Translate this page into:
“Two tales of Frantz”: Varied presentations of solid pseudopapillary epithelial neoplasms of the pancreas
*Corresponding author: Mariya Jacob, Department of General Surgery, Sri Ramakrishna Hospital, Coimbatore, Tamil Nadu, India. theeditor13@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Jacob M, Bharathan A, Balaraman K, Venugopal S. “Two tales of Frantz”: Varied presentations of solid pseudopapillary epithelial neoplasms of the pancreas. Indian J Med Sci. 2025;77:43-5. doi: 10.25259/IJMS_264_2024
Abstract
Frantz tumors or solid pseudopapillary epithelial neoplasms (SPEN) are rare pancreatic neoplasms seen in young, adolescent females, and rarely affect adult men. They are one of the most common pediatric pancreatic tumors and are most commonly seen in the distal pancreas (body and tail). Here, we present the two cases of Frantz tumor, of which the first is a classical presentation - SPEN tumor in the pancreatic body in a 9-year-old girl child, while the second is a rarer presentation in an adult male with the tumor located in the head of pancreas. Both patients presented with abdominal pain as their initial complaint and eventually underwent complete excision of the tumor. The contrasting features of the same tumor in both patients highlighted the need for us to report them as well as to review the tumor in general.
Keywords
Frantz tumor
Pancreatic tumors
Pediatric tumors
INTRODUCTION
Solid pseudopapillary epithelial neoplasms (SPEN), also known as Frantz tumors, are rare pancreatic neoplasms of low malignant potential predominantly affecting young females. They account for approximately 0.13–2.7% of all pancreatic tumors,[1] representing nearly 70% of pancreatic lesions in the pediatric population. SPEN typically presents as a well-encapsulated, mixed tumor that can vary in size and often remains asymptomatic until significant growth occurs. This case report discusses the two distinct presentations of SPEN, emphasizing the differences in age, gender, tumor location, and surgical outcomes.
CASE REPORTS
Case 1
A 9-year-old girl diagnosed with Kawasaki disease (since age-1) presented with complaints of abdominal pain for 2 days. On examination, she was vitally stable with no abdominal tenderness or palpable mass. Blood investigations were normal. Ultrasound (USG) scan of the abdomen done outside showed a space-occupying-lesion in the pancreatic body. Contrast-enhanced computed tomography scan of the abdomen [Figure 1] showed a well-defined enhancing solid mass of 3.5 × 2.9 cm in the pancreatic neck region, causing narrowing of the splenic vein and portal confluence.
Endoscopic USG [Figure 2] confirmed the tumor location in the neck/proximal body of the pancreas, at portal vein confluence. Intraoperatively, the lesion was found encapsulated with nodes along the common hepatic duct region. Postoperative recovery was uneventful. Histopathological examination was reported as SPEN with tumor-free margins, absent capsular/vascular invasion, mitotic activity of <1/10 hpf, and beta-catenin positivity.

- Contrast-enhanced computed tomography of the abdomen image showing hypodense lesion at junction of the head and body of the pancreas (red arrow).

- Endoscopic ultrasound showing heteroechoic lesion at the pancreatic neck (red arrow). The blue cross indicates the diameter of the swelling.
Case 2
A 41-year-old male with no comorbidities, presented with complaints of severe, nonradiating upper abdominal pain for 2 days along with a 6-month history of anorexia and weight-loss (5 kg). He has no past history of upper abdominal pain, vomiting, or jaundice. He was found anicteric, afebrile, and vitally stable. There was no abdominal tenderness or palpable lump. His blood investigations revealed elevated prothrombin time - International normalised ratio (PT-INR) (30 s–2.1) and activated partial thromboplastin time (APTT) of 51 s. Rest investigations were normal. USG scan of the abdomen [Figure 3] showed a 4.7 × 4.2 × 3.5 cm, hypoechoic lesion with internal calcifications in the pancreatic head and uncinate process, with compression of portal vein and superior mesenteric vein. CECT abdomen showing ill-defined hypodense lesion with predominantly solid and minimal cystic components, in the head of pancreas. the solid component shows late arterial enhancement [Figure 4].
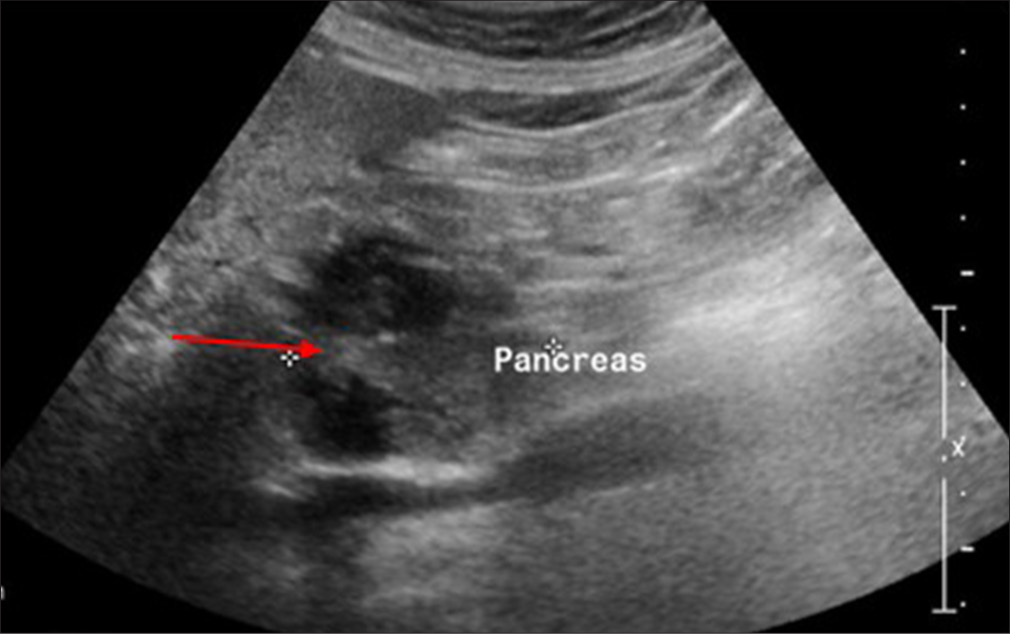
- Ultrasound of the abdomen showing heteroechoic lesion (red arrow) in the pancreatic head with few hypoechoic areas within.

- Contrast-enhanced computed tomography of the abdomen showing ill-defined hypodense lesion (red arrow) with predominantly solid and minimal cystic components, in the head of pancreas. The solid component shows late arterial enhancement.
Endoscopic ultra-sonography guided fine needle aspiration (EUS-FNA) biopsy done outside revealed it as SPEN. After optimization, he underwent Whipple’s pancreaticoduodenectomy. Intraoperatively, mass was found to be in close contact with the major vessels, but could be separated in-toto from them. Post-operative recovery was stormy as patient had infarction of a portion of the greater omentum with abdominal wound infection and pus discharge which prompted re-operation to avoid wound dehiscence, on postoperative day 16. Following this, recovery was uncomplicated. Histopathological report confirmed the diagnosis of SPEN with R0 resection margins and absent metastasis in peritumoral lymph nodes.
DISCUSSION
SPEN or Frantz tumors are rare pancreatic exocrine neoplasms of low malignant potential, seen in young and adolescent females and rarely affecting adult men.[1] They account for 0.13–2.7% of all pancreatic tumors but almost 70% of pediatric pancreatic lesions.[1] The hypothesized etiology is that these neoplasms develop from either pluripotent pancreatic stem cells or cells of female genital epithelial origin due to increased prevalence in younger females.[1] They can be locally invasive and when it occurs in adult males, is found to be more aggressive with 5% of patients developing metastases.[2] Asymptomatic nature of the tumor thus causes it to grow to a large size before detected. The commonly seen symptoms include abdominal pain, abdominal discomfort, nausea, vomiting, loss of appetite, early satiety, or weight-loss. A palpable abdominal mass may be present on the physical examination. Obstructive jaundice is extremely rare, even in cases with tumor at the pancreatic head.[2]
SPEN are usually well-demarcated and well-encapsulated, mixed (solid and cystic) tumors,[3] with an average diameter of 6 cm. Although it can occur anywhere along the pancreatic parenchyma, it is most common in the body and tail. Malignant tumors will have capsular invasion or adjacent structure infiltration. The most commonly reported procedures are distal pancreatectomy (with or without splenic preservation), pancreato-duodenectomy, local resection/enucleation.[4] Following surgical resection, pediatric patients have an excellent prognosis and a disease-free survival rate of >95%.[5] Survival is better in children than adults, mostly due to differences in tumor biology and presence of comorbidities in adults.[5] Metastases is seen in about 12–15% of cases (mostly in adults than children). Surgical debulking could be curative in metastases (unlike pancreatic cancer).[2] Recurrence rate of 2–6% is usually seen in infliltrative tumors. Even metastasized cases have a long survival rate.[6] Poor prognosis is expected when tumor size is >5 cm, with vascular/local invasion into adjacent structures, male gender, and presence of necrosis or cellular atypia[2] on histopathology.
Case 1 is a classic case of SPEN affecting a young girl and located in the pancreatic body. Case 2 is a rarer presentation happening in an adult male with tumor in the pancreatic head. Both were symptomatic with abdominal pain just like 49%[2] of the cases. The contrasting presentations of the same disease, based on age, gender, tumor location, and surgical modality, but their similarity in presenting complaint and postoperative recovery had to be brought to the attention of the surgical community. This is imperative as the chances of metastases, postoperative complications, and overall survival rate are poorer in adults than in children.
CONCLUSION
SPENs are rare and have a varied presentation, thus presenting unique clinical challenges. The outcome is favorable when diagnosed and managed promptly and appropriately. This report highlights the clinical spectrum as well as the outcome of SPEN in different age groups, thus emphasizing the need for the awareness among healthcare professionals regarding the same.
Ethical approval
Institutional Review Board approval was not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Solid pseudopapillary neoplasms of the pancreas: A surgical and genetic enigma. World J Surg. 2017;41:1871-81.
- [CrossRef] [PubMed] [Google Scholar]
- Solid pseudopapillary pancreatic tumor-tumor of frantz. Surg Gastroenterol. 2019;24:259-64.
- [CrossRef] [Google Scholar]
- Clinical and pathological features of solid pseudopapillary neoplasms of the pancreas: A nationwide multicenter study in Japan. Pancreas. 2018;47:1019-26.
- [CrossRef] [PubMed] [Google Scholar]
- Solid pseudopapillary tumor of the pancreas: Clinical features and imaging findings. Clin Imaging. 2018;48:113-21.
- [CrossRef] [PubMed] [Google Scholar]
- Solid pseudopapillary tumor of the pancreas: A single-center experience and review of the literature. In Vivo. 2017;31:501-10.
- [CrossRef] [Google Scholar]
- Comparison of pediatric and adult solid pseudopapillary neoplasms of the pancreas. J Surg Res. 2019;242:312-7.
- [CrossRef] [PubMed] [Google Scholar]






