Translate this page into:
Recurrent aggressive multicystic ameloblastoma with hemangiomatous proliferation and giant cells: A perplexed diagnosis

*Corresponding author: Dr. S. Mishra, Department of Oral and Maxillofacial Surgery, Institute of Dental Sciences, Siksha ‘O’ Anusandhan, Deemed to be University, Bhubaneswar, Odisha, India. sobhan.surgeon@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Routray S, Mishra S, Mohanty N, Panda S, Panda P. Recurrent aggressive multicystic ameloblastoma with hemangiomatous proliferation and giant cells: A perplexed diagnosis. Indian J Med Sci 2019;71(2):93-6.
Abstract
Hemangiomatous ameloblastoma, a very rare variant of ameloblastoma, was originally described as ameloblastoma in which part of the tumor contained spaces filled with blood or large endothelial-lined capillaries. Ameloblastoma, the most commonly affecting a slow-growing, persistent, and locally aggressive neoplasm of epithelial origin, account for a major chunk of all odontogenic tumors. A 43-year-old female reported to our outpatient department with a rare association of multicystic ameloblastoma with unusual hemangiomatous proliferation (both in lining and the stroma) along with giant cells in the lesional tissue. There are <8 cases documented in the literature with the same histologic features and most are in the middle age with the mandibular location.
Keywords
Ameloblastoma
Hemangiomatous
Multicystic
Odontogenic tumors
INTRODUCTION
Ameloblastoma, a slow-growing, persistent, and locally aggressive neoplasm of epithelial origin, accounts for a major chunk of all odontogenic tumors. According to the 2005 World Health Organization classification, ameloblastomas are classified into the following types: (1) Solid/multicystic, (2) extra-osseous/peripheral, (3) desmoplastic, and (4) unicystic. The follicular and plexiform patterns are the main histologic subtypes of the solid/multicystic variant.[1] The follicular type can be further subdivided into a spindle cell, an acanthomatous, a granular type, and a basal cell type. Other less commonly encountered histologic patterns include desmoplastic, basal cell, clear cell, keratoameloblastoma, papilliferous keratoameloblastoma, and unicystic ameloblastoma (UA).[2] UA, first described by Robinson and Martinez in 1977, refers to those cystic lesions that show clinical, radiographic, or gross features of a mandibular cyst, but on histologic examination shows a typical ameloblastomatous epithelium lining part of the cyst cavity, with or without luminal, and/or mural tumor growth.[3] Three histopathological variants are recognized, being the luminal, intraluminal, and the mural variant. Although with the exception of desmoplastic and unicystic type, histopathological variants do not carry significance in terms of prognosis and biological behavior.[4] Hemangiomatous ameloblastoma (HA), a very rare variant of ameloblastoma, was originally described as an ameloblastoma in which part of the tumor contained spaces filled with blood or large endothelial-lined capillaries.[5] Lesions with similar histologic features were earlier documented as ameloblastic hemangiomas, adamantinohemangiomas, and hemangio ameloblastomas. It was Kuhn in 1932, who described the first case of vascular ameloblastoma, a combination of adamantinoma and hemangioma; followed by Oesterreich and Aisenberg as adamantinohemangiomas. It was also documented in the early literature as ameloblastic hemangiomas and hemangio ameloblastomas.[5,6] There are <8 cases documented in literature with same histologic features and most are in the middle age with mandibular location.[7] We here describe a rare association of multicystic ameloblastoma with unusual hemangiomatous proliferation (both in lining and the stroma) along with giant cells in the lesional tissue.
CLINICAL HISTORY
A 43-year-old female with a history of swelling and surgery for ameloblastoma in the same region 10 years back reported to our outpatient department with a recurrent painful swelling in the right mandible with a 3-month history. A panoramic radiograph showed a huge multilocular radiolucency on the right mandible ramus extending from right body of the mandible till coronoid process [Figure 1a]. Lingual cortical bone perforation was also evident. She underwent excision of the tumor and partial resection of the left mandible. The resected mandibular specimen [Figure 1b and c] on radiographic evaluation showed gross destruction of bony tissue along the body of mandible and a destroyed coronoid and condylar process too [Figure 1d and e].
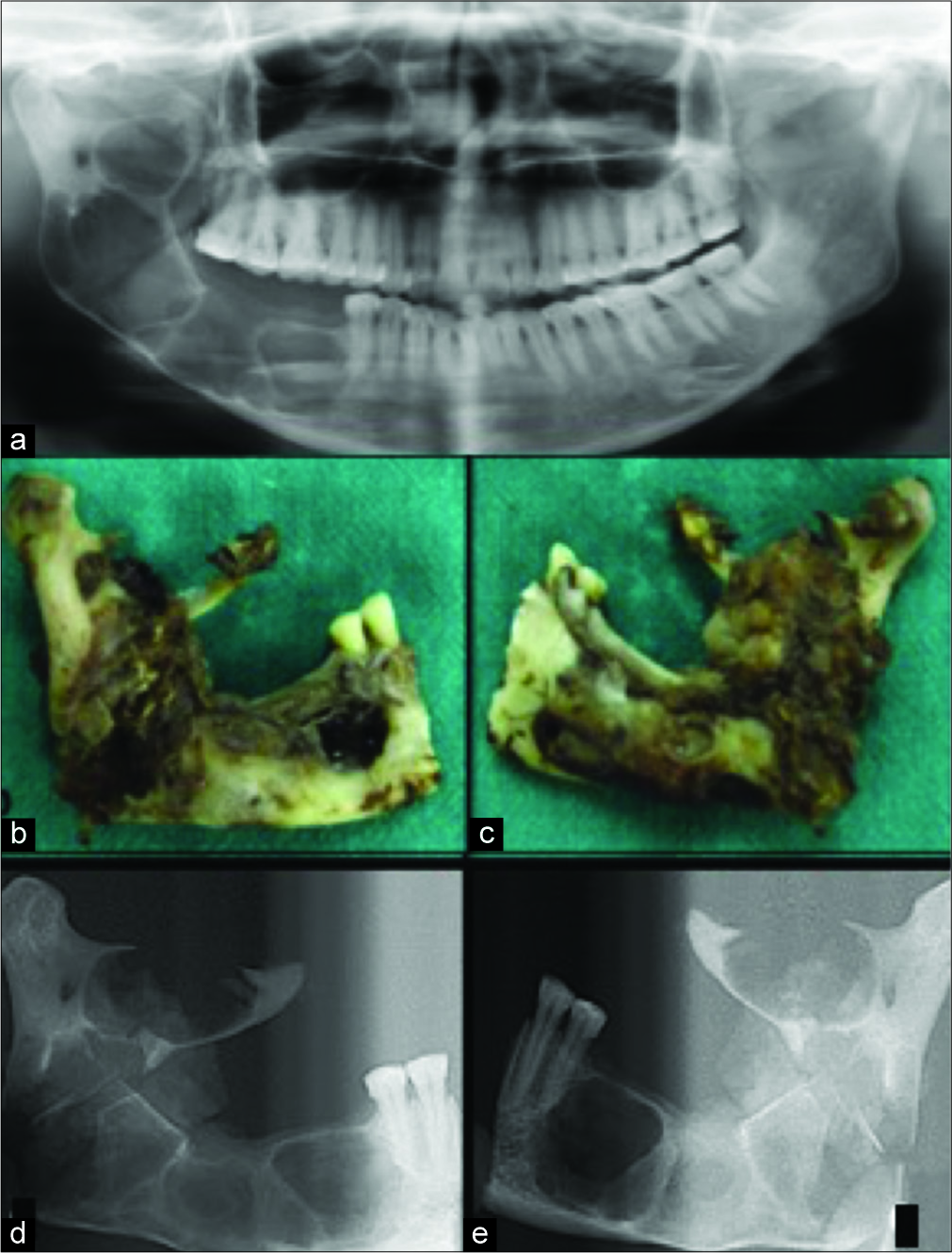
- (a) A panoramic radiograph showed a huge multilocular radiolucency on the right mandible ramus extending from right body of the mandible till coronoid process (b and d) the resected mandibular specimen with both anterior and posterior views. (c and e) Radiographs of both anterior and posterior views of specimen showed gross destruction of bony tissue along the body of mandible and a destroyed coronoid and condylar process.
Microscopically, the ameloblastic epithelium was seen to be proliferative with sprouting of blood vessels as a distinct feature [Figure 2a and b]. An area in stroma of the lesional tissue showed accumulation of multiple multinucleated giant cells (MGCs) [Figure 2d and e]. The stroma showed numerous blood vessels and chronic inflammatory cells [Figure 2g]. The epithelial lining with a basal cell layer composed of columnar cells displaying hyperchromatic, palisaded nuclei with reverse polarity of the nuclei appreciated [Figure 2h] confirmed the diagnosis of ameloblastoma, though mimicking unicystic variant (UA) with hemangiomatous propagations. To understand the nature of these aggressive varieties with hemangiomatous proliferations and comprehend the origin of MGCs, immunohistochemistry (IHC) was done. The lesional tissue showed strong positivity for matrix metalloproteinase 9 (MMP-9), the giant cells were positive for tartrate-resistant acid phosphatase (TRAP) and focally positive for calcitonin [Figure 2c, f and i].

- (a and b) Microscopically, the ameloblastic epithelium was seen to be proliferative with sprouting of blood vessels as a distinct feature (low- and high-power magnification) (c) the lesional tissue showing strong positivity for matrix metalloproteinase 9 (d and e) an area in the lesional tissue showed accumulation of multiple multinucleated giant cells (high- and low-power magnification). (f) The giant cells were positive for tartrate-resistant acid phosphatase (g) cystic epithelial lining with a basal cell layer composed of columnar cells displaying hyperchromatic, palisaded nuclei with reverse polarity of the nuclei. (h) The stroma showed numerous blood vessels and chronic inflammatory cells. (i) The lesional tissue showed focally positive for calcitonin but negative for the unicystic lining.
DISCUSSION
It is generally accepted that the ameloblastoma of follicular type cystic variant with histological features as in our case being multilocular, has a benign course and represents a distinct entity that occurs during the first two decades of life, whose diagnosis is entirely based on the histological picture. The histomorphologic patterns do have a significant bearing on the biologic behavior or prognosis of these tumors.[8-10] Although Lucas and Smith have described vascular and controversial ameloblastoma way back, still the concept is still delusional.[11,12] In our reported case the unusual histologic pattern of UA in a multilocular lesion, showing hemangiomatous proliferation has made us diagnose it as HA. The vascular component of the HA has not yet been conducible to a neoplastic process, or a hamartomatous malformation or representing a collision tumor. It might be a disturbance in the repair of neoplastic odontogenic tissue resulting in excessive granulation tissue formation or the development of an abnormal vascular component. According to Smith, HA was similar to one of the other recognized types of ameloblastoma and not as a distinct histologic entity. However, a recent concept by Sarode et al. emphasized on features such as vascular malformation and neoangiogenesis/ aberrant angiogenesis and a very aggressive course which did not support the diagnosis of UA making it more relative to be designated either as a unique variant of UA with multifoci or a different entity like HA.[13] The clinical course of multicystic hemangio ameloblastoma (MHA) and the aggressive nature found in other case reports, then nature of blood vessels in MHA should be studied thoroughly to be more precise in designating a terminology for HA.
Taking the above queries into consideration, in our case of recurrent lesion after 10 years showing a very aggressive behavior and the presence of MGCs in the stroma, we advised for IHC. IHC showed strong positivity for MMP-9 corroborating to the aggressiveness. Literature has confirmed the role of MGCs contributing to inflammatory tissue damage leading to granuloma formation thereby releasing MMP-9.[14] MMP-9 expression in osteolytic lesions of bone correlates well with the extent of bone destruction and local recurrence and their expression maybe related to prognostic indication of the possible aggressive behavior of the underlying pathology. The origin of giant cells in the presented case could not be ascertained for which IHC of tissue using calcitonin and TRAP was also done. TRAP which is associated with osteoblast migration and plays a major role in initiating osteoblastic differentiation, activation, and proliferation, was found strongly positive confirming these MGCs to be osteoclasts.[15] However, the best marker for osteoclast is the calcitonin receptor, though was diffusely positive in our case in the stroma.[16,17] Considering the aggressive clinical course of the presented case we concluded the osteoclastic nature of giant cell to be the reason behind.
CONCLUSION
We presented a case with recurrent multicystic ameloblastoma, aggressive in nature with hemangioblastomatosis proliferations in the cystic lining, authenticating to the nutrition for the tumor to recur and the destructive physiology attributable to the giant cells in the stroma. Collectively, all these features are rarely seen or have been reported and so making it a unique diagnosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- World Health Organization Classification of Tumors, Pathology and Genetics. Head and neck tumors. Lyon: IARC Press; 2005.
- Odontogenic Tumors and Allied Lesions. London: Quintessence Publishing Co., Ltd.; 2004.
- Diagnostic criteria for unicystic ameloblastoma: Ameloblastic versus ameloblastomatous epithelium. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:536.
- [CrossRef] [PubMed] [Google Scholar]
- Odontogenic tumours: A Rationale for Diagnosis and Treatment. Surrey: Quintessence Publishing Co., Inc.; 2003. p. :635-53.
- Hemangiomatous ameloblastoma: Clinical, radiologic, and pathologic features. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91:374-80.
- [CrossRef] [PubMed] [Google Scholar]
- Hemangiomatous Ameloblastoma: A case report of a rare variant of ameloblastoma. Int J Contemp Dent. 2010;2:16-9.
- [Google Scholar]
- Hemangiomatous ameloblastoma in maxilla: A report of a very rare case. Dent Res J (Isfahan). 2012;9:345-9.
- [Google Scholar]
- The desmo-and osteoplastic ameloblastoma. Histologic variant or clinicopathologic entity? Case reports. Int J Oral Maxillofac Surg. 1992;21:352-7.
- [CrossRef] [Google Scholar]
- Clear cell ameloblastoma--an odontogenic carcinoma. J Oral Maxillofac Surg. 1985;43:707-17.
- [CrossRef] [Google Scholar]
- Unicystic ameloblastoma: A prognostically distinct entity. Cancer. 1977;40:2278-85.
- [CrossRef] [Google Scholar]
- A vascular ameloblastoma. Oral Surg Oral Med Oral Pathol. 1957;10:863-8.
- [CrossRef] [Google Scholar]
- The controversial ameloblastoma. Oral Surg Oral Med Oral Pathol. 1968;26:45-75.
- [CrossRef] [Google Scholar]
- Intraluminal plexiform hemangioameloblastomatous proliferation in unicystic ameloblastoma: An unusual case report. Indian J Dent Res. 2013;24:390-2.
- [CrossRef] [PubMed] [Google Scholar]
- Expression of VEGF and MMP-9 in giant cell tumor of bone and other osteolytic lesions. Life Sci. 2003;73:1427-36.
- [CrossRef] [Google Scholar]
- Tartrate-resistant acid phosphatase (TRAP) and the osteoclast/immune cell dichotomy. Autoimmunity. 2008;41:218-23.
- [CrossRef] [PubMed] [Google Scholar]
- Immunohistochemical expression of RANK, GRalpha and CTR in central giant cell granuloma of the jaws. Oral Oncol. 2005;41:480-8.
- [CrossRef] [PubMed] [Google Scholar]
- Immunohistochemical expression of glucocorticoid and calcitonin receptors as a tool for selecting therapeutic approach in central giant cell granuloma of the jawbones. Int J Oral Maxillofac Surg. 2006;35:756-60.
- [CrossRef] [PubMed] [Google Scholar]






