Translate this page into:
Autologous blood injection as a modality of the treatment of temporomandibular joints dislocation: A case report

*Corresponding author: Sobhan Mishra, Department of Oral and Maxillofacial Surgery, Institute of Dental Sciences, Bhubaneswar - 7510 03, Odisha, India. sobhan.surgeon@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Roy SS, Alam WM, Lenka S, Mishra S. Autologous blood injection as a modality of the treatment of temporomandibular joints dislocation: A case report. Indian J Med Sci 2021;73(1):117-20.
Abstract
Many specific surgical procedures have been identified for treating the dislocation of chronic recurrent temporomandibular joints (TMJs). This article addresses an autologous blood injection (ABI) procedure for the TMJ diagnosis of chronic recurrent TMJ dislocation. A 22-year-old patient reported with chronic TMJ dislocation for 3 months. Autologous blood was injected into upper joint space and surrounding pericapsular tissue under local anesthesia. The patient was followed up regularly. The treatment was successful and the patient had no more dislocation of TMJ as inferred from favorable improvement in mouth opening. Autologous blood infusion (ABI) within the articular capsule and/or pericapsular space or joint depression, is one of the most negligibly intrusive treatments methodology for repetitive separations of TMJ, was as of now presented.
Keywords
Temporomandibular joint dislocation
Autologous blood injection
Temporomandibular joint
Joint
INTRODUCTION
Temporomandibular joint (TMJ) is one of the most complex facial structures with diagnosis and management of its anomalies posing unique challenges. Dislocation of the TMJ is a condition which occurs when condyle moves and stays ahead of the eminence. Chronic dislocation of TMJ can happen even during daily activities such as laughing and yawning.[1,2] It might also happen after too much opening of the mouth while undergoing general anesthesia (GA) and dental treatment. Various surgical and non-surgical procedures have been used in the literature to treat patients with chronic dislocation of TMJ. Conservative methods[3,4] include limitation of mandibular movements, local anesthetic applications, injection of botulinum toxin into the mastication muscles (causes denervation of muscle that draws the chin down), and injection of sclerosing agents (tincture of iodine, alcohol, and sodium psylliate). Non-surgical methods of treatment are not always helpful; so, multiple surgical procedures, including capsular placation, reduction or increase of articular eminence, temporalis tendon scarification, lateral pterygoid myotomy, and condylectomy,[5] have been tried. Some clinicians[6,7] successfully treated cases of persistent TMJ dislocation with autologous blood in the TMJ in the past.
Brachmann in 1964 first reported autologous blood injection (ABI) as a modality of treatment of TMJ dislocation.[8] This treatment modality was reintroduced in 2001 by Hasson and Nahlieli.[9] In 2014, Oshiro et al. reviewed clinical and MRI fines after ABI for chronic TMJ dislocation therapy.[10] They found that ABI was minimally invasive, effective, and safe to treat. The concept behind ABI is to restrict mandibular movements by causing fibrosis in the upper joint area, pericapsular tissue, or both, by injecting blood into TMJ. The patient’s own blood is pumped into TMJ in this cautious process, thereby preventing the risk of an allergic reaction and post-operative infection. Machon et al.[11] and others have recently reintroduced the technique. The purpose of this study was to evaluate the infusion of ABI in the management for chronic TMJ dislocation.
TECHNIQUE
This procedure can be performed on local anesthesia (LA), LA along with sedation, or GA. The operating surgeon should physically define a path from the ear tragus to the angle of the eye after positioning the patient in the normal way. Along this axis is located the articular fossa (AF) point, 10 mm anterior to ear tragus and 2 mm lower than axis. The patient is given LA of the auriculotemporal nerve, and a 19-gauge needle is placed into the AF region. On injecting Marcaine 0.5%, 3 cc of saline is pumped, allowing the upper compartment to distend. The exact position of needle is indicated by forward (protrusive) placement of the mandible while injecting saline. “The nineteen-gauge needle stays in position AF, while 5 cc of blood is drained from the cubital fossa of the individual and the syringe is attached to the previously implanted needle and blood is injected – 4 cc in the upper compartment and 1 cc in surrounding pericapsular tissue. After that is applied an adhesive bandage and leaves for the 1st post-operative day. Individuals are advised to suppress their mandibular activity for 1 week after the operation.” Soft diet has been recommended for the same 7 days, and antibiotics with cephalosporin and anti-inflammatory nonsteroidal medications have been prescribed for a week. Mouth opening exercises were advised before the opening and normal excursive movements.[9]
CASE REPORT
A 22-year-old female patient reported with a complaint of lock jaw frequently for 3 months. While examining, the patient had initially mouth opening of 26 mm measured inter-incisal. There was slight deviation present on the left side while opening mouth. There was no clicking or popping sound present. No joint tenderness present.
The patient was made to seat on the dental chair at an angulation of 45°. The target site as prepared, scrubbed with betadine. From middle of tragus to outer canthus of eye, a straight line was made and points were noted on canthotragal line. A point 10 mm from the mid-tragus was marked and 2 mm below the line which corresponds to posterior superior joint cavity as mentioned above. Local anesthetic 2% lidocaine with vasoconstrictor was injected at marked entrance point near the pre auricular region. Using 5 ml syringe blood was drawn from the cubital vein and 3 ml was injected into joint space and 2 ml into the pericapsular tissue. Procedure was repeated bilaterally.
DISCUSSION
Dislocation/subluxation of TMJ happens when either one or both condylar head is displaced anterior to the articular eminence. It might be reduced when it comes back to temporomandibular fossa or might remain irreducible when one or more condyle remains displaced. In such cases, the role of masticatory (elevator) group of muscles with or without lateral divergence, the mouth presents an anterior open bite, depending on whether the dislocation is single sided or present on both sides. Acute mandibular dislocation is manually treated by moving the mandible downward, backward, and upward, to relocate the condyle into the temporomandibular fossa. When this occurs spontaneously, it is termed as chronic TMJ dislocation. Pathogenesis includes a variety of reasons such as laxity of TMJ, weakening of capsule (TMJ),[12] an abnormal projection of articular eminence, muscle spasms/hyperactivity, trauma, and unusual chewing movements which does not facilitate the backward translation of head of the condyle. Repeated dislocation causes damage to articular disc, the joint capsule, and ligaments lending to internal derangement of TMJ.
Brachmann et al. treated 60 patients successfully by injecting autologous blood into the TMJs.[8] In the year 1973, Schulz treated 16 patients injecting autologous blood in the affected TMJ, 2 times weekly for a continuous period of 3 weeks preceded by immobilization using intermaxillary fixation (IMF) for 4 weeks.[6] He stated that in 1-year review, 10 individuals were symptomless. Jacobbi-Hermanns[7] in the year 1981 stated her findings with 19 patients who given only a single ABI and had undergone IMF for the next 2 weeks. After a follow-up period of 18 months, 17 patients were good and also symptom free. At present, Hasson[9] presented case scenarios of successful treatment of three patients. Kato et al.[13] also treated one of their patients successfully using ABI.
Injecting blood into the TMJ follows the mechanism of bleeding in joints like various other parts in the body, for example, the elbow or knee joint. Primarily, the joint capsule and its surrounding tissues of periarticular region are expanded by the injected blood. An inflammatory reaction occurs within a few hours or days which lead to release of inflammatory mediators from the injured and dead cells, platelets which ultimately result in dilation of adjacent blood vessels and plasma leakage. This causes swelling of the remaining surrounding structures and tissues, and the swelling makes the movement of the joint difficult thus causes decrease in patient’s complaint. The blood clot and loose fibrous tissue formed, help to maintain the firmness of joint. In the end, maturation of this tissue occurs causing a permanent restricted movement of joint.[14] Moreover, this exposure of blood to cartilage leads to cartilage matrix turnover disruption and reduction in chondrocyte metabolism and ultimately results in localized contraction. However, after a traumatic injury to the TMJ, mouth opening exercises/ physiotherapy is practiced to prevent the accumulation of inflammatory mediators within the joint, which is in contrast to the cases of deliberate hemarthrosis. The blood which is injected in the artificially created wound leads to an inflammatory reaction, which further proceeds to fibrosis and adhesion of joint space. The end result is scarring of joint and in the adjacent soft tissue leading to mandible immobilization to avoid early stretching of newly developed fibrous tissue.[7] Those contraindicating this theory assume that even a minor exposure of cartilage to the intra-articular blood may lead to permanent joint destruction,[15] such as degenerative joint damage,[16] cartilage degeneration, and apoptosis,[17] of which joint destruction may eventually continue.
Injecting autologous blood in the management of recurrent TMJ dislocation was found efficacious. Since there is no dissection of tissue, post-operative complications such as facial nerve palsy, altered sensation (dysesthesia), inflammation, any kind of infection, and pain which subsequently reduces and becomes non-existent.[11]
The patient came back for review during the 1st week, 2nd week, and after 3 months with a maximum inter-incisal opening of 33 mm with no complaint of dislocation [Figure 1].
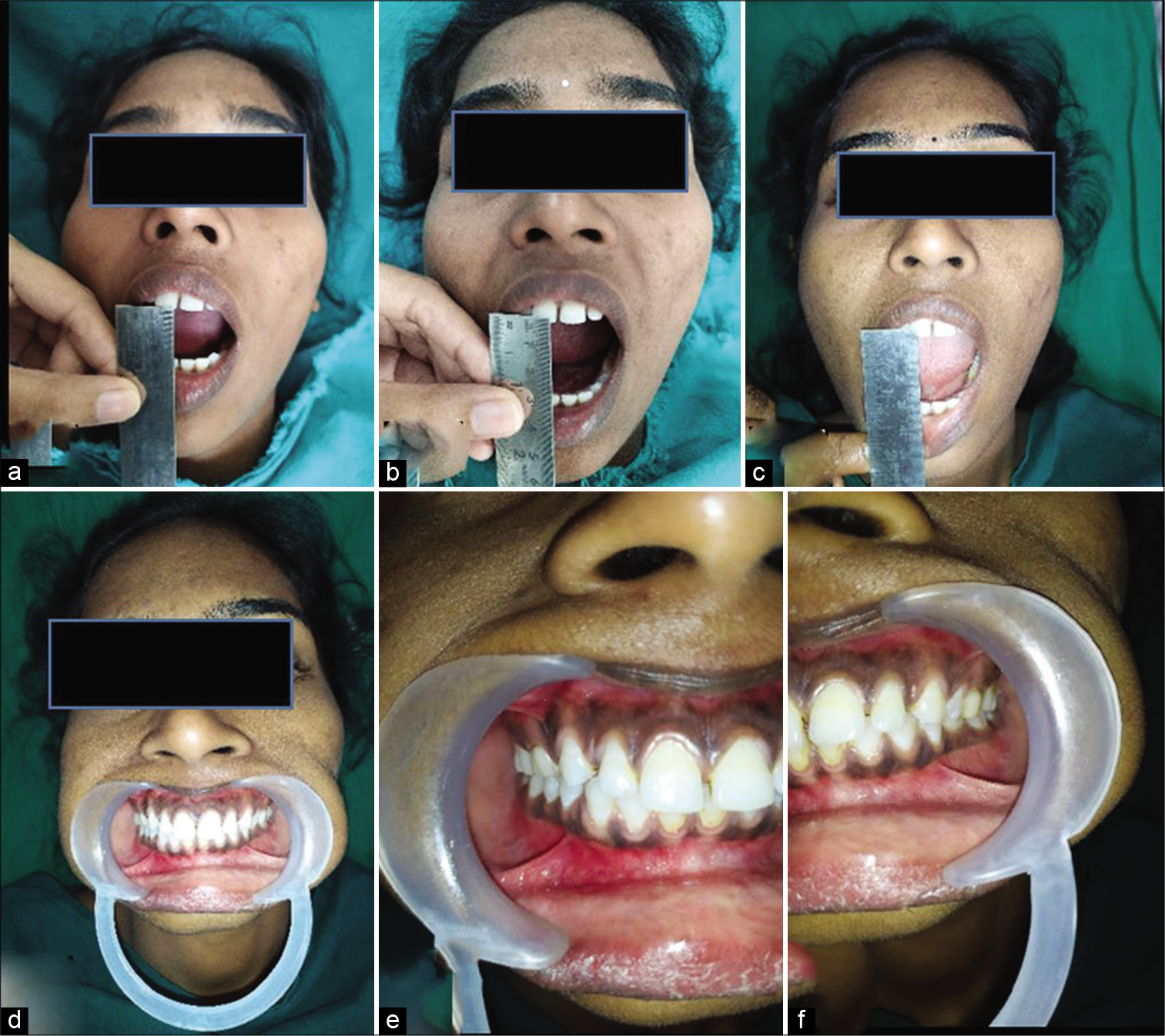
- Post-operative. Maximum inter-incisal opening (a) 1st week: 26 mm, (b) 2nd week: 29 mm, (c) 3rd month: 32 mm, (d-f) no occlusal discrepancy present.
CONCLUSION
This technique of injecting autologous blood to the TMJ is an effortless, secured, and inexpensive procedure helpful in treating 80% of patients with recurrent TMJ dislocation successfully. The operating surgeon is advised and motivated to perform this procedure when the individual comes with a history of chronic recurrent TMJ dislocation, before going for an invasive surgical technique.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Randomized effectiveness study of four therapeutic strategies for TMJ closed lock. J Dent Res. 2007;86:58-63.
- [CrossRef] [PubMed] [Google Scholar]
- Pre-and posttreatment analysis of clinical symptoms of patients with temporomandibular disorders. Quintessence Int. 2004;35:811-4.
- [Google Scholar]
- Reduction of a chronic bilateral temporomandibular joint dislocation with intermaxillary fixation and botulinum toxin A. Br J Oral Maxillofac Surg. 2004;42:272-3.
- [CrossRef] [PubMed] [Google Scholar]
- OK-432 (picibanil) Sclerotherapy for recurrent dislocation of the temporomandibular joint in elderly edentulous patients: Case reports. Br J Oral Maxillofac Surg. 2007;45:511-3.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical reconstruction of the temporomandibular joint for chronic subluxation and dislocation. Int J Oral Maxillofac Surg. 2001;30:344-8.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of periarticular autotransfusion for therapy of recurrent dislocations of the temporomandibular joint. Dtsch Stomatol. 1973;23:94-8.
- [Google Scholar]
- Pericapsular autologous blood injection as therapy for habitual temporomandibular joint luxation. Dtsch Zahnarztl Z. 1981;36:187-90.
- [Google Scholar]
- Autologous blood injection for recurrent hypermobility of the temporomandibular joint. Dtsch Zahnarztl Z. 1964;15:97-102.
- [Google Scholar]
- Autologous blood injection for treatment of recurrent temporomandibular joint dislocation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:390-3.
- [CrossRef] [PubMed] [Google Scholar]
- Analysis of MRI findings in minimum invasive treatment for habitual temporomandibular joint dislocation by autologous blood injection around the temporomandibular joint capsule. J Craniomaxillofac Surg. 2014;42:1486-90.
- [CrossRef] [PubMed] [Google Scholar]
- Autologous blood injection for the treatment of chronic recurrent temporomandibular joint dislocation. J Oral Maxillofac Surg. 2009;67:114-9.
- [CrossRef] [PubMed] [Google Scholar]
- Temporomandibular joint “open lock” versus condylar dislocation: Signs and symptoms, imaging, treatment, and pathogenesis. J Oral Maxillofac Surg. 2002;60:506-11.
- [CrossRef] [PubMed] [Google Scholar]
- Autologous blood injection into the articular cavity for the treatment of recurrent temporomandibular joint dislocation: A case report. J Oral Sci. 2007;49:237-9.
- [CrossRef] [PubMed] [Google Scholar]
- Continuous passive motion (CPM): Theory and principles of clinical application. J Rehabil Res Dev. 2003;37:179-88.
- [Google Scholar]
- Blood-induced joint damage: Longterm effects in vitro and in vivo. J Rheumatol. 2003;30:339-44.
- [Google Scholar]
- Initiation of degenerative joint damage by experimental bleeding combined with loading of the joint: A possible mechanism of hemophilic arthropathy. Arthritis Rheum. 2004;50:2024-31.
- [CrossRef] [PubMed] [Google Scholar]
- Short-term exposure of cartilage to blood results in chondrocyte apoptosis. Am J Pathol. 2003;162:943-51.
- [CrossRef] [Google Scholar]






