Translate this page into:
Epithelioid rhabdomyosarcoma: A rare case report mimicking carcinoma breast

*Corresponding author: Sneha Jatan Bothra, Department of Medical Oncology, Rajiv Gandhi Cancer Institute and Research Center, New Delhi, India. snehabothra2@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bothra SJ, Sharma M, Jain P, Bansal D, Batra U. Epithelioid rhabdomyosarcoma: A rare case report mimicking carcinoma breast. Indian J Med Sci 2021;73(1):127-9.
Abstract
Rhabdomyosarcoma (RMS) is an unusual sarcoma in adults. There are four main types of RMS described in the literature, including embryonal, alveolar, pleomorphic, and spindle cell type. Epithelioid RMS is a relatively newer form of RMS described in the literature, with little information regarding the natural course and management. We present a rare case of a young woman with metastatic epithelioid RMS, with an atypical presentation with bilateral large breast lumps, large ovarian mass progressing rapidly to metastasize, involving multiple sites. It has an aggressive clinical course with poor response to therapy.
Keywords
Epithelioid rhabdomyosarcoma
Breast lumps
Metastatic sarcoma
Aggressive sarcoma
INTRODUCTION
Rhabdomyosarcoma (RMS) is a type of soft-tissue sarcoma commonly occurring in children less than 10 years of age, which is an exceedingly rare variety in adults. It is classified by the WHO into four major types, embryonal RMS, alveolar RMS, pleomorphic RMS, spindle cell RMS,[1] and a newer subtype called epithelioid RMS.[2] The epithelioid variant of RMS is a newly described distinct entity which demonstrates epithelioid morphology with poorly differentiated tumors. We, here, describe a case report of a 21-year-old woman, mother of a 2-year-old child, with rapidly progressive breast lumps mimicking benign breast disease.
CASE REPORT
A 20-year-old married woman with irregular menses presented with a history of lumps in both breasts gradually increasing over the past 5 months. She was evaluated at her local place, where a provisional diagnosis of fibroadenoma was made and she was kept on follow-up. However, as the lumps continued to increase in size, she underwent a fine needle aspiration cytology (FNAC). FNAC was positive for malignant cells. She was then referred to our institute for further management.
On detailed history taking, she revealed that there were bilateral breast lumps which progressively increased in size, with increasing abdominal distension. On physical examination, she was cachectic, poorly built, and poorly nourished. General physical examination revealed a baseline tachycardia and pallor. She had bilateral large breast lumps which were hard in consistency, mobile, not adhered to the skin, or the underlying muscle. The chest was clear on auscultation.
The liver and spleen were not palpable but had a palpable abdominal lump with a tensely distended abdomen with massive ascites. She underwent further diagnostic and staging workup.
PET CT scan revealed a metabolically active ill-defined soft-tissue mass in the cervix extending to involve the bilateral adnexa, uterus, and vagina. Multiple metabolically active abdominal and mediastinal lymph nodes were also present with subcentimetric lung parenchymal nodules. Bilateral breast showed multiple metabolically active necrotic soft-tissue lesions (largest 5.8 x 3.2 cm in the right upper quadrant). There was the presence of a metabolically active diffuse peritoneal and omental thickening with evidence of mass formation. No other metabolically active disease was found. Of the tumor markers, CA-125 was 849, S. CEA and CA 19.9 were normal. Her endoscopy and colonoscopy were normal.
Histopathology from the breast lump revealed breast tissue infiltrated by the tumor, with tumor cells arranged in diffuse sheets [Figure 1]. Individual cells are round to polygonal, having moderate to abundant eosinophilic cytoplasm, with oval to irregular peripherally nucleated vesicular to hyperchromatic nuclei with few displaying conspicuous nucleoli. On immunohistochemistry, the tumor cells are positive for myogenin and desmin [Figure 2], while negative for CK, GATA3, PAX-8, SALL 4, CD34, LCA, and S100. The tumor cells display retained expression if INI-1 suggestive of epithelioid RMS. She was diagnosed to have International Rhabdomyosarcoma Group Stage 4 epithelioid RMS. The site of the primary could not be ascertained.
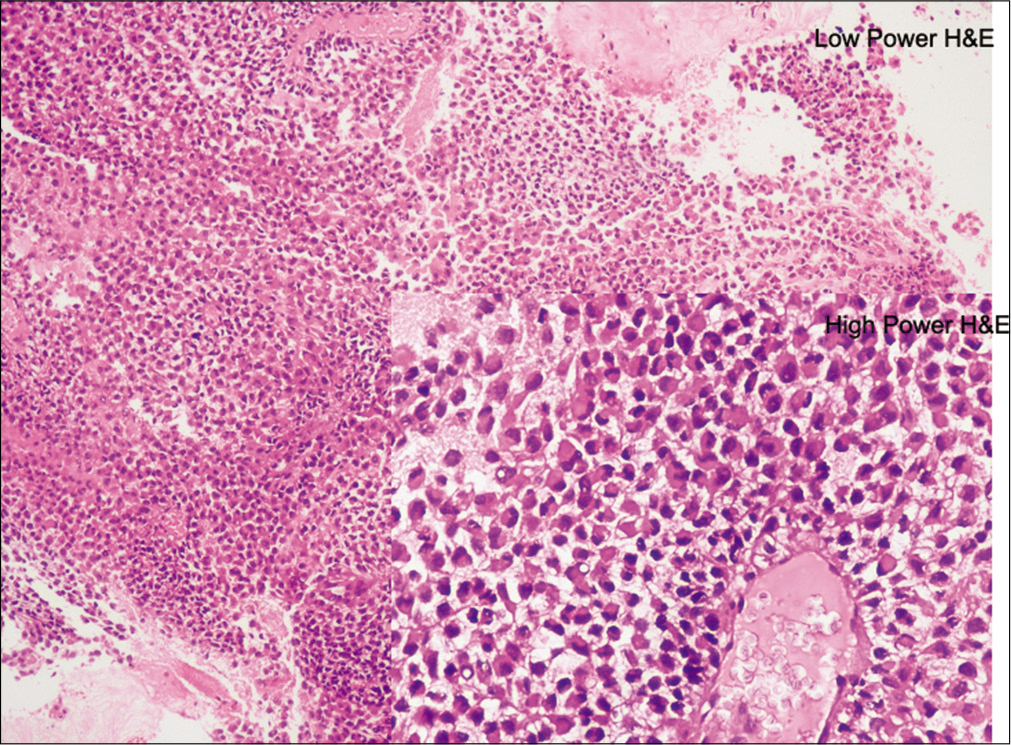
- Low and high power H&E stain showing diffuse sheet-like growth of uniformly sized epithelioid cells with abundant amphophilic to eosinophilic cytoplasm, large vesicular nuclei, and frequent prominent nucleoli.
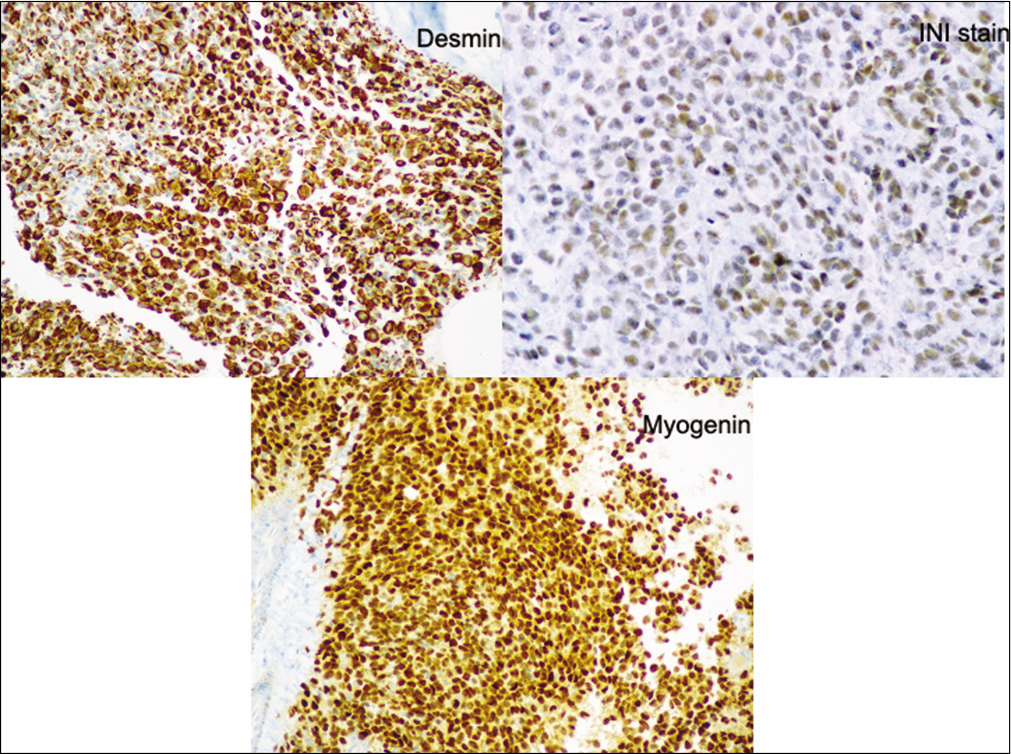
- IHC suggestive of INI, desmin, and myogenic positivity diffusely.
After stabilization of her general condition, she was started on vincristine, adriamycin, and cyclophosphamide-based palliative chemotherapy. During the course of chemotherapy, she required multiple abdominal paracentesis. She also had episodes of Grade 4 febrile neutropenia, requiring dose reduction. After completion of three cycles of chemotherapy, the patient was re-evaluated. Reassessment with whole-body PET CT scan was suggestive of progressive disease. In view of poor general condition and poor tolerance to chemotherapy, she was advised for the best supportive care with therapeutic abdominal paracentesis and pain management. The patient continued to progress and deteriorate, with severe hypoproteinemia and malignant ascites requiring recurrent paracentesis. She then succumbed to the disease in a month.
DISCUSSION
RMS is an infrequent variety of sarcoma in adults. Soft-tissue sarcoma comprises <1% of all adult solid tumors, and only 3% of the soft-tissue sarcomas are RMS subtype.[3] RMS is classified into its four subtypes, including the alveolar, embryonal, pleomorphic, and spindle cell subtypes. Recently, a newer variant of RMS has been described, namely, the epithelioid variant.[2] There are various differences between pediatric and adult RMS. It tends to be more aggressive and with poor prognosis in adults. Adult RMS patients have an increased chance of having a primary tumor at unfavorable anatomic sites.
Histologically, these tumors are usually composed of diffuse sheet-like growth of uniformly sized epithelioid cells with abundant amphophilic to eosinophilic cytoplasm, large vesicular nuclei, and frequent prominent nucleoli and reminiscent of poorly differentiated carcinoma. In our patient, the diagnosis was a little tricky as it was a breast tissue biopsy, showing a similar picture, where it could be a poorly differentiated carcinoma of the duct or the epithelioid sarcoma.[4] However, on immunohistochemistry, the tumor cells are positive for myogenin and desmin, while negative for CK, GATA3, PAX-8, SALL 4, CD34, LCA, and S100. The tumor cells display retained expression if INI-1. There are few case series which discuss the aggressive behavior of this tumor.[2,5] Due to a lack of clinical trials in this type of RMS, treatment is variable. In this case, a young woman, who presented with bilateral mobile breast lumps, was thought to be benign, leading to the delay in diagnosis. However, due to the delay, she was diagnosed in a very advanced stage, when chemotherapy could no longer halt the disease progression. The disease in this patient was very aggressive, rapidly progressive with minimal response to the chemotherapy.
CONCLUSION
Epithelioid rhabdomyosarcoma is a new and rare entity. Its presentation may be stormy with rapid progression and minimal response to therapy. Diagnosis is confirmed by immunohistochemistry. Early diagnosis is the key to improvement in the oncological outcomes.
Another learning point from this case is that not all breast lumps in young woman are the benign and increasing the size of the breast lump must be further investigated.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- WHO Classification of Tumours of Soft Tissue and Bone, World Health Organization Classification of Tumours Lyon: IARC; 2013.
- [Google Scholar]
- Epithelioid rhabdomyosarcoma: Clinicopathologic analysis of 16 cases of a morphologically distinct variant of rhabdomyosarcoma. Am J Surg Pathol. 2011;35:1523-30.
- [CrossRef] [PubMed] [Google Scholar]
- Rhabdomyosarcoma in adults. A retrospective analysis of 171 patients treated at a single institution. Cancer. 2003;98:571-80.
- [CrossRef] [PubMed] [Google Scholar]
- Epithelioid Rhabdomyosarcoma; a case report with immunohistochemical and molecular study. Diagn Pathol. 2015;10:124.
- [CrossRef] [PubMed] [Google Scholar]
- Epithelioid rhabdomyosarcoma: A clinicopathological study of seven additional cases supporting a distinctive variant with aggressive biological behaviour. Pathology. 2015;47:667-72.
- [CrossRef] [PubMed] [Google Scholar]






