Translate this page into:
Cardiovascular disease burden and associated risk factors in chronic kidney disease
*Corresponding author: Roshan Bhandari, Department of Cardiovascular Medicine, Hiroshima University Hospital/Hiroshima University Graduate School of Biomedical and Health Sciences, Hiroshima, Japan. bhandariroshan369@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bhandari R, Pantha S, Pandey G, Paudyal R. Cardiovascular disease burden and associated risk factors in chronic kidney disease. Indian J Med Sci. doi: 10.25259/IJMS_289_2024
Abstract
Objectives
Cardiovascular disease (CVD) is regarded as a leading cause of premature mortality and morbidity among individuals with chronic kidney disease (CKD). There is a high burden of cardiovascular complications in CKD patients, necessitating an integrated approach for targeted management of cardiovascular complications among CKD patients. The objective of this study was to evaluate the prevalence, nature, and risk factors of cardiovascular complications among CKD patients in a tertiary care center in Nepal.
Materials and Methods
It is a prospective and cross-sectional study conducted for 1 year (April 2020–2021). We recruited a total of 60 patients, meeting the criteria. Comprehensive patient histories, thorough physical examinations, potential risk factors for cardiovascular complications, echocardiographic, and laboratory data were collected. Statistical analysis was performed using the Statistical Package for the Social Sciences version 25.
Results
Among all, the predominant cardiovascular complication was valvular heart disease (VHD) (71.67%), with mitral regurgitation being the most prevalent (58.33%). Other complications included left ventricular diastolic dysfunction (66.67%), left ventricular hypertrophy (LVH) (53.33%), left ventricular systolic dysfunction (21.67%), pericardial effusion (15.00%), and global hypokinesia (11.67%). Significant comorbidities included anemia (100%), hypertension (HTN) (91.67%), diabetes mellitus (DM) (56.67%), and dyslipidemia (58.33%). Notably, 40.00% were smokers, 38.33% reported alcohol consumption, 21.67% were obese, and 13.33% were underweight.
Conclusion
Our study highlights the substantial impact of cardiovascular complications among CKD patients in Nepal. We found that VHD and LVH are particularly prevalent, underscoring the urgent need for early detection and targeted management strategies in clinical practice. The strong association with common comorbidities such as anemia, HTN, DM, and dyslipidemia further emphasizes the intricate relationship between renal and cardiovascular health in this population. Thus, these findings provide valuable insights into the cardiovascular and general healthcare challenges faced by CKD patients in our setting, urging for integrated care approaches to improve outcomes and enhance patient care.
Keywords
Cardiovascular diseases
Chronic kidney disease
Echocardiography
Valvular heart disease
INTRODUCTION
Cardiovascular disease (CVD) is regarded as a leading cause of premature mortality and morbidity among individuals with chronic kidney disease (CKD).[1] The global prevalence of CKD is estimated to be 13.4% (ranging from 11.7% to 15.1%).[2] CVD, rather than end-stage kidney disease (CKD stage 5), is the leading cause of death in this high-risk population.[3] In the early stages of CKD, traditional risk factors for CVD play a significant role. However, in the intermediate and late stages, non-traditional risk factors become more prominent. These include iso-osmotic and non-osmotic sodium retention, volume expansion, anemia, inflammation, malnutrition, sympathetic overactivity, mineral bone disorders, the buildup of uremic toxins, and hormonal imbalances, all of which contribute to the accelerated progression of CVD in these patients.[4] The combination of CVD risk factors is linked to a higher prevalence of ventricular hypertrophy, myocardial fibrosis, valvopathy, arrhythmias, and an increased risk of sudden death.[5,6]
In Nepal, there is a growing prevalence of CKD, with its share of total disability-adjusted life years rising from 0.5% [95% Uncertainty Interval (UI): 0.4, 0.6] in 1990 to 1.8% (95% UI: 1.4, 2.2%) in 2019.[7] Our study aimed to evaluate the prevalence, nature, and risk factors of cardiovascular complications among CKD patients, highlighting the disproportionate burden of CVD in this population and addressing the significant gap in clinical research focused on CKD patients in cardiovascular studies within a developing country context.
The general objective of the study was as follows: To assess the prevalence, nature, and risk factors associated with cardiovascular complications among CKD patients in a tertiary care center. While the specific objectives were: (i) To assess the prevalence of specific cardiovascular complications, including structural and functional heart diseases using echocardiography, in the CKD patients; (ii). To identify and analyze the risk factors contributing to cardiovascular complications in CKD patients, including hypertension (HTN), diabetes mellitus (DM), anemia, obesity, alcohol consumption, dyslipidemia, and smoking; (iii). To explore the demographic, clinical, and laboratory profiles of the patients; and (iv) To measure the association between cardiovascular complications and common comorbidities in the CKD patients.
MATERIALS AND METHODS
This is a quantitative, prospective, and cross-sectional study conducted in the Department of Internal Medicine (Cardiology and Nephrology outpatient/inpatient departments) at Chitwan Medical College (CMC)-Teaching Hospital, Nepal, over 1 year (April 2020– 2021).
Patients’ consent and ethical approval
Ethical clearance was obtained from the Institutional Review Committee of CMC -Teaching Hospital before starting the study, and informed written consent was obtained from all enrolled patients.
Inclusion criteria
(i) Patients diagnosed with CKD based on the diagnosis and staging as per Kidney Disease Improving Global Outcomes (KDIGO);[8] and (ii) patients aged 18 years old and more.
Exclusion criteria
(i) Patients who were already diagnosed to have heart diseases such as – rheumatic heart disease, myocarditis, and cardiomyopathies; (ii) patients who did not give written consent for the study; and (iii) critically-ill patients.
Sampling
We enrolled 60 patients undergoing treatment at various stages of CKD. Participants were selected through non-probability purposive sampling, using a 6% CKD prevalence rate in Nepal from a previous study,[9] with a 95% confidence interval and a 5% margin of error.
Data collection and analysis
Comprehensive patient histories, thorough physical examinations, and echocardiographic and laboratory data were recorded using a standard pro forma. We also gathered information on potential risk factors for cardiovascular complications. The collected data were analyzed to determine the prevalence, nature, and risk factors of cardiovascular complications, as well as their correlations with various definable factors. Statistical analysis was performed using the Statistical Package for the Social Sciences version 25, employing descriptive characteristics such as frequency, percentage, central tendency, and dispersion. Association between variables was studied using Chi-square test or fisher exact test at 5% level of significance.
RESULTS
Total 60 patients were recruited for the study over a 1-year period, among which 56.67% were male. Their mean age was 45.23 ± 10.5 (25–65). Table 1 shows the baseline characteristics of the study population, and associated risk factors. Among all participants [Figure 1], the predominant cardiovascular complication was valvular heart disease (VHD) (71.67%), with mitral regurgitation being the most prevalent (58.33%). Other common complications included left ventricular diastolic dysfunction (LVDD) (66.67%), left ventricular hypertrophy (LVH) (53.33%), left ventricular systolic dysfunction (LVSD) (21.67%), pericardial effusion (15.00%), and global hypokinesia (11.67%). Significant comorbidities included anemia (100%), HTN (91.67%), DM (56.67%), and dyslipidemia (58.33%). Notably, 40.00% were smokers, 38.33% reported alcohol consumption, 21.67% were obese, and 13.33% were underweight. VHD was most prevalent among patients with dyslipidemia (85.71%), while LVDD was notably higher in smokers (83.33%). Mitral regurgitation showed a slight increase in prevalence among those with obesity (61.54%), and LVSD was consistently lower compared to other comorbidities. The detailed analysis of cardiovascular comorbidities revealing distinct patterns associated with various risk factors is shown in Table 2, while Table 3 shows the important investigation findings among the patients.
| Baseline characteristics | Total (n=60) | Male (n=34) | Female (n=26) | P-value |
|---|---|---|---|---|
| Age (years) | 45.23±10.5 | 46.12±9.8 | 44.05±11.2 | 0.15 |
| Height (inches) | 59.35±3.5 | 60.12±3.1 | 58.23±3.8 | 0.02 |
| Weight (kgs) | 51.66±5.2 | 52.45±4.8 | 50.32±5.6 | 0.05 |
| Risk factors (%) | ||||
| HTN | 55 (91.67) | 31 (91.18) | 24 (92.31) | 0.87 |
| DM | 34 (56.67) | 19 (55.88) | 15 (57.69) | 0.82 |
| Smokers | 24 (40.00) | 18 (52.94) | 6 (23.08) | 0.01 |
| Alcohol consumption | 23 (38.33) | 17 (50.00) | 6 (23.08) | 0.03 |
| Obesity | 13 (21.67) | 8 (23.53) | 5 (19.23) | 0.65 |
| Underweight | 8 (13.33) | 2 (5.88) | 6 (23.08) | 0.04 |
| Dyslipidemia | 35 (58.33) | 20 (58.82) | 15 (57.69) | 0.92 |
HTN: Hypertension, DM: Diabetes mellitus, CKD: Chronic kidney disease, CMC: Chitwan Medical College
| Cardiovascular Comorbidities | Total (n=60) (%) | HTN (n=55) (%) | DM (n=34) (%) | Smokers (n=24) (%) | Alcohol (n=23) (%) | Obese (n=13) (%) | Underweight (n=8) (%) | Dyslipidemia (n=35) (%) |
|---|---|---|---|---|---|---|---|---|
| VHD | 43 (71.67) | 39 (70.91) | 27 (79.41) | 19 (79.17) | 17 (73.91) | 10 (76.92) | 6 (75.00) | 30 (85.71) |
| LVDD | 40 (66.67) | 37 (67.27) | 26 (76.47) | 20 (83.33) | 18 (78.26) | 10 (76.92) | 5 (62.50) | 28 (80.00) |
| LVH | 32 (53.33) | 30 (54.55) | 21 (61.76) | 15 (62.50) | 14 (60.87) | 8 (61.54) | 5 (62.50) | 22 (62.86) |
| LVSD | 13 (21.67) | 12 (21.82) | 8 (23.53) | 5 (20.83) | 5 (21.74) | 3 (23.08) | 2 (25.00) | 8 (22.86) |
| Pericardial effusion | 9 (15.00) | 8 (14.55) | 6 (17.65) | 4 (16.67) | 4 (17.39) | 2 (15.38) | 1 (12.50) | 6 (17.14) |
| Global hypokinesia | 7 (11.67) | 6 (10.91) | 4 (11.76) | 3 (12.50) | 3 (13.04) | 2 (15.38) | 1 (12.50) | 5 (14.29) |
VHD: Valvular heart disease, LVDD: Ventricular diastolic dysfunction, LVH: Left ventricular hypertrophy, LVSD: Left ventricular systolic dysfunction, CKD: Chronic kidney disease, CMC: Chitwan Medical College
| Variables | Central tendency | Min/Max | P-value |
|---|---|---|---|
| Hemoglobin | Mean±SD=7.54±1.25 | 4.2/10.5 | 0.921 |
| Total leucocyte count | Median (IQR)=5900 (3600) | 1600/19000 | <0.001 |
| Platelet | Mean±SD=192000±67000 | 53000/370000 | 0.645 |
| Serum urea | Mean±SD=138.4±48.25 | 55.0/270 | 0.215 |
| Serum creatinine | Median (IQR)=9.85 (5.50) | 2.50/24.00 | 0.008 |
| Serum calcium | Median (IQR)=8.05 (1.40) | 6.90/10.00 | 0.014 |
| Serum phosphorus | Mean±SD=5.03±1.30 | 2.10/8.00 | 0.270 |
(IQR denotes interquartile range), CKD: Chronic kidney disease, CMC: Chitwan Medical College, SD: Standard deviation
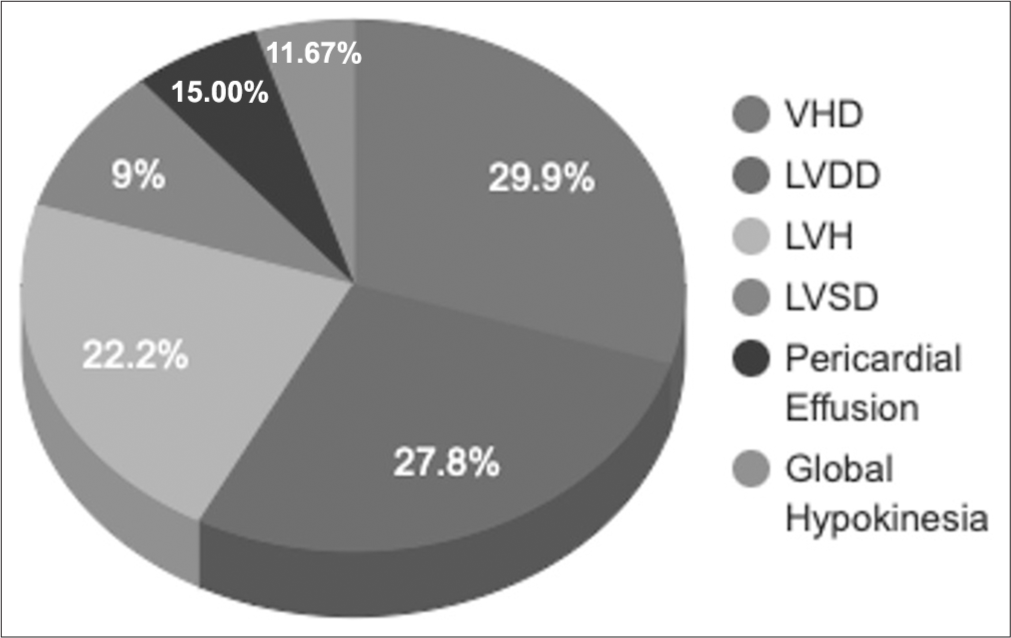
- Cardiovascular complications in the chronic kidney disease patients at Chitwan Medical College-teaching hospital. VHD: Valvular heart disease, LVDD: Ventricular diastolic dysfunction, LVH: Left ventricular hypertrophy, LVSD: Left ventricular systolic dysfunction.
DISCUSSION
Our study provides important insights into the prevalence and characteristics of cardiovascular complications in patients with CKD in Nepal. It emphasizes the significant burden of CVD in this population. These findings highlight the importance of integrating cardiovascular care in the management of CKD.
The main cardiovascular complication observed was VHD, which affected 71.67% of patients. This finding is consistent with other studies that reported a high prevalence of VHD in patients with CKD due to increased calcium accumulation and hemodynamic changes associated with kidney dysfunction.[10] It was also established that mitral regurgitation was very high, as would be expected from previous studies, which have concluded that mitral regurgitation is a common incidence of CKD patients due to progressive calcification of the heart valves.[11]
Meanwhile, 66.67% of the patients had LVDD, indicating that the disease prevalence is very high in CKD patients. Indeed, it is very common to have LVDD in CKD due to the associated fluid overload and HTN, all of which together increase the left ventricular mass.[12] Furthermore, LVH was observed in 53.33% of the patients in the present study, which is a well-established case in CKD secondary to the effects of HTN and volume overload.[13] About 91.67% of our study population were hypertensive.
Interestingly, LVSD was seen in 21.67% of the patients, and this is a bit on the lower scale compared to other complications. This could be so because LVSD often appears later in the course of CKD, or association with other underlying conditions.[14] The prevalence of pericardial effusion was 15.00%, and global hypokinesia was 11.67%, further indicating how multifaceted cardiovascular complications can be in CKD, thus reflecting the interrelationship that exists between kidney dysfunction and heart disease.
Our study also reflects strong associations of cardiovascular complications with common comorbidities and risk factors. For example, VHD was highest in dyslipidemic patients at 85.71%, while LVDD was significantly higher in smokers at 83.33%. These results are in consonance with previous literature in which dyslipidemia and smoking have been found to be major aggravating factors for cardiovascular health in CKD patients.[15,16] In addition, high levels of lipids contribute to endothelial dysfunction and increased CVD risk in CKD.[15] The significant association between obesity and cardiovascular complications underscores the impact of obesity on cardiac structure and function, as supported by previous studies.[17]
These findings are also complemented quite well by the descriptive analysis of our laboratory findings. Our study showed that there is a very high prevalence in anemia of CKD patients (100%). Its impact on cardiovascular health aligns well with the previous studies that reported that anemia makes significant contributions to cardiovascular morbidity in CKD patients.[18] Furthermore, high values of serum creatinine and altered values of serum calcium reveal the degree of renal impairment and the influence on cardiovascular status, as is evident in similar prior studies.[19,20]
DM was present in 56.67% of the patients and was significantly associated with cardiovascular complications. Specifically, DM was found to be a contributing factor to both VHD and LVDD. The association between diabetes and cardiovascular complications is well-established as hyperglycemia exacerbates endothelial damage and accelerates CVD progression in CKD patients.[21] Diabetes-induced glycation of proteins and increased oxidative stress contribute to both structural and functional cardiovascular abnormalities.[22,23]
CONCLUSION
Our study highlighted the high burden of cardiovascular complications in CKD patients in Nepal. There is an urgent need for targeted management of cardiovascular complications among CKD patients, as high proportions of VHD, left ventricular dysfunction, and other complications have come into view. Strong associations with HTN, DM, dyslipidemia, smoking, alcohol consumption, and anemia further emphasize effective management of these risk factors in this population. These findings highlight that early detection and comprehensive management strategies regarding cardiovascular and renal issues among patients with CKD are highly essential. Longitudinal studies are essential to further investigate the development of CVD across the spectrum of CKD and determine the effect of different approaches to management.
Ethical approval
The research/study approved by the Institutional Review Board at Institutional Review Committee of Chitwan Medical College-Teaching Hospital (CMC-IRC), number 133712078179, dated April 01, 2020.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Cardiovascular risk factors in pre-dialysis chronic kidney disease patients of Nepal. J Adv Intern Med. 2020;9:47-53.
- [CrossRef] [Google Scholar]
- Prevalence and disease burden of chronic kidney disease. Adv Exp Med Biol. 2019;1165:3-15.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiovascular complications in chronic kidney disease: A review from the European Renal and Cardiovascular Medicine Working Group of the European Renal Association. Cardiovasc Res. 2023;119:2017-32.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiovascular risk factor profiles and kidney function stage in the US general population: The NHANES III study. Mayo Clin Proc. 2005;80:1270-7.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiovascular disease in chronic kidney disease. Indian J Nephrol. 2005;15:1-7.
- [CrossRef] [Google Scholar]
- Cardiovascular disease in chronic kidney disease: Pathophysiological insights and therapeutic options. Circulation. 2021;143:1157-72.
- [CrossRef] [PubMed] [Google Scholar]
- Burden of chronic kidney disease in Nepal: An analysis of the burden of disease from 1990 to 2019. PLOS Glob Public Health. 2023;3:e0001727.
- [CrossRef] [PubMed] [Google Scholar]
- KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;3:1-150.
- [Google Scholar]
- Prevalence and risk factors associated with chronic kidney disease in Nepal: Evidence from a nationally representative population-based cross-sectional study. BMJ Open. 2022;12:e057509.
- [CrossRef] [PubMed] [Google Scholar]
- Valvular heart disease in patients with chronic kidney disease. Eur Cardiol. 2022;17:e02.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic kidney disease and valvular heart disease: Conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kidney Int. 2019;96:836-49.
- [CrossRef] [PubMed] [Google Scholar]
- Left ventricular diastolic dysfunction in chronic kidney disease patients not treated with dialysis. Nutrients. 2022;14:4664.
- [CrossRef] [PubMed] [Google Scholar]
- Left ventricular hypertrophy in chronic kidney disease patients: From pathophysiology to treatment. Cardiorenal Med. 2015;5:254-66.
- [CrossRef] [PubMed] [Google Scholar]
- Study of left ventricular systolic dysfunction, left ventricular diastolic dysfunction and pulmonary hypertension in CKD 3b-5ND patients-A single centre cross-sectional study. Nefrologia (Engl Ed). 2023;43:596-605.
- [CrossRef] [PubMed] [Google Scholar]
- Dyslipidemia in patients with chronic kidney disease: An updated overview. Diabetes Metab J. 2023;47:612-29.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of smoking on cardiovascular outcomes in patients with stable coronary artery disease. Eur J Prev Cardiol. 2021;28:1460-6.
- [CrossRef] [PubMed] [Google Scholar]
- Obesity-related kidney disease: Beyond hypertension and insulin-resistance. Front Endocrinol (Lausanne). 2023;13:1095211.
- [CrossRef] [PubMed] [Google Scholar]
- Anemia in chronic kidney disease: From pathophysiology and current treatments, to future agents. Front Med (Lausanne). 2021;8:642296.
- [CrossRef] [PubMed] [Google Scholar]
- Serum creatinine concentration and risk of cardiovascular disease: A possible marker for increased risk of stroke. Stroke. 1997;28:557-63.
- [CrossRef] [PubMed] [Google Scholar]
- Calcium as a cardiovascular toxin in CKD-MBD. Bone. 2017;100:94-9.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiovascular disease in diabetes and chronic kidney disease. J Clin Med. 2023;12:6984.
- [CrossRef] [PubMed] [Google Scholar]
- Diabetic cardiovascular disease induced by oxidative stress. Int J Mol Sci. 2015;16:25234-63.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic kidney disease, diabetes mellitus and cardiovascular disease: Risks and commonalities. J Ren Care. 2012;38:4-11.
- [CrossRef] [PubMed] [Google Scholar]






