Translate this page into:
Scleral tunnel based sutureless extracapsular cataract extraction: An approach to astigmatic correction in soft cataracts of nuclear sclerosis grade 1
*Corresponding author: Narendra Kumar Keisham, Department of Ophthalmology, Military Hospital, Jabalpur Cantonment, Madhya Pradesh - 482001, India. drnareneye_afmc@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Keisham NK, Sharma A. Scleral tunnel based sutureless extracapsular cataract extraction: An approach to astigmatic correction in soft cataracts of non-structural protein 1 grade nuclear sclerosis. Indian J Med Sci 2021;73:305-10.
Abstract
Objectives:
A study to see if scleral tunnel based sutureless extracapsular cataract extraction with superior quadrant approach can correct pre-existing corneal astigmatism in soft cataracts of non-structural protein 1 (NS1) grade nuclear sclerosis in patients of younger age profile having “with-the-rule” pattern of corneal astigmatism.
Material and Methods:
47 eyes of 41 patients who underwent scleral tunnel based sutureless extracapsular cataract extraction were taken as the study group and a second group of 44 eyes of 38 patients who underwent clear corneal incision based phacoemulsification surgery formed the control group. Soft cataracts of NS1 grade nucleus having “with-the-rule” corneal astigmatism were included in the study. Keratometry measurements were done preoperatively and at 6 weeks post-operative follow-up by Zeiss IOLMaster.
Results:
Sutureless scleral tunnel based extracapsular cataract extraction was found to neutralize pre-existing corneal astigmatism if it was in range of 1.0–1.5 D. It was also found to change the pattern of astigmatism from “with-the-rule” to “against-the-rule” if the pre-operative astigmatism was in the range of 0.5–1.0 D with little change in the absolute value of the astigmatism.
Conclusion:
Patients with pre-existing with-the-rule corneal astigmatism undergoing scleral tunnel based sutureless extracapsular cataract extraction had reduced corneal astigmatism. Phacoemulsification, on the other hand, was found to be an astigmatically neutral surgery.
Keywords
Corneal astigmatism
Sutureless extracapsular cataract extraction
Phacoemulsification
Keratometry
INTRODUCTION
Cataracts are caused by the degeneration and opacification of lens fibers already formed, the formation of aberrant lens fibers or the deposition of other materials in their place.[1] Treatment remains surgical removal with implantation of an intraocular lens. With advancements in technology, cataract surgery is now also expected to be a refractive surgery in addition to being a lenticular surgery and patients expect post-operative freedom from spectacles along with a painless visual recovery.
There is a constant effort by ophthalmologists to come up with surgical innovations to improve the visual outcome following cataract surgery. Extraction by phacoemusification and placement of a posterior chamber intraocular lens in the capsular bag has become the routine procedure in most parts of the world. Scleral tunnel based sutureless extracapsular cataract surgery (also known as manual small incision cataract surgery in some parts of the world) had often been considered a low technology, unproven technique compared with phacoemulsification.[2] However, it remains an important tool for eliminating blindness due to cataract especially in the developing countries[3] and studies have reported equivalent outcomes between these two surgical techniques.[4,5] However, astigmatism remains an important cause of low uncorrected visual acuity in post-operative patients.[6] One of the advantages of phacoemulsification reported in the literature is better unaided visual acuity compared with the extracapsular technique as the result of less surgical-induced astigmatism seen in phacoemulsification.[7] While this may be true for harder cataracts as their removal by manual scleral tunnel based extracapsular extraction will require larger incisions, the clinical significance of this difference in surgical induced astigmatism between these two techniques remains debatable.[8] And cataracts with softer nuclei will require smaller incisions with manual scleral tunnel based extracapsular extraction and post-operative astigmatism can be reduced by choosing the right surgical approach and the pattern of incision in these cases.[9]
The manual scleral tunnel based extracapsular cataract extraction has undergone innovative changes and often times considered as alternate option for phacoemulsification particularly in developing countries due to lack of resources. It is also a much faster and cost-effective technique. This study was done to see if this surgical technique can reduce or neutralize a pre-existing “with-the-rule” corneal astigmatism in soft cataracts of non-structural protein 1 grade nucleus.
MATERIAL AND METHODS
Study design
A prospective interventional study was conducted at the ophthalmology center of a military hospital of the Indian Armed Forces.
Study population
47 eyes of 41 patients underwent scleral tunnel based sutureless extracapsular cataract extraction and formed the study group. A control group of 44 eyes of 38 patients who underwent clear corneal incision based phacoemulsification surgery was also taken. Patients were included in the study after obtaining informed and written consent. All eyes in both groups had soft cataractous lens of nuclear sclerosis Grade 1 based on the lens opacity classification system III[10] after clinical examination with slit lamp bio-microscopy. All the eyes included in the study and control groups had “with-the-rule” corneal astigmatism with the steeper corneal axis between 70° and 120°. Eyes with other pre-existing ocular morbidities were excluded from both the study and control groups.
Study procedure
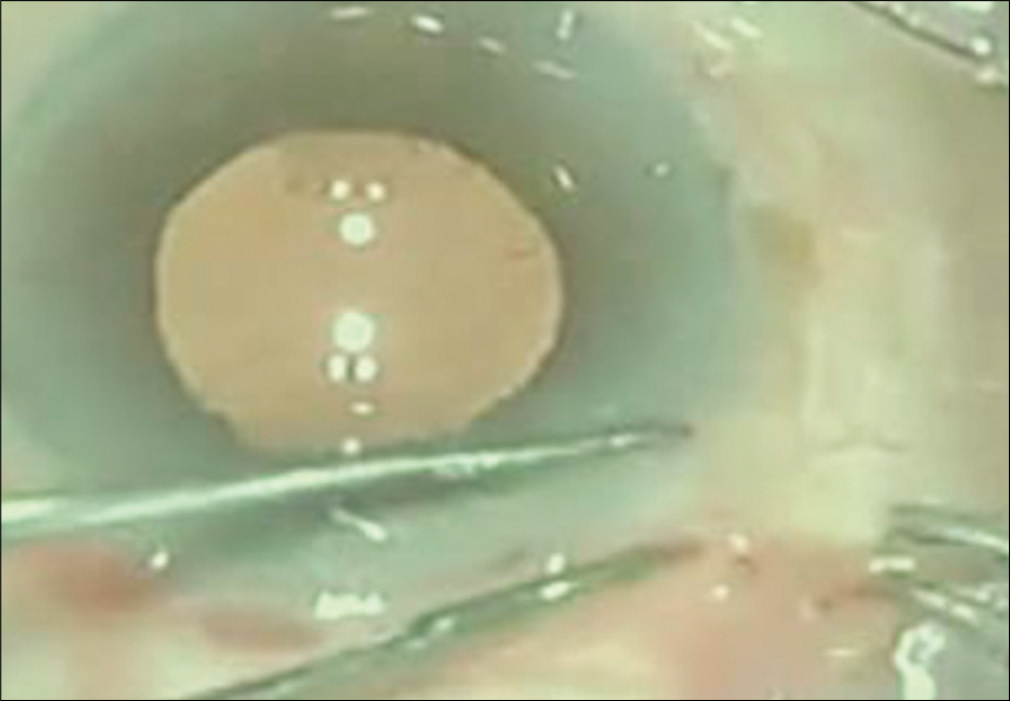
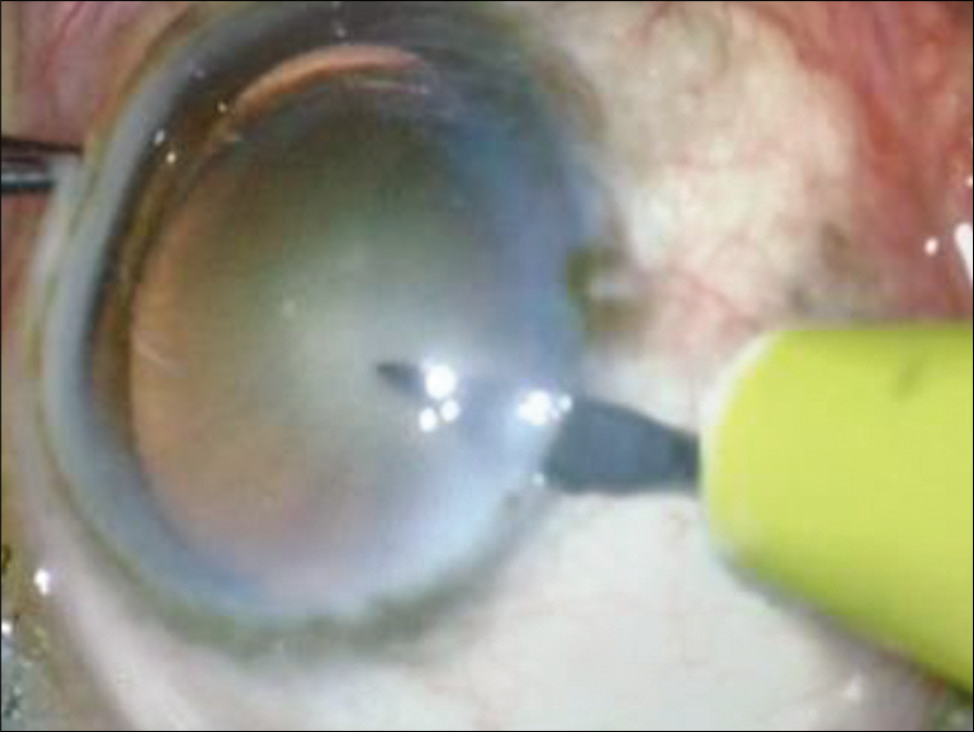
For all eyes operated in the study group, peribulbar anesthesia with mixture of lignocaine 2%, bupivacaine 0.5%, and hyaluronidase was given. Superior rectus bridle suture was passed with 4–0 prolene suture. Peritomy was done superiorly from 10 O’clock to 2 O’clock and any bleeding vessels visible in the scleral bed were cauterized with bipolar cautery. A side stab incision was made between 9 O’ clock and 10 O’clock positions with the side port knife [Figure 1] and entry made into the anterior chamber. This was followed by staining of the anterior lens capsule with trypan blue dye. Continuous curvilinear capsulorrhexis (CCC) was done with the bent tip of a 26G needle [Figure 2]. After completion of capsulorhexis, a 6.00 mm long and 300–400 micron deep incision was made on the sclera in the shape of a frown with the center of the incision line being 2 mm away from the limbus, and the end points of the incision line being 4.0–4.5 mm away from the limbus. Then, through this incision line a scleral tunnel was constructed using crescent ophthalmic knife forming a trapezoid shaped tunnel wound with the inner end of the tunnel about 7 mm in length and extending 1.5 mm into the clear cornea and into the sides forming scleral pockets [Figure 3]. Then, entry was made into anterior chamber using a keratome knife through the scleral tunnel wound. Cortical cleaving hydrodissection was done and nucleus rotated inside the bag and dialled out of the bag with the sinskey hook. Hydroxypropylmethyl cellulose 2% gel was injected between the lens and corneal endothelium and below the lens to inflate the capsular bag and lens delivery was done by visco-expression by pressing down the posterior lip of the scleral tunnel to open it up or with a wire vectis [Figure 4]. Anterior chamber was reformed; residual cortical matter aspirated using a simcoe two-way irrigation/aspiration cannula. A rigid 6.00 mm optic polymethyl methacrylate posterior chamber intraocular lens was implanted in the capsular bag. Residual viscoelastic was removed [Figure 5], intracameral preservative free moxifloxacin hydrochloride 0.5% solution was given, the side port incision was hydrated, and conjunctiva over the scleral tunnel was reposited back by using cautery [Figure 6].
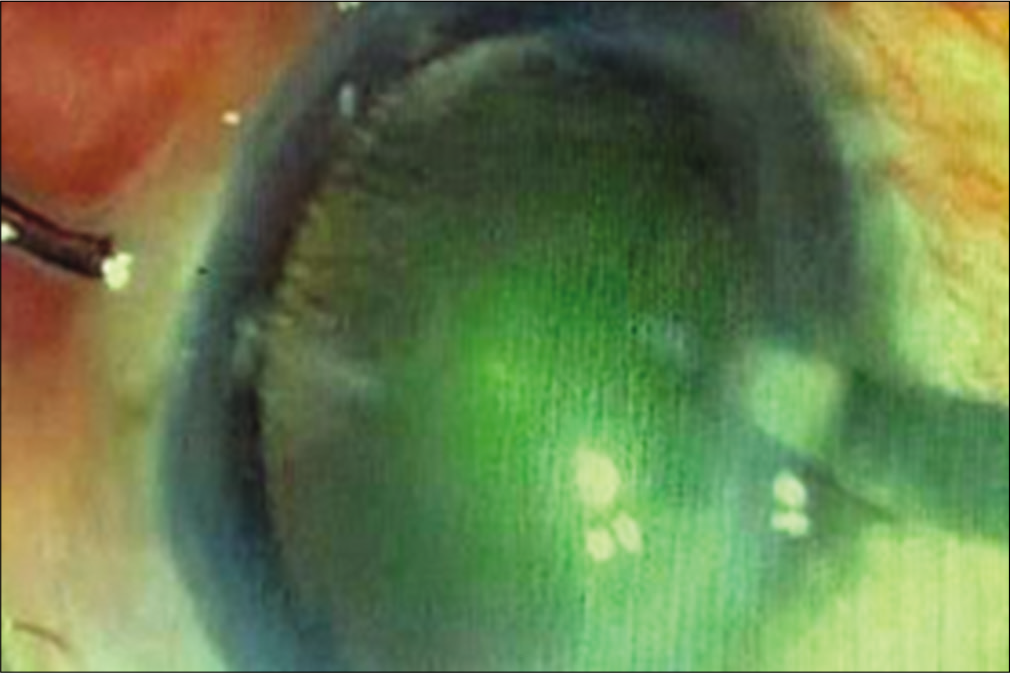
- Side port incision between 9 O clock and 10 O clock.
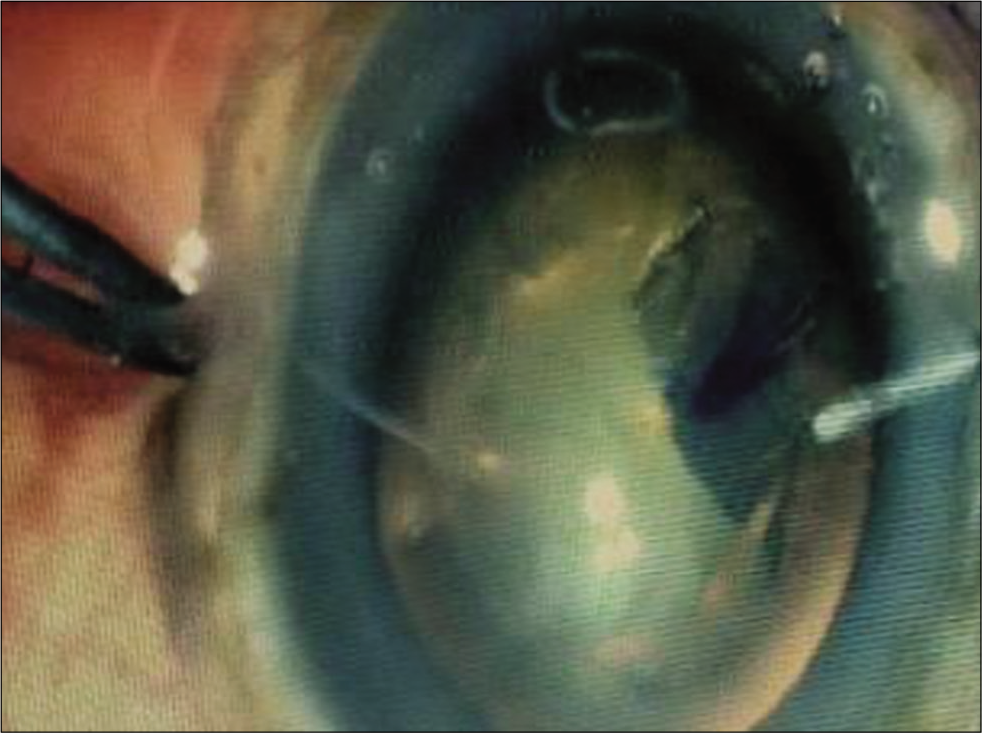
- Continuous curvilinear capsulorhexis.

- Construction of the scleral tunnel using crescent knife.
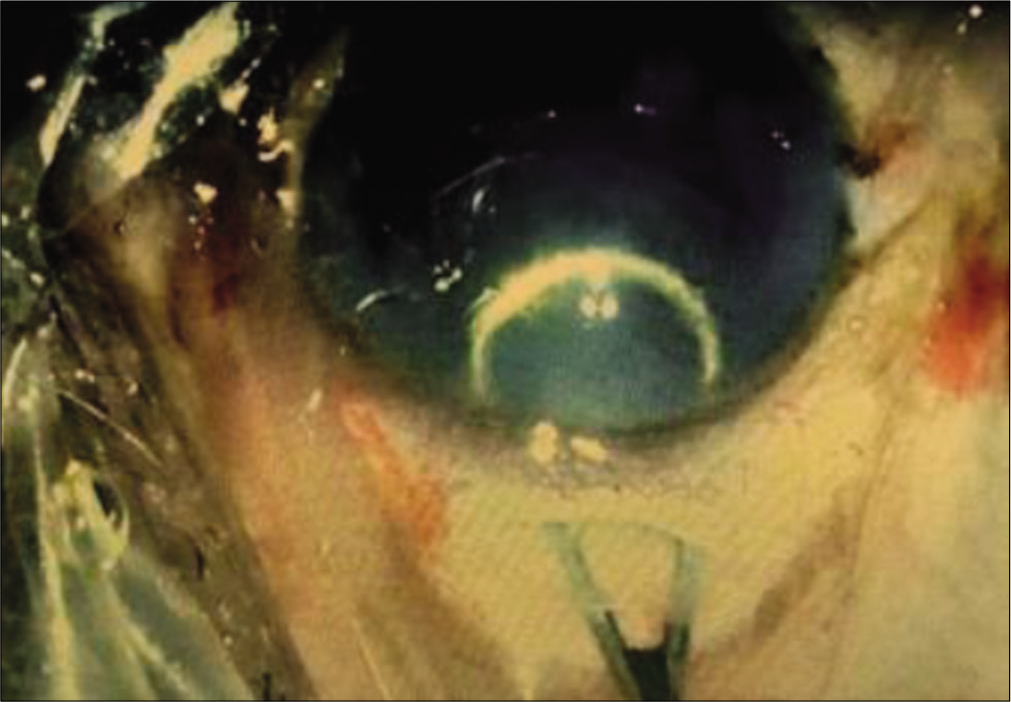
- Nucleus delivery using wire vectis.

- Posterior chamber intraocular lenses in bag with simcoe cannula in anterior chamber.
- Reposition of conjunctiva using cautery.
| Study group | Control group | Calculated t-value (Independent samples t-test) | |
|---|---|---|---|
| Age in years | 48.23+2.60289 (SD) | 48.84+2.91702 (SD) | –1.0553 |
| Percentage of males | 30 males out of 41 patients (73.17%) |
27 males out of 38 patients (71.05%) |
– |
| Eyes having unaided VA 6/9 or better at 6 weeks | 41 out of 47 eyes (87.23 %) | 37 out of 44 eyes (84.09%) | – |
| Mean unaided visual acuity at 6 weeks (logMAR) | 0.15872+0.07264 (SD) | 0.17318+0.06205 (SD) | –1.01171 |
| The average time for surgery in minutes | 14.2766+1.65111 (SD) | 21.3182+1.72226 (SD) | 19.796 |
| Mean surgical induced astigmatism in diopters | 0.81511+0.14663 (SD) | 0.43591+0.05880 (SD) | 15.895 |
Eyes in the control group were also operated under peribulbar anesthesia. A side stab incision was made between 9 O’clock and 10 O’clock positions by a side port knife and entry made into the anterior chamber [Figure 7]. This was followed by staining of the anterior lens capsule with trypan blue dye. CCC was performed with the bent tip of a 26G needle [Figure 8]. A clear corneal main incision was made at 11 O’clock position with a 2.8 mm keratome knife [Figure 9]. Another side stab incision was made at 1 O’clock position. Cortical cleaving hydrodissection was done and nucleus rotated inside the bag. Stop and chop technique of nucleotomy was done in which trench was made in nucleus, nucleus was divided into two halves [Figure 10] and phacoemulsified. This was followed by aspiration of remnant cortical matter with bimanual irrigation-aspiration cannulae [Figure 11]. In cases, where it was difficult to divide the nucleus, it was prolapsed out of the capsular bag into the anterior chamber and emulsified after coating the corneal endothelium with chondroitin sulfate-sodium hyaluronate gel. Alcon INFINITI vision system was used for operating these eyes. Hydrophobic acrylic foldable unifocal intraocular lens were implanted in the capsular bag [Figure 12], the residual viscoelastic was removed, intracameral preservative free moxifloxacin hydrochloride 0.5% solution was given, and the wounds were hydrated.
- Side port incision between 9 O clock and 10 O clock positions.

- Continuous curvilinear capsulorhexis.
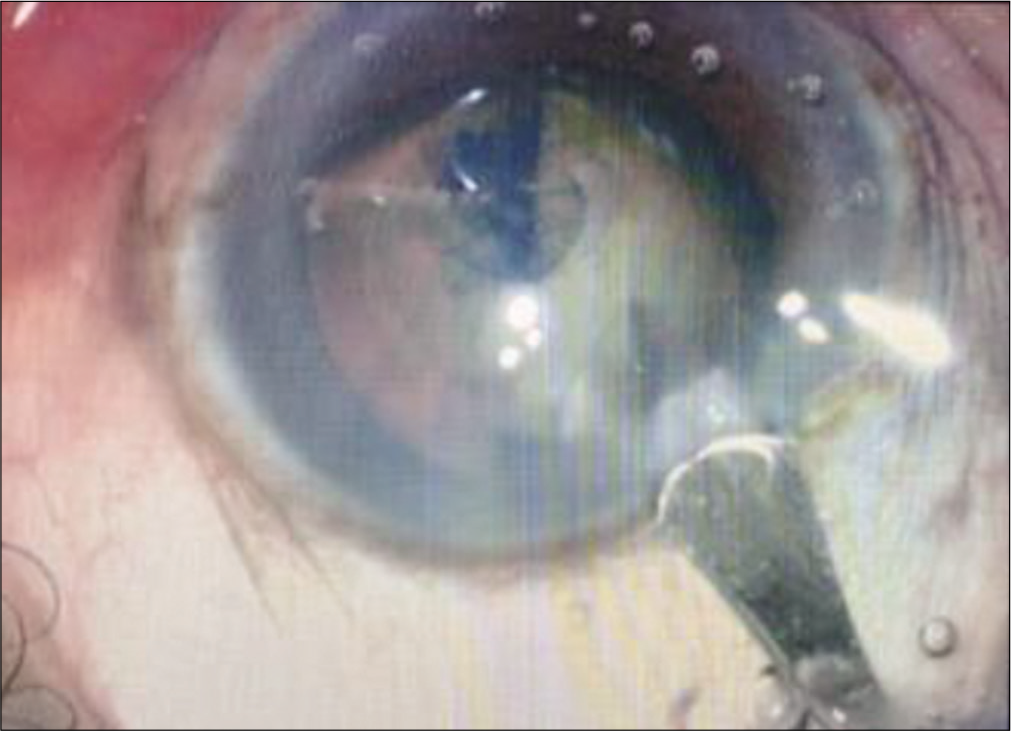
- Construction of the clear corneal main incision.

- Division of the nucleus.

- Aspiration of residual cortical matter.
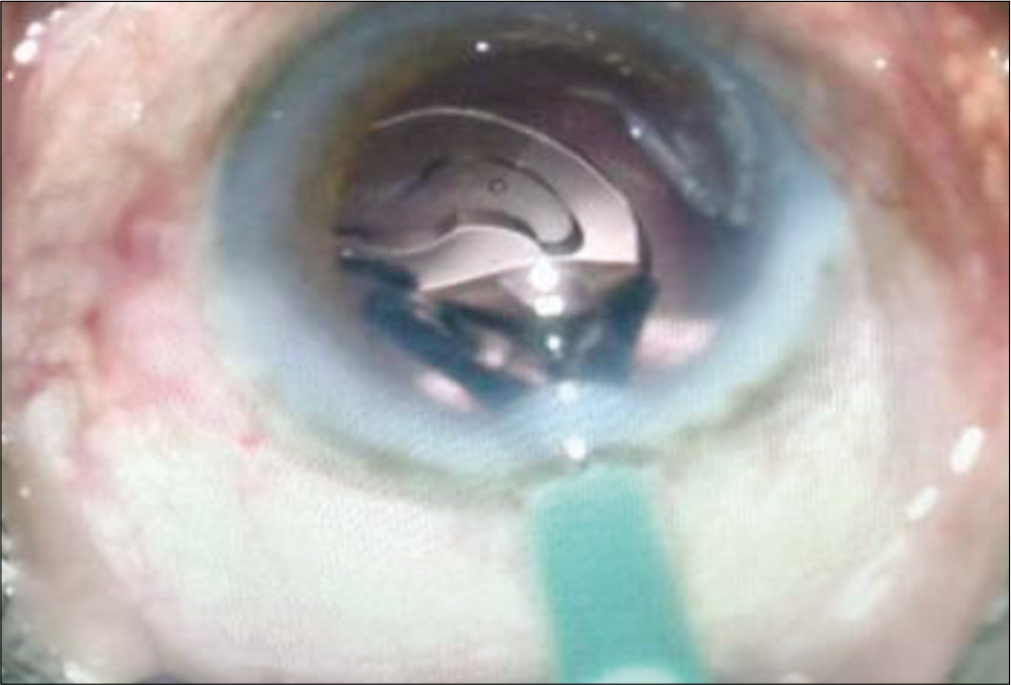
- Implantation of foldable intraocular lenses.
There were no intra-operative complications in both the study and control groups and patients were put on frequent topical preservative free moxifloxacin hydrochloride 0.5% + dexamethasone phosphate 0.1% which was gradually tapered over 5 weeks. Post-operative recovery was uneventful and complete ophthalmological evaluation was repeated at 6 weeks follow-up including unaided visual acuity, best corrected visual acuity, and keratometry readings using Zeiss IOLMaster.
RESULTS
Independent samples t-test was done to see for any statistically significant differences in the mean age, mean unaided visual acuity at 6 weeks follow-up measured in logMAR scale, average time taken for surgery, and mean surgical induced astigmatism between the two groups. Critical t was 1.9867 for P = 0.05.
DISCUSSION
Comparison of the calculated t and the critical t for the mean age in the two groups for p of 0.05 indicated that the two groups were matched for age. The mean ages of 48.23 + 2.60289 (SD) years in the study group and 48.84 + 2.91702 (SD) years in the control group also indicated that patients in both the study and control groups had eyes with earlier onset of cataract.[11] This also explains why these patients have softer cataracts of Grade 1 nuclear sclerosis.[12] The type of astigmatism presents in both groups were of “with-the-rule” pattern with the steeper corneal axis in the vertical meridian and the flatter axis in the horizontal meridian. This was in agreement with the results of several studies about “with-the-rule” astigmatism being more prevalent in younger age groups and astigmatism changing to “against-the-rule” pattern with advancing age due to changes in the cornea.[13,14]
There were 30 males out of 41 patients (73.17%) in the study group and 27 males out of 38 patients (71.05%) in the control group. At 6 weeks follow-up period, 41 eyes out of 47 eyes in the study group and 37 eyes out of 44 eyes in the control group had uncorrected visual acuity of 6/9 or better. These eyes had no need of corrective glasses for distant vision. The percentage of eyes not requiring corrective glasses for distant vision at 6 weeks follow-up was found to be marginally more in the study group (87.23%) than in the control group (84.09%). It may seem to indicate that the refractive results in the study group were as good as those in the control group, if not better. However, there was no significant difference in the mean visual acuity measured in logMAR scale at 6 weeks follow-up as shown by the calculated t value of –1.01171 against the critical t of 1.9867 for P of 0.05. Perhaps more studies with larger samples may be required to substantiate this. The mean surgical time was also found to be less in the study group.
The amount of surgical induced astigmatism measured in diopters as the sum total of the absolute amount of corneal flattening/decrease in K value in steeper vertical meridian plus and the absolute amount of corneal steepening/increase in K value in the flatter horizontal meridian was 0.81511 + 0.14663 (SD) in the study group and 0.43591 + 0.0588 (SD) in the control group, respectively. This difference was found to be statistically significant by the independent samples t-test. It shows that phacoemulsification produces less astigmatical changes and is an astigmatically neutral procedure. This is also in agreement with studies reported in literature.[15,16] However, it also meant that any significant corneal astigmatism in pre-operative period will continue to remain in the post-operative period along with the requirement of corrective glasses for distant vision.
The surgical induced astigmatism in the study group was found to neutralize any pre-existing “with-the-rule” corneal astigmatism in the range of 1.00–1.50 D, thereby reducing or eliminating the requirement for corrective glasses for distant vision in the post-operative period. In cases, where the preexisting corneal astigmatism was in the range of 0.50–1.00 D, this surgical induced astigmatism tended to overcorrect the pre-existing astigmatism and changing the pattern from “with-the-rule” to “against-the-rule” with the horizontal meridian now becoming steeper than the vertical meridian while the absolute value of the astigmatism did not differ much. These eyes also had either reduced requirement or no requirement of corrective glasses for distant vision in the post-operative period.
CONCLUSION
For eyes having soft cataracts of Grade 1 nuclear sclerosis and “with-the-rule” pattern of corneal astigmatism in younger age groups, the refractive results of superior quadrant approach sutureless scleral tunnel based extracapsular cataract surgery are as good as those of clear corneal based phacoemulsification surgery, if not better. Sutureless scleral tunnel based extracapsular cataract extraction was found to neutralize pre-existing corneal astigmatism if it was in range of 1.0–1.5 D. It was also found to change the pattern of astigmatism from “with-the-rule” to “against-the-rule” if it was in the range of 0.5–1.0 D with little change in the absolute value of the astigmatism. This resulted in reduced requirement or no requirement of corrective glasses for distant vision in the post-operative period for these eyes. Phacoemulsification, on the other hand, was found to be an astigmatically neutral surgery.
A more precise correlation between the length and pattern of the scleral based incision and amount of correction of pre-existing astigmatism will require more studies. And also most patients requiring cataract surgery in ophthalmological practice are of older age group, and most of them have “against-the-rule” pattern of astigmatism[17] and will require temporal based incisions to tackle it. Further studies will be required to see if a sutureless scleral tunnel based extracapsular cataract extraction with a temporal approach can reduce/eliminate this “against-the-rule” corneal astigmatism.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Cataract surgery for the developing world. Curr Opin Ophthalmol. 2008;19:55-9.
- [CrossRef] [PubMed] [Google Scholar]
- A prospective randomized clinical trial of phacoemulsification vs manual sutureless small-incision extracapsular surgery in Nepal. Am J Ophthalmol. 2007;143:1069. author reply 1069
- [CrossRef] [PubMed] [Google Scholar]
- Phacoemulsification versus manual small incision cataract surgery: Anatomic and functional results. J Fr Ophtalmol. 2017;40:460-6.
- [CrossRef] [PubMed] [Google Scholar]
- Post-operative residual astigmatism after cataract surgery: Current surgical methods of treatment. J Fr Ophtalmol. 2012;35:226-8.
- [CrossRef] [PubMed] [Google Scholar]
- Phaco-emulsification versus manual small-incision cataract surgery in South Africa. S Afr Med J. 2012;102:537-40.
- [CrossRef] [PubMed] [Google Scholar]
- Manual small incision cataract surgery (MSICS) with posterior chamber intraocular lens versus phacoemulsification with posterior chamber intraocular lens for age-related cataract. Cochrane Database Syst Rev. 2013;10:CD008813.
- [CrossRef] [PubMed] [Google Scholar]
- Surgically induced astigmatism in manual small-incision cataract surgery: A comparative study between superotemporal and temporal scleral incisions. TNAO J Ophthalmic Sci Res. 2019;57:105-8.
- [CrossRef] [Google Scholar]
- Clinical importance of the lens opacities classification system III (LOCS III) in phacoemulsification. Coll Antropol. 2005;29(Suppl 1):91-4.
- [Google Scholar]
- Epidemiologic study of age-related cataracts among an elderly Chinese population in Shih-Pai, Taiwan. Ophthalmology. 2003;110:1089-95.
- [CrossRef] [Google Scholar]
- Water content, lens hardness and cataract appearance. Eye (Lond). 1994;8:125-9.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of corneal astigmatism before cataract surgery in Caucasian patients. Eur J Ophthalmol. 2013;24:494-500.
- [CrossRef] [PubMed] [Google Scholar]
- Astigmatism prevalence and biometric analysis in normal population. Eur J Ophthalmol. 2013;23:779-83.
- [CrossRef] [PubMed] [Google Scholar]
- Astigmatic change induced by 2.8-mm corneal incisions for cataract surgery. Invest Ophthalmol Vis Sci. 2009;50:989-94.
- [CrossRef] [PubMed] [Google Scholar]
- Site of clear corneal incision in cataract surgery and its effects on surgically induced astigmatism. Sci Rep. 2020;10:3955.
- [CrossRef] [PubMed] [Google Scholar]
- Relationship between age, corneal astigmatism, and ocular dimensions with reference to astigmatism in eyes undergoing routine cataract surgery. Eye (Lond). 2016;30:562-9.
- [CrossRef] [PubMed] [Google Scholar]






