Translate this page into:
Unraveling the quivering dance: Trichomoniasis
*Corresponding author: Archana Rajan, Department of Medicine, All India Institute of Medical Sciences (AIIMS), Delhi, India. archanarajan29@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Rajan A, Kapil N. Unraveling the quivering dance: Trichomoniasis. Indian J Med Sci. 2024;76:89-90. doi: 10.25259/IJMS_233_2023
Abstract
This case report delves into an atypical presentation of trichomoniasis in a previously healthy 56-year-old female. Presenting with burning micturition and pruritus, the patient’s urine microscopy revealed characteristic twisting motility of Trichomonas vaginalis, confirming the diagnosis. Treatment with metronidazole resulted in prompt symptomatic improvement. This case underscores the importance of recognizing diverse presentations of Trichomoniasis for accurate diagnosis and timely intervention.
Keywords
Trichomoniasis
Urinary tract infection
Sexually transmitted diseases
INTRODUCTION
Trichomoniasis, caused by Trichomonas vaginalis, commonly manifests as urogenital infections. This case delves into an unusual presentation of the infection, emphasizing the need for clinicians to consider diverse clinical scenarios.
CASE REPORT
A 56-year-old female with no prior comorbidity presented with complaints of burning micturition, pruritus and increased frequency of urine for the past 1 week. On further probing, she revealed occasional grayish-white discharge which she considered insignificant. On examination, she was vitally stable and systemic examination was unremarkable. Her laboratory examination revealed a total leucocyte count-15,240/μL, with 86.1% neutrophils (reference range, 48–76), 12.8% lymphocytes (reference range, 18–41), 2.1% monocytes (reference range, 4–11), the hemoglobin level was 13.6 g/dL, and the platelet count 338,000 per microliter. The erythrocyte sedimentation rate was 50 mm/h (reference range, 0–20), and the C-reactive protein level was 38 mg/L (normal <10 mg/L), kidney function test and blood sugar level were within normal limits. With suspicion of urinary tract infection, we did a urine routine microscopy revealed characteristic twisting motility or quivering motility of which T. vaginalis [Figures 1 and 2]. Thus, a diagnosis of trichomoniasis was made. She was treated with 7-day course of 500 mg metronidazole twice daily following which she improved symptomatically and symptoms did not recur.[1]
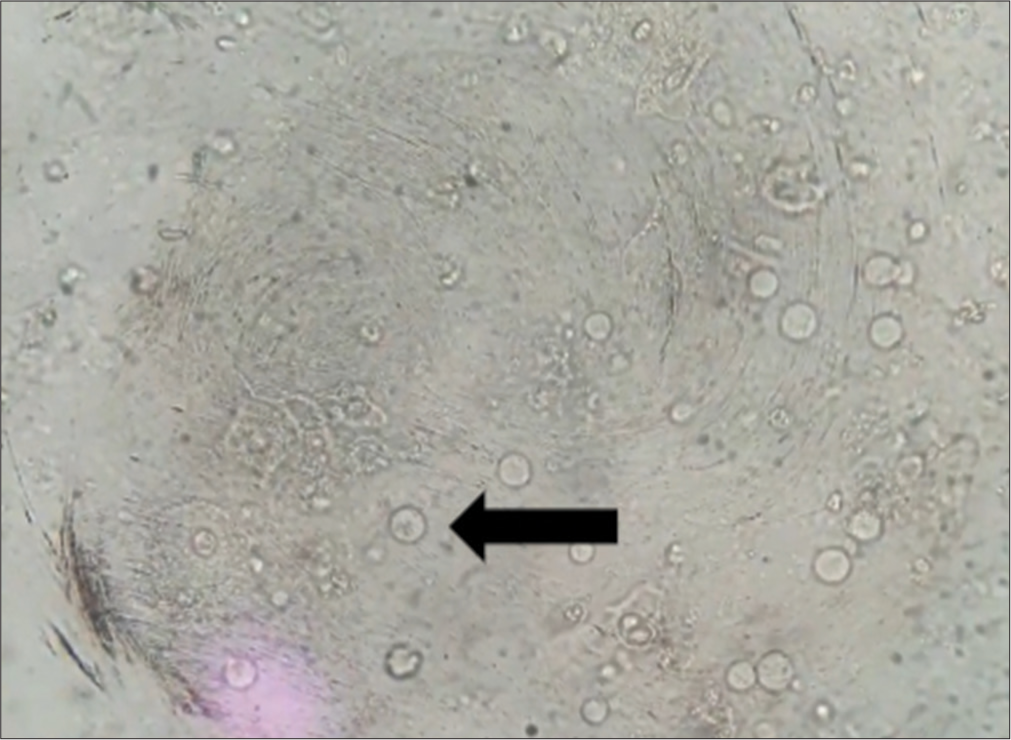
- Urine microscopic examination showing field full of Trichomonas vaginalis (black arrowhead).

- Urine microscopic examination of same patient-Trichomonas vaginalis-internal structure is also visible.
DISCUSSION
T. vaginalis is pear-shaped or oval in appearance, with a size ranging from 10 μm to 20 μm in length, has four flagella, which are whip-like structures that extend from the front of the organism, along with an undulating membrane, which is a thin, wavy membrane extending along the organism’s length. The parasite contains a single, centrally located nucleus, which is often visible in the body of the organism and cytoplasm of T. vaginalis appears granular and may contain ingested bacteria, erythrocytes, or other debris.[2]
Trichomoniasis, caused by the protozoan parasite T. vaginalis, commonly manifests as a urogenital infection. In this case, the patient’s atypical presentation with burning micturition, pruritus, and increased urine frequency prompted a thorough diagnostic investigation. The identification of characteristic twisting motility of T. vaginalis in urine microscopy was pivotal in confirming the diagnosis.
The patient’s lack of prior comorbidities and the absence of typical risk factors for Trichomoniasis make this case noteworthy. The atypical presentation underscores the importance of maintaining a high index of suspicion for parasitic infections even in patients without conventional risk factors. Moreover, the patient’s asymptomatic grayish-white discharge, initially considered insignificant, serves as a reminder that subtle symptoms may be indicative of underlying infections and warrant careful exploration during clinical assessments.
The laboratory findings revealed an elevated total leucocyte count with a predominance of neutrophils, indicating an inflammatory response to the infection. The inflammatory markers, including an elevated erythrocyte sedimentation rate and C-reactive protein level, further supported the diagnosis. While these laboratory parameters are nonspecific, they contribute to the overall clinical picture, emphasizing the need for a comprehensive diagnostic approach.
The prompt resolution of symptoms following a 7-day course of metronidazole highlights the efficacy of targeted treatment for trichomoniasis. The patient’s favorable response aligns with established guidelines for managing this parasitic infection, emphasizing the importance of accurate identification for appropriate therapeutic interventions.
CONCLUSION
This case illuminates an uncommon presentation of trichomoniasis, emphasizing the necessity of a comprehensive diagnostic strategy. Recognition of the characteristic motility in urine microscopy enabled precise diagnosis and effective treatment. Clinicians should remain vigilant for diverse presentations of trichomoniasis to enhance timely intervention.
Acknowledgment
To co-author for data collection and concept.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Diagnosis and management of trichomonas vaginalis: Summary of evidence reviewed for the 2021 centers for disease control and prevention sexually transmitted infections treatment guidelines. Clin Infect Dis. 2022;74(Suppl_2):S152-61.
- [CrossRef] [PubMed] [Google Scholar]
- Trichomoniasis In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2023. Available from: http://www.ncbi.nlm.nih.gov/books/NBK534826 [Last accessed on 2023 Aug 09]
- [Google Scholar]







