psychological resilience even lower than what currently it is. This psychological pandemic at the global level needs particular attention. We aimed to assess the presence of psychological distress, depression, anxiety, stress, and insomnia experienced by the healthcare workers in India related to COVID-19 pandemic.
MATERIAL AND METHODS
A multicentric cross-sectional study was conducted in India to evaluate the mental health of doctors working in COVID-19 wards from April 2020 to May 2020. Institute ethical committee approval was obtained for this study. A pre-designed, pre-tested validated semi-structured questionnaire was administered to the study subjects wherein objectives were explained, respectively. The questionnaires were prepared in the format of a Google document which was sent across through social media platforms such as WhatsApp, Facebook, and various social platforms where doctors are involved, e-mails, etc., to follow the restrictions and protocols of social distancing. Informed consent was taken from the respondents before the study and an option to terminate was made available anytime they desired in the form itself. Complete confidentiality of the respondents was ensured and no personal details were recorded for the purpose of the study such as name, address, and contact details. Participants doctors were targeted in this study. The target sample size of participants was determined using the formula N = Zα2P(1 − P) / d2, in which α = 0.05 and Zα = 1.96, and the estimated acceptable margin of error for proportion d was 10%. The proportion of doctors with psychological comorbidities was estimated at 24.3%, based on a previous study outbreak.[11] The calculated sample size is 707, adding 10% non-response rate the final sample size is 777.
Demographic details were reported by the participants, including age, gender (male, female, and other), present work area (government teaching/non-teaching hospital/institute, private teaching/non-teaching hospital/institute, private practice, and not working currently), primary specialty, any pre-existing conditions (hypertension, diabetes, asthma, etc.), and habits (smoking, alcohol consumption, etc.), if the participants were residing with children <3 years or with the elderly >65 years. Participants were also asked if they are exposed to COVID-19 patients/COVID-19 samples and their current postings in the COVID hospital.
Instruments
The online survey collected the information of the study variables of depression, stress, anxiety, and insomnia using the DASS-21 questionnaire and the Insomnia Severity Index (ISI). The DASS-21 scale is a self-report measure that is frequently used to assess the emotional states of depression, anxiety, and stress. Each of these three scales within DASS contains seven items. The scale of depression assesses feelings of hopelessness, loss of interest and pleasure, dysphoria, self-deprecation, etc. The anxiety scale measures autonomic arousal, subjective, situational aspects of anxiety, etc. The stress scale assesses aspects such as inability to relax, being easily upset or irritated, and being impatient or over reactive. It is a self-rated Likert scale with scores of 0 (did not apply to me at all) to 3 (mostly applied to me) in the past 1 week. The final score for the shorter version is multiplied by two to obtain the cumulative score.[12] The ISI consists of seven questions which are added together to get a final score. For each question specific Likert scale is provided ranging between scores 0 and 4. The appropriate score is to be selected based on severity of insomnia experienced in the past 2 weeks. The scores are interpreted according to the scoring guidelines ranging from 0 to 7 indicating no clinically significant insomnia to 22–28 indicating clinical insomnia (severe level).[13]
Statistical analysis
Statistical software used to analyze data were MS Excel, SPSS for Windows Inc. Version 22. Chicago, Illinois. Descriptive statistics were reported as median and interquartile range for continuous variables, frequencies (percentage) for categorical variables. Proportions were compared using Chi-square test. Continuous variables between the groups were measured using Mann–Whitney U-test and Kruskal–Wallis H test. Multiple logistic regressions were used to find the predictors of mental health outcome. Error bar plot and Box and Whisker plot were used to depict median scores. For all comparisons, P < 0.05 was considered statistically significant.
RESULTS
The study was conducted among 777 medical doctors. Out of which 538 doctors had exposure to COVID-19 patients. The mean age of the respondents (n = 538) was 32.07 ± 7.94 years. Out of 777 responding participants, we have got 538 participants directly working with COVID-19 patients. Maximum number of response rate individuals was seen in the age group of 20–30 years and 31–40 years. Around 54.7% of males are working in COVID-19 wards. Among our study participants, 8.7% use alcohol, 2.8% are smokers, and 5.4% are indulged in both. Around 71% of our study group is working in a tertiary care center while remaining 29% in a secondary care center. In our study, around 52% are working in a government set up and 48% in a private set up. Among the COVID-19 exposure participants in our study, 34% are professors working in a teaching institution, 42% working as residents, and 24% as medical officers, respectively.
Table 1 shows the association of ISI with demographic variables among our study participants. Severe and moderate insomnia were more commonly seen among females, those working at secondary care centers, working at private institutions, and among medical officers. All the factors were significantly associated with an increase in scores in ISI scale.
| Variable | No insomnia (n=320) | Sub-threshold (n=144) | Moderate insomnia (n=60) | Severe insomnia (n=14) | P-value |
|---|---|---|---|---|---|
| Gender | |||||
| Male | 192 (60) | 75 (52.1) | 21 (35) | 6 (42.9) | 0.02* |
| Female | 128 (40) | 69 (47.9) | 39 (65) | 8 (57.1) | |
| Place of working | |||||
| Tertiary | 250 (78.1) | 111 (77.1) | 16 (26.7) | 5 (35.7) | <0.001* |
| Secondary | 70 (21.9) | 33 (22.9) | 44 (73.3) | 9 (64.3) | |
| Currently working | |||||
| Government | 172 (53.75) | 82 (56.9) | 20 (33.33) | 6 (42.9) | 0.014* |
| Private | 148 (46.25) | 62 (43.1) | 40 (66.67) | 8 (57.1) | |
| Job title | |||||
| Professor | 120 (37.5) | 41 (28.5) | 18 (30) | 4 (28.6) | 0.001* |
| Residents | 138 (43.1) | 71 (49.3) | 12 (20) | 5 (35.7) | |
| Medical officers | 62 (19.4) | 32 (22.2) | 30 (50.0) | 5 (35.7) | |
Table 2 shows depression and anxiety to be significantly associated with COVID-19 exposed participants in our study. Moderate depression as a feature is present more commonly among females (60%) and was found to be statistically significant. Mild depression was seen more among those working at tertiary care centers (51.1%), while moderate depression was seen more commonly among those working at tertiary and secondary care centers and was found significant. Mild depression was seen more among those working at tertiary care centers (51.1%), while moderate depression was seen more commonly among those working at tertiary and secondary care centers and was found significant. Moderate depression was seen more commonly among medical officers (55%) and was found to be statistically significant. Severe anxiety is seen more among males (52.2%), whereas moderate anxiety more commonly seen among females (67.5%). In our study, 56.5% working at tertiary care hospitals subjected to COVID-19 were having severe anxiety. Medical officers and residents were more likely to have moderate and severe anxiety levels than others and were found to be statistically significant. Stress factor did not show any significant difference in our study.
| Variable | Depression | Anxiety | Stress (n=60) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Normal (n=471) | Mild (n=47) | Moderate (n=20) | P-value | Normal (n=395) | Mild (n=40) | Moderate (n=74) | Severe (n=23) | P-value | Normal (n=519) | Mild (n=10) | Moderate (n=9) | P-value | |
| Gender | |||||||||||||
| Male | 267 (56.7) | 19 (40.4) | 8 (40) | 0.04* | 239 (60.5) | 17 (42.5) | 24 (32.4) | 12 (52.2) | 0.001* | 287 (55.3) | 3 (30) | 4 (44.4) | 0.23 |
| Female | 204 (43.3) | 28 (59.6) | 12 (60) | 165 (39.5) | 23 (57.5) | 50 (67.5) | 11 (47.8) | 232 (44.7) | 7 (70) | 5 (55.6) | |||
| Place of working | |||||||||||||
| Tertiary | 348 (73.9) | 24 (51.1) | 10 (50) | 0.01* | 296 (74.9) | 27 (67.5) | 43 (58.1) | 13 (56.5) | 0.01* | 369 (71.1) | 7 (70) | 6 (66.7) | 0.95 |
| Secondary | 123 (26.1) | 23 (48.9) | 10 (50) | 99 (25.1) | 13 (32.5) | 31 (41.9) | 10 (43.5) | 150 (28.9) | 3 (30) | 3 (33.3) | |||
| Currently working | |||||||||||||
| Government | 241 (51.2) | 25 (53.2) | 14 (70) | 0.25 | 204 (51.6) | 19 (47.5) | 43 (58.1) | 10 (43.5) | 0.62 | 271 (52.2) | 3 (30) | 6 (66.7) | 0.25 |
| Private | 230 (48.8) | 22 (46.8) | 6 (30) | 191 (48.4) | 21 (52.5) | 31 (41.9) | 13 (56.5) | 248 (47.8) | 7 (70) | 3 (33.3) | |||
| Job title | |||||||||||||
| Professor | 165 (35) | 13 (27.7) | 5 (25) | 0.01* | 149 (37.7) | 11 (27.5) | 15 (20.3) | 7 (30.4) | 176 (33.9) | 4 (40) | 3 (33.3) | 0.54 | |
| Residents | 202 (42.9) | 20 (42.6) | 4 (20) | 168 (42.5) | 18 (45) | 32 (43.2) | 8 (34.8) | 0.001* | 221 (42.6) | 3 (30) | 2 (22.2) | ||
| Medical officers | 104 (22.1) | 14 (29.8) | 11 (55) | 78 (19.7) | 11 (27.5) | 27 (36.5) | 8 (34.8) | 122 (23.5) | 3 (30) | 4 (44.4) | |||
Table 3 shows the median and interquartile range of all the scores subjected to COVID-19 exposed participants. Depression, anxiety, and stress scores (DASS) were significantly higher among females, 5.0 (2.0–8.0) versus 6.0 (2.0–10.0) versus 3.0 (1.0–8.0); P < 0.001. Among those working at secondary care centers had a significantly higher DASS scores, 4.0 (2.0–8.0) versus 6.0 (2.0–10.0) versus 3.0 (0.0–8.0); P < 0.001. In our study, there was no significant difference in DASS with respect to working environment. Medical officers had a significantly higher DASS, 4.0 (2.0–8.5) versus 6.0 (2.0–11.0), 3.0 (0.5–9.0);P < 0.001. Similarly, ISI scores were significantly higher among females, 7.0 (2.0– 12.0); those working at secondary care centers, 8.0 (3.0–16.0) and among medical officers 8.0 (3.0–15.0).
| Variable | Depression | P-value | Anxiety | P-value | Stress | P-value | Insomnia | P-value |
|---|---|---|---|---|---|---|---|---|
| Total median (IQR) | 4.0 (2.0–7.0) | 4.0 (1.0–8.0) | 2.0 (0.0–6.0) | 6.0 (2.0–10.0) | ||||
| Gender | ||||||||
| Male | 3.0 (1.0–5.0) | <0.001* | 3.0 (1.0–7.0) | <0.001* | 2.0 (0.0–4.0) | <0.001* | 5.0 (1.0–9.0) | 0.002* |
| Female | 5.0 (2.0–8.0) | 6.0 (2.0–10.0) | 3.0 (1.0–8.0) | 7.0 (2.0–12.0) | ||||
| Place of working | ||||||||
| Tertiary | 3.0 (2.0–6.0) | 0.001* | 4.0 (1.0–7.0) | <0.001* | 2.0 (0.0–5.0) | 0.04* | 5.0 (2.0–9.0) | <0.001* |
| Secondary | 4.0 (2.0–8.0) | 6.0 (2.0–10.0) | 3.0 (0.0–8.0) | 8.0 (3.0–16.0) | ||||
| Currently working | ||||||||
| Government | 4.0 (2.0–7.0) | 0.22 | 4.0 (1.0–8.0) | 0.69 | 2.0 (0.0–6.0) | 0.55 | 6.0 (2.0–9.0) | 0.31 |
| Private | 3.0 (2.0–7.0) | 4.0 (1.0–8.0) | 3.0 (0.0–5.0) | 6.0 (2.0–11.0) | ||||
| Job title | ||||||||
| Professor | 3.0 (1.0–6.0) | 0.005* | 3.0 (1.0–7.0) | <0.001* | 2.0 (0.0–5.0) | 5.0 (1.0–9.0) | <0.001* | |
| Residents | 3.0 (2.0–7.0) | 4.0 (1.0–8.0) | 2.0 (0.0–5.0) | 0.01* | 6.0 (2.0–9.0) | |||
| Medical officers | 4.0 (2.0–8.5) | 6.0 (2.0–11.0) | 3.0 (0.5–9.0) | 8.0 (3.0–15.0) | ||||
Graph 1 shows the median and interquartile range of all the scores. In our study, overall median depression scores were 4.0 (2.0–7.0); anxiety scores were 4.0 (1.0–8.0), stress scores were 2.0 (0.0–6.0), and insomnia scores were 6.0 (2.0–10.0). Graph 2 shows error bar plot featuring the DASS score over ISI. Severe clinical insomnia scores were associated with higher DASS.
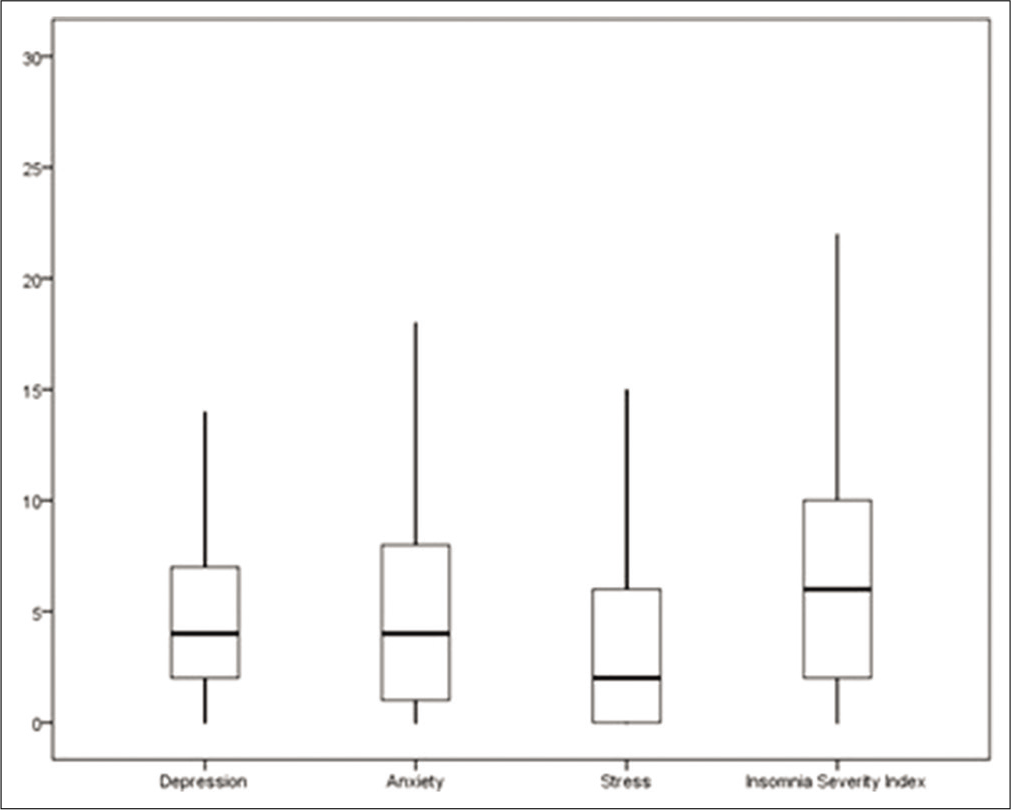
- Box and whisker plot showing scores of depression, anxiety, stress and insomnia index (n=538)
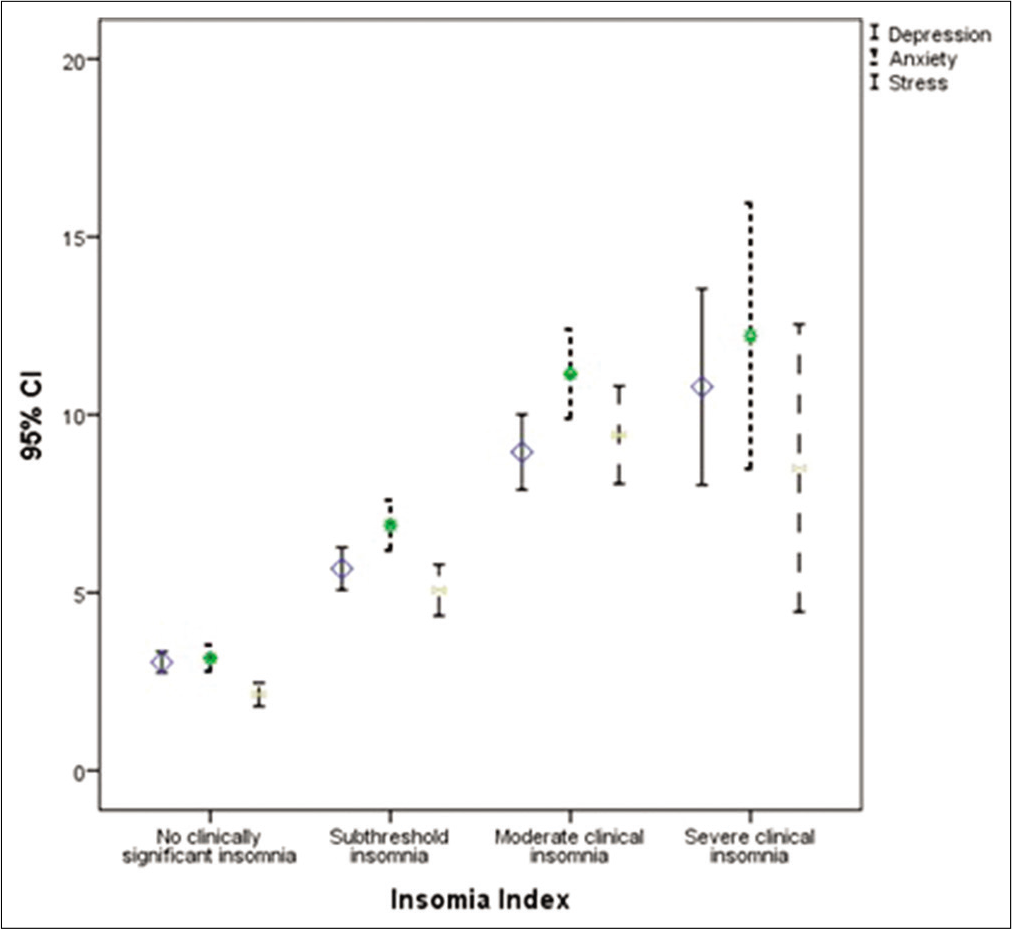
- Error bar plot featuring the DASS score over Insomnia index severity (n=538)
DISCUSSION
The results of our study revealed a 40.4% and 40% prevalence of mild and moderate depression, respectively, among male doctors and 59.6% and 60% of mild and moderate depression, respectively, among female doctors during COVID-19 pandemic. Around 55% of medical officers in the study reported having moderate levels of depression. A study conducted in Korea among 64 doctors indicated a depression rate of nearly 27% during the Middle East Respiratory Syndrome outbreak.[14] In our study, with respect to anxiety it was found that among men as many as 52% reported experiencing severe anxiety and 24% had moderate levels of anxiety whereas females reported as high as 68% and 48% of moderate and severe anxiety, respectively. This indicates an alarmingly high number of healthcare workers experiencing mental overload during this time of uncertainty reiterating the fact that the frontline workers are indeed the worst hit by the pandemic. Anxiety rates were higher especially among the resident doctors and the medical officers [Table 3]. A study on the mental health of general public was conducted in China which reported moderate to severe levels of depression, stress, and anxiety (16.5%, 8.1%, and 28.8%, respectively) among the respondents. Such increased rates of reported problems even in general public in turn indicates how the frontliners are at even greater risk to experience mental health problems during this crucial time.[15,16]
Outbreak of COVID-19 has led to a sudden shift in the workforce behavior around the globe posing immense burden on the health-care system. In our study, around 30% and 44% male doctors reported mild and moderate level of stress, respectively, whereas 70% and 56% female doctors reported mild and moderate level of stress, respectively, again indicating an increase in the stress levels being experienced by the health-care staff during this time. Stress rates were especially high among professors and medical officers [Table 3]. A study conducted in China to assess the psychological impact of COVID-19 on medical workforce reported the participants (n = 2299) to be twice at risk of depression, fear, and anxiety by working in close contact with the infected patients.[17] It was observed in our study that among female doctors the rates of moderate insomnia were especially high (65%), whereas high level of male participants reported sub threshold insomnia (52%). As many as, 57% females reported severe insomnia. With the increase in working hours, shortage of manpower and acute burden on healthcare infrastructure, it is bound to have a downward spiral effect on those who are tirelessly battling with this ever increasing problem. The residents and the medical officers are worst hit by this issue [Table 2].
Early reports of COVID-19 and from the previous outbreak of severe acute respiratory syndrome (SARS, 2003) depict that the healthcare workers are highly prone to experiencing stress, fear, depression, insomnia, and anxiety.[6] This is true for the workers directly engaged in diagnosing, treating, and providing care to suspected or confirmed cases of COVID-19. Another similar observational study involving 180 medical staff dealing directly with COVID-19 patients showed substantial effect of stress and anxiety on the sleep quality and levels of self-efficacy. Indeed, escalation in social support acts as a buffer against stress and anxiety by lowering its level.[18] No Indian studies have been conducted in the area of COVID-19 like the present study by studying all these variables in conjunction. It is agonizing to report that an increasing number of suicides have been reported worldwide especially among the general public. Similar instance was reported in India on February 12, 2020 at first.[19] Recent findings add to the reporting of two more similar suicidal cases in India and brings out the turmoil of this avalanching pandemic condition.[20] These incidences have been increasing among the healthcare workers as well all over the world due to the increasing demand and reliance on the medical professionals with an added burden where they have the responsibility to take decision of someone else’s life. There is an increased risk of experiencing cumulative trauma or vicarious trauma when working with huge number of patients daily during such a crisis.[7]
The COVID-19 mental health concerns can be classified in acute phase (approximately 2–6 months after the outbreak) which includes immediate psychological issues such as anxiety, fear dissociative symptoms, substance withdrawal, and denial and long-term phase (after the control of the outbreak, >6 months) which includes depression, grief, and relapse of pre-existing mental health issues.[21] Therefore, consistent commitment is needed by the mental health professionals even after the pandemic is over. Our study shows that participants treating COVID-19 patients had increased risk of insomnia, with severe and moderate insomnia more commonly seen in females. Furthermore, statistically significant moderate depression was present commonly among females (60%). Severe anxiety was common in males (52.2%) and moderate anxiety was commonly seen in females (67.5%). A similar online survey in China concluded that medical healthcare workers were more prone to developing insomnia, anxiety, depression, obsessive-compulsive, and traumatization disorders as compared to their non-medical counterparts.[11]
Taking into consideration the mammoth impact of this pandemic, it is essential that mental healthcare should be the primary focus along with the medical care provided. Telecounselling and psychotherapy are the need of the hour. In a time that warrants social distancing to be maintained, it is essential to equip the frontliners with how to do meditation, breathing and other relaxation techniques such as the Jacobson Progressive Muscle Relaxation. Supportive psychotherapy, mindfulness techniques, psychoeducation, activity scheduling, grief counseling, and sleep hygiene are some of the ways that can ensure the mental sanity of the healthcare workers during this overwhelming time. A team of trained personnel’s should be made available for quick assessment of the psychological issues and its remediation. The daunting impact of the pandemic can also be contained by the process of debriefing and catharsis promoted by team members especially during unfortunate outcomes such as increased death count. The existing health-care system should be boosted in the coming times to push forward the psychological care of everyone for a better and more robust future. The information obtained from self-reported questionnaires was not verified with responder’s medical records. Furthermore, currently, India is in the midst of the pandemic and the delayed psychological outcomes related to COVID-19 are difficult to capture with the current survey. Hence, this may limit the generalizability of the findings.
CONCLUSION
The impact that this pandemic is casting over the mental health of the healthcare workers should not be overlooked today and even in the coming times when the crisis is over. It is suggestive of high need for psychological support and interventions for maintaining a robust clinical workforce. Early screening targeting the medical workforce and implementation of psychological interventions are essential for protecting and maintaining the functionality of the health-care system.
Acknowledgments
We thank Dr. Shivam Mahajan, Resident, North Delhi Medical College & Hindu Rao Hospital, Delhi, India, for literature search regarding COVID-19. We also thank all the participants for their valuable inputs and feedback in our study. All the authors have equally contributed in framing and reviewing the manuscript.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Government of India. Available from: https://www.mygov.in/covid-19 [Last accessed on 2020 Aug 14]
- [Google Scholar]
- Available from: http://www.covid19-sdmc.org [Last accessed on 2020 Aug 14]
- Coronavirus: Hotspot on coronavirus disease 2019 in India. Indian J Med Sci. 2020;72:29.
- [CrossRef] [Google Scholar]
- Impact on health care workers employed in high-risk areas during the Toronto SARS outbreak. J Psychosom Res. 2008;64:177-83.
- [CrossRef] [PubMed] [Google Scholar]
- The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet. 2020;395:912-20.
- [CrossRef] [Google Scholar]
- Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3:e203976.
- [CrossRef] [PubMed] [Google Scholar]
- Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav Immun. 2020;88:916-9.
- [CrossRef] [PubMed] [Google Scholar]
- Role of nasopharyngeal lactate dehydrogenase as a possible economical mass screening test for the detection and segregation of SARS-CoV-2 (COVID-19) cases in India. Indian J Med Sci. 2020;72:21.
- [CrossRef] [Google Scholar]
- Does the Bacillus Calmette-Guérin vaccine provide protection from COVID-19? Indian J Med Sci. 2020;72:17.
- [CrossRef] [Google Scholar]
- The impact of severe acute respiratory syndrome on medical house staff: A qualitative study. J Gen Intern Med. 2005;20:381-5.
- [CrossRef] [PubMed] [Google Scholar]
- Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom. 2020;89:242-50.
- [CrossRef] [PubMed] [Google Scholar]
- The structure of negative emotional states: Comparison of the depression anxiety stress scales (DASS) with the beck depression and anxiety inventories. Behav Res Ther. 1995;33:335-43.
- [CrossRef] [Google Scholar]
- The insomnia severity index: Psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34:601-8.
- [CrossRef] [PubMed] [Google Scholar]
- Psychological effects on medical doctors from the Middle East respiratory syndrome (MERS) outbreak: A comparison of whether they worked at the MERS occurred hospital or not, and whether they participated in MERS diagnosis and treatment. J Korean Neuropsychiatr Assoc. 2017;56:28.
- [CrossRef] [Google Scholar]
- Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17:1729.
- [CrossRef] [PubMed] [Google Scholar]
- Protecting health-care professionals and workers (other than COVID-19 management facilities) from contamination during COVID-19 pandemic (March 26, 2020-India) Indian J Med Sci. 2020;72:3.
- [CrossRef] [Google Scholar]
- Psychological status of medical workforce during the COVID-19 pandemic: A cross-sectional study. Psychiatry Res. 2020;288:112936.
- [CrossRef] [PubMed] [Google Scholar]
- The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monit. 2020;26:e923549.
- [CrossRef] [Google Scholar]
- Fear of COVID 2019: First suicidal case in India. Asia J Psychiatry. 2020;49:101989.
- [CrossRef] [PubMed] [Google Scholar]
- Self-harm and COVID19 pandemic: An emerging concern-a report of 2 cases from India. Asia J Psychiatry. 2020;51:102104.
- [CrossRef] [PubMed] [Google Scholar]
- Mental Health in the Times of COVID-19 Pandemic-guidance for General Medical and Specialised Mental Health Care Settings In: Department of Psychiatry. Karnataka: NIMHANS; 2020.
- [Google Scholar]






