Translate this page into:
Spectrum of hepatic encephalopathy admitted in a tertiary care center

*Corresponding author: Amit Soni, Department of Gastroenterology, MMIMSR, Maharishi Markandeshwar (Deemed to be) University, Ambala, Haryana, India. aamitsoni@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Soni A, Nagpal S, Mittal A. Spectrum of hepatic encephalopathy admitted in a tertiary care center. Indian J Med Sci, doi: 10.25259/IJMS_55_2020
Abstract
Objectives:
Few of the common symptoms for which cirrhotic patient seeks medical care are gastrointestinal bleed, abdominal distension (ascites), altered sensorium (hepatic encephalopathy [HE]), etc. This study was done to look at the spectrum of HE among cirrhotic patients admitted in a tertiary care center.
Material and Methods:
This hospital-based study was carried on 36 HE patients (with liver cirrhosis and age >18 years) admitted in the department of gastroenterology of a tertiary care center, between April 2019 and November 2019.
Results:
Constipation and infections were the two most frequent precipitating factors identified. Majority patients (77.8%) belonged to CTP Class C. In-hospital mortality was observed in seven patients. The OR was significant for infections and in-hospital mortality (OR – 28.80 and P < 0.05). A moderate positive correlation (Pearson’s correlation, r = 0.335) was seen between MELD score and in-hospital mortality among HE patients.
Conclusion:
A larger mass of HE patients belongs to CTP Class C. Constipation and infections are the two most common precipitating factors for HE. All HE patients who have concomitant infection and/or high MELD score should be managed on priority basis.
Keywords
Hepatic encephalopathy
Cirrhosis
MELD
INTRODUCTION
The burden of liver cirrhosis is soaring worldwide. With liver cirrhosis, the morbidity and mortality of the patient escalates. There are close to 10.6 million cases (2017) of decompensated cirrhosis globally.[1] It is estimated that with the given population burden, India accounts for approximately 18.3% of all cirrhosis deaths globally.[2] This figure is big and it can also be attributed to the poor availability of health services in rural areas and dearth of universal health insurance. According to studies, patients with liver cirrhosis do not pursue hospital treatment when in compensated state. It is only when the patient becomes decompensated, they seek medical attention for varied signs and symptoms.[1] Few of the common signs and symptoms for which patient seeks advice are gastrointestinal (GI) bleed, abdominal distension (ascites), altered sensorium (hepatic encephalopathy [HE]), etc. HE is a reversible syndrome of impaired brain function occurring in patients with advanced liver failure.[3]
The pathogenesis of HE is multifactorial. Various factors implicated in pathogenesis include the role of neurotoxins (ammonia), impaired neurotransmission due to metabolic changes in liver failure, altered brain energy metabolism, changes in blood– brain barrier, and systemic inflammatory response.[3] Various precipitating factors have been described for HE such as GI bleed, electrolyte imbalances, constipation, infections, etc.[3] Timely diagnosis of precipitating factor and rectifying it is very important. A large majority of patients can be treated by merely amending the precipitating factor. Focusing on various precipitating factors is also important as prevention of such precipitating factors can reduce the future incidence of HE and hence morbidity/mortality in a patient with liver cirrhosis. Treatment strategy also includes use of lactulose and rifaximin.[4] Multitudinal studies have been done to show efficacy of single lactulose therapy or combining lactulose with rifaximin.[4] L-ornithine-L-aspartate has also been used in the treatment of HE; however, this medicine is not FDA approved.[5,6] One of an American studies estimated the overall incidence of HE to be 11.6 per 100 patient-years.[7] This study was done to look at the spectrum of HE among cirrhotic patients admitted in a tertiary care center.
MATERIAL AND METHODS
This hospital-based observational study was carried on HE patients (with liver cirrhosis and age >18 years) admitted in the department of gastroenterology of a tertiary care center, between April 2019 and November 2019. Patients with any other cause of altered sensorium or history of any neurological disorder were excluded from the study. Details of the patient including history, clinical examination findings, and results of laboratory investigations were collected. CTP (Child-Pugh) score and MELD (Model for End-Stage Liver disease) score of patients were also noted. Diagnosis and classification of HE was considered as per the West Haven criteria.[8] The study protocol conformed to the ethical guidelines and was approved by the institutional review board.
Results for continuous variables were expressed as means and standard deviation. Variables with non-normal distribution were described by a median. Categorical variables were expressed as percentages. Significant factors associated with the presence of HE were analyzed using binary logistic regression analysis. Bivariate analysis was carried out using Pearson’s coefficient of correlation. Odds ratio (OR) was used to ascertain the strength of relationship between two variables. P < 0.05 was considered statistically significant. SPSS21 software was used for statistical analysis.
RESULTS
The mean age among study group was found to be 51.83 years (SD 12.83). A total of 32 patients (88.9%) included in the study were male, while rest 4 (11.1%) patients were female. The most prevalent etiology of liver cirrhosis among the patient group was alcohol, aggregating for 77.8% of the etiology. Various etiologies of liver cirrhosis are depicted in Table 1. Ten patients had more than 1 etiology (alcohol with hepatitis C and alcohol with non-alcoholic steatohepatitis [NASH] were the most common seen in three patients each). Various precipitating factors for HE are depicted in Table 2.
| Etiological factor for cirrhosis** | n(%) |
|---|---|
| Alcohol | 28 (77.8) |
| HBV related | 7 (19.4) |
| HCV related | 4 (11.1) |
| NASH related | 7 (19.4) |
| Precipitating factors for HE* | n(%) |
|---|---|
| Constipation | 14 (38.8) |
| GI bleed | 7 (19.4) |
| Electrolyte imbalances | 9 (25) |
| Infections | 11 (30.5) |
| Drug misuse/overdosage | 4 (11.1) |
Five patients were in Grade I HE, while 10, 14, and 7 patients belonged to Grades II, III, and IV HE, respectively [Figure 1]. Various other complications of liver cirrhosis were also looked for in patients with HE. Ascites (88.9%) was the most common complication seen among liver cirrhosis patients with HE, while renal failure, infections, and SBP were seen in 55.6%, 30.6%, and 16.7%, respectively. Each and every patient had decompensated liver cirrhosis. Eight (22.2%) patients belonged to CTP Class B while the rest 28 (77.8%) patients were the part of Class C. The median value for MELD score was 23. In-hospital mortality was observed in seven patients. Follow-up of discharged patients was not available. The OR was calculated for various parameters and in-hospital mortality among HE patients [Table 3]. The OR was significant for infections and in-hospital mortality with the OR value of 28.80 (2.81–294.82) and P < 0.05.
| In-hospital mortality | No mortality | Odds ratio (95% C.I.) | P-value | |
|---|---|---|---|---|
| Renal failure | ||||
| Present | 7 | 13 | 18.33 (0.95–350.88) | 0.053 |
| Absent | 0 | 16 | ||
| Ascites | ||||
| Present | 7 | 25 | 2.64 (0.12–54.95) | 0.52 |
| Absent | 0 | 4 | ||
| SBP | ||||
| Present | 3 | 3 | 6.50 (0.95–44.13) | 0.055 |
| Absent | 4 | 26 | ||
| Infections | ||||
| Present | 6 | 5 | 28.80 (2.81–294.82) | 0.004 |
| Absent | 1 | 24 |
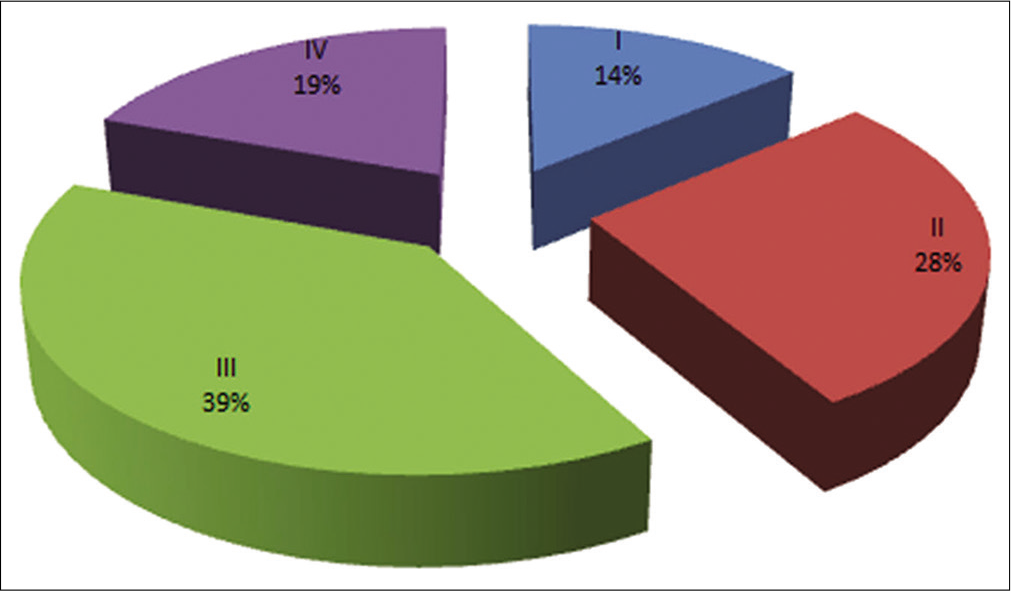
- Percentage of patients in various grades of hepatic encephalopathy.
A moderate positive correlation (Pearson’s correlation, r = 0.335) was seen between MELD score and in-hospital mortality among HE patients. This positive correlation was significant at P < 0.05 level. The correlation calculated was not significant for CTP score and grades of HE when correlated with in-hospital mortality.
DISCUSSION
Our study depicted the spectrum of HE among liver cirrhosis patients, including various precipitating factors, associated signs/symptoms, and in-hospital mortality. In a study by Jhajharia et al., the mean age of liver cirrhosis patients was 45.6 years. Furthermore, in the same study, men dominated with a male-to-female ratio of 5.5:1.[9] A study from Puducherry, wherein HE patients were observed, male (92.23%) patients predominated and the mean age of the study group was 49.58 years.[10] These data match with our study results, indicating male preponderance among cirrhotic patients.
In a multicenter Indian study, a substantial regional variation in the etiology of liver disease across the country was found. However, alcohol (34.3%) emerged as the most common etiology of liver cirrhosis.[11] In a study from Sweden, alcohol was most common and constituted 50.5% of all etiologies of liver cirrhosis.[12] Alcohol-related liver cirrhosis predominated in our study also. Multiple studies have given a similar alcohol predominant etiology for liver cirrhosis. In one Indian study, it was concluded that alcohol-related diseases contribute up to one-fifth of in hospital admissions in the gastroenterology department.[13] It can be predicted that alcohol-related liver disease and other alcohol-related diseases are being added to a gigantic extent for in hospital gastroenterology admissions. Globally, NASH-related liver cirrhosis is on the surge. In GBD 2017, NASH was included as the fifth cause of cirrhosis for the 1st time.[1] Although few of previous studies from India do not recognize NASH as an etiological factor, it was well identified in our survey.[9]
In our research, constipation and infections were the two frequent precipitating factors identified while drug overdosage/misuse comprised the least. In a study by Devrajani et al., the most common precipitating factors detected were infections and constipation. In this study, majority of the patients belongs to CTP Class C.[14] Panchili and Thomas investigated and found constipation, spontaneous bacterial peritonitis, and urinary tract infection as the most rampant precipitating factor for HE. They also summarized that patients who have multiple precipitating factors for encephalopathy have delayed recovery and high mortality.[15] In a scrutiny by Dhande et al., upper GI bleed was the most common precipitating factor for HE followed by constipation.[16] Author also established that 18.4% of patients had multiple precipitating factors for HE.[16] In a study from Nigeria, the common precipitating factor identified for HE were sepsis 29% and GI bleed 24%.[17] Furthermore, in the aforementioned study, the author identified that 61% of their patients belong to CTP Class C. Various predictors of mortality identified by the author included a history of significant alcohol ingestion, previous blood transfusion, hepatitis B and C infection, and Class C Child Pugh.[17] Sethuraman and Balasubramanian analyzed that dehydration and infections were the most common precipitating factors for HE.[10]
The precipitating factors of HE were diverse in each study. Many patients have multiple precipitating factors. Infection/sepsis has been a common precipitating factor found in plentiful of research articles. Although it is difficult to predict this variation in the precipitating factor, as per the author, this variation probably can be attributed to regional differences, ethnic differences, and varying literacy rates among the patients. Compensated cirrhosis patients are usually asymptomatic; hence, majority of the studies found decompensated patients. Our study too reported 77.8% of child C patients. Decompensated cirrhosis is more prone to various liver-related complications including HE.
In one study, the majority of patients belonged to Grades III and II HE (39.81% and 36.89%, respectively), while only 3.88% belonged to Grade I.[10] We too found our majority of patients in Grade III (39%) and lowest in Grade I (14%).
A critical finding suggested in this study, was the association of infection and in-hospital mortality among HE patients. We are aware that liver cirrhosis patients are prone to infections, so any patient who present with clinical features suggestive of infection and HE might be at a higher risk of in-hospital mortality in comparison to those who do not have an infection. Infection was found as the mortality predictor by Onyekwere et al. too.[17] The infection was not found as the predictor of mortality in the study by Sethuraman and Balasubramanian who found association between hematemesis and mortality.[10] Furthermore, in our study, we found that a moderate positive association between MELD score and in-hospital mortality. The Pearson’s correlation coefficient was 0.335 between them, which suggests that as the MELD score increases the mortality also increases among HE patients. It is proposed that HE patients with a higher MELD score might be at higher risk for in-hospital mortality than those with lower MELD score.
It is vital to underline few of the limitations of this study. Besides involving fewer number of patients, it was a hospital-based study with no follow-up of patients after discharge. Hence, the author recommends a larger study with long follow-up of patients who are discharged after reversal of HE. Such studies will definitely give further insight about the regional differences that do occur. This study is first of its kind from this particular region of India, hence retaining its importance.
CONCLUSION
HE is associated with numerous morbidity and mortality for cirrhotic patients. A larger mass of such patients belongs to child Class C. Constipation and infections are the two most common precipitating factors for HE. There is an association between infection and/MELD score with inhospital mortality among HE patients. All HE patients who have concomitant infection and/or high MELD score should be managed on priority basis. Emphasis should be put on identifying the precipitating factors and devising various measures to treat and prevent them in future.
Declaration of patient consent
The Institutional Review Board permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- The global, regional, and national burden of cirrhosis by cause in 195 countries and territories, 1990-2017, A systematic analysis for the global burden of disease study 2017. Lancet Gastroenterol Hepatol. 2020;5:245-66.
- [CrossRef] [Google Scholar]
- Burden of liver diseases in the world. J Hepatol. 2019;70:151-71.
- [CrossRef] [PubMed] [Google Scholar]
- Hepatic encephalopathy. Gastroenterol Rep (Oxf). 2017;5:138-47.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term management of hepatic encephalopathy with lactulose and/or rifaximin: A review of the evidence. Eur J Gastroenterol Hepatol. 2019;31:434-50.
- [CrossRef] [PubMed] [Google Scholar]
- Beneficial effects of L-ornithine L-aspartate for prevention of overt hepatic encephalopathy in patients with cirrhosis: A systematic review with meta-analysis. Metab Brain Dis. 2020;35:75-81.
- [CrossRef] [PubMed] [Google Scholar]
- Schiff 's Diseases of the Liver. Oxford: John Wiley & Sons;. ;2017:1193.
- [CrossRef] [Google Scholar]
- Incidence of and risk factors for hepatic encephalopathy in a population-based cohort of Americans with cirrhosis. Hepatol Commun. 2019;3:1510-9.
- [CrossRef] [PubMed] [Google Scholar]
- Definition and nomenclature of hepatic encephalopathy. J Clin Exp Hepatol. 2015;5:S37-41.
- [CrossRef] [PubMed] [Google Scholar]
- Spectrum of chronic liver disease admitted to a medical college hospital in Northern India: Is there cause for concern? Indian J Gastroenterol. 2014;33:480-1.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical spectrum of precipitating factors of hepatic encephalopathy in cirrhosis of liver and its relation to prognosis in a tertiary care hospital-a retrospective study. Int J Contemp Med Surg Radiol. 2019;4:B65-70.
- [CrossRef] [Google Scholar]
- Etiology and mode of presentation of chronic liver diseases in India: A multi centric study. PLoS One. 2017;12:e0187033.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence, aetiology and related comorbidities of cirrhosis: A Swedish population-based cohort study. BMC Gastroenterol. 2020;20:84.
- [CrossRef] [PubMed] [Google Scholar]
- Burden of alcohol related admissions in the gastroenterology department of a North Indian tertiary care centre. Trop Gastroenterol. 2017;38:36-41.
- [CrossRef] [Google Scholar]
- Precipitating factors of hepatic encephalopathy at a tertiary care hospital Jamshoro, Hyderabad. J Pak Med Assoc. 2009;59:4.
- [Google Scholar]
- Presence of multiple precipitating factors of hepatic encephalopathy lead to late recovery and more mortality in cirrhotic patients. J Clin Exp Hepatol. 2015;5:S41.
- [CrossRef] [Google Scholar]
- 20. Precipitating factors of hepatic encephalopathy in liver cirrhosis and their impact on hospital stay and mortality-our center experience. J Clin Exp Hepatol. 2018;8:S60-1.
- [CrossRef] [Google Scholar]
- Chronic liver disease and hepatic encephalopathy: Clinical profile and outcomes. Niger J Clin Pract. 2011;14:181.
- [CrossRef] [PubMed] [Google Scholar]






