Translate this page into:
Community care for COVID-19 in the constraint resources is the need of the hour to provide health facility to the last man of the queue

*Corresponding author: Anil Kumar, Department of Trauma and Emergency, Type- 5, Block-2, Flat No-104, AIIMS Residential Complex, Hydraulic Road, Opposite to WALMI, Phulwarisharif (Danapur), Patna - 801 105, Bihar, India. Mobile: +91-9835699103. dranil4@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kumar A. Community care for COVID-19 in the constraint resources is the need of the hour to provide health facility to the last man of the queue. Indian J Med Sci 2021;73(1):52-6.
Abstract
In COVID era, the developing countries like India are facing big problems and fail to provide health care to needy patients. The main reason for this failure is limited health resources and overpopulated states. Considering these, it is need of the hour to establish community care for COVID-19 in every district. The trained health worker will be instrumental in categorizing COVID-positive patients in three different zones that are green, yellow, or red on the basis of mild, moderate, or severe clinical symptoms, respectively. All such patients may be treated under the guidance of doctors of the telemedicine department of the tertiary center with close monitoring under CCTV camera and other telemedicine software. The only limitation of this model is that we need to shift sick patients (red) to higher center. The estimated cost is approximately 2,29,000 only to establish one center.
Keywords
COVID-19
Community care
Health facility
Last man of the queue
INTRODUCTION
In the last few weeks, the number of corona infected patients has increased very rapidly.[1-3] On the other hand, the health facility and available beds in the hospital are not sufficient.[4,5] The patients and their relatives are wandering here and there to get a bed in the hospital but with little success. Only few hospitals are admitting the patients of corona and, in fact, are unable to accommodate and provide quality care to the needy patients. The government of India was initiated several types of actions to control the spread of coronaviruses.[3]
In this pandemic situation, it is required to frame some innovative models for state, where resources are limited and number of patients is more. Considering all these, our institute took a small initiative as a pilot project to make a model to categorize the COVID-positive patients into three categories as red, yellow, and green-like trauma triage.[6] In this model, all corona-positive patients are classified into three categories on the basis of the extent of symptoms, whether he/she has mild/no symptoms, moderate, or severe symptoms. A training program has been framed for common people as well as health workers to strengthen this model to provide treatment for green and yellow category patients at their home and community, respectively. The training program and advice for patients of home quarantine may be considered by telemedicine.[7]
The limitation of this model is that red patients are required to shift to tertiary center because such patients may require ventilator and ICU management.
Objective
The objective of this study was to provide the greatest benefit for the maximum number of people at their doorstep. This will also avoid unnecessary overload at the tertiary center in view to maintain social distance as well as keep the resources reserved at the tertiary center for the sick patients who require ICU management.
RESOURCES AND WORKFORCE
The resources and workforce required for one center are as follows:
First, we need a space of 1500 square feet for each center with a facility of water, electricity, and toilet. Any community center, marriage hall, school, college, Panchayat Bhavan, or available space (personal) may be identified to start the center.
For each center, there will be a requirement of 10 beds, mattresses, bedsheets, side tables, oxygen cylinders, flow meters, oxygen masks, spo2 probes, IV Stands, thermometers, and BP measuring machines.
Biomedical disposal bins.
CCTV with four cameras.
Personal protective equipment and medicines as per requirement.
WORKFORCE AND TRAINING
We can identify the trained health workers such as telemedicine operator, ASHA worker, local compounder, paramedical staff, doctors, or volunteers. Identified persons will work under the control of district administration and doctor of medical colleges or tertiary centers. The medical colleges will give training to identify person regarding the following areas:
How to assess the patient clinically?
How to wear PPE and take universal precautions (Donning and doffing)?
How to measure their vitals, including pulse, BP, and oxygen saturation with the help of saturation probe?
What is the normal limit of these parameters and what to do in case of any abnormality?
What are the different medications which should be prescribed by doctors through telemedicine and how to instruct to follow the given advice at patient’s end?
How to give oxygen therapy in case of SPO2 <94% on room air?
How to regulate the inflow of oxygen by a flow meter and assess the saturation?
How to categorize COVID-positive patients in mild, moderate, and severe categories to isolate in green, yellow, and red zone?
How to identify a critical patient who should be kept in the red zone just by assessing the saturation level?
What should be the next step in shifting such critical patients if their saturation is not improving even after flow of oxygen at the rate of 15 L/min?
All these skills can be learned through video conference or by already made video which is available on Google/YouTube by the name of “Community care for COVID-19.” For any doubt or help, the person can talk to telemedicine team of medical colleges round-the-clock. Our resource person will also become an expert in triaging the patients in three categories and they will identify the stable patients who have tested positive for COVID and counsel such patients for home isolation after consulting the doctors of medical colleges. They will also liaison with the transport of sick (red) to a higher center.
FINANCIAL IMPLICATIONS
The expected cost of drugs including hydroxychloroquine, azithromycin 500 mg, tab paracetamol, injection low molecular weight heparin 40 mg, and tab dexamethasone 6 mg for each patient would be Rs. 3,500, and for total of 30 patients (expected numbers to be admitted in 1 month) would be Rs. 105000 (one lakh five thousand), and cost for PPE would be Rs. 24,000. Hence, total expected cost to establish one center is Rs 229,000 only including 100,000 for fixture and 129,000 for consumable (PPE and drugs) for 30 patients. The financial help to establish these centers may be arranged with the help of either Bihar Government or Government of India or both after a proper meeting to make a concrete policy to sustain this model as a robust program.[8]
TREATMENT PROTOCOL AS PER CATEGORY
The COVID-positive patient with no/mild clinical symptoms comes under the green category. The patient of such category needs either observation at a community center or home isolation with specific general instructions like maintain social distance, do not greet by handshakes, use alcohol-based hand rub with >60%, betadine mouth gargle, eat nutritious diet, drink plenty of warm water, and all other measures to boost immunity.[9,10] The COVID-positive patient with moderate symptoms such as fever, cough, malaise, difficulty in breathing, and weakness may be considered in the yellow category. These patients need admission at community center with start of specific treatment as per ICMR guideline described in [Table 1]. The COVID-positive patient with severe symptoms (high-grade fever, tachypnea, tachycardia, shortness of breathing, and oxygen saturation <94% even after giving oxygen at the rate of 15 L/min) must be considered to keep in red category. Such sick patients may require ventilator and ICU management, so shift these patients to the higher center at the earliest after giving primary care at the community center.
| Clinical symptoms of COVID-positive patient | Category | Medical advice and intervention at community center | Responsibility of tertiary center |
|---|---|---|---|
| Asymptomatic or mild symptom like fever or upper respiratory tract infection | Green zone | Home isolation or observation at the community center with followings advice. • Contact and droplet precautions. • Strict hand hygiene. • Tab paracetamol for fever. For home isolation patients, seek medical attention when the following warning symptoms/signs occur: • Difficulty in breathing • Persistent pain in the chest. • Mental confusion/drowsiness. • Developing bluish discoloration of lips. • Decrease urine output. |
Take e-round using video conferencing or other telemedicine software. |
| Moderate symptoms like Fever persistent in nature Shortness of breath Cough Spo2 level <94% RR>24/min pneumonia with no signs of severe disease. |
Yellow zone | Admission at community center. • Tab paracetamol for fever. • Tab hydroxychloroquine 400 mg BD on the first day (start only if no heart diseases and ECG shows normal findings) followed by 200 mg BD for the next 4 days. • Tab Dexamethasone 6 mg OD and consider IV methylprednisolone 0.5 to 1 mg/kg for 3 days (if oxygen requirement is increasing) • Tab aspirin 75 mg BD or Low molecular weight heparin (for example, enoxaparin) 40 mg daily subcutaneous. • Start oxygen therapy to keep the target spo2: 92–96% (88–92% in patients with COPD). Investigations: • CBC, LFT, and RFT: Daily • CRP, D-Dimer, and Ferritin: Every 48–72 h (if available) |
Doctor evaluates such patient through phone, CCTV camera, WhatsApp video call. Keep eye open and more vigilant on the patient of this category. Shift to the higher center if any of the following occurs: • Increasing use of breathing( use of accessory muscles) • Hemodynamically not stable. • Increase in oxygen requirement. |
| Severe symptoms like respiratory distress requiring mechanical ventilation (non-invasive and invasive) RR>30/min Spo2 level < 90% on room air or <94% even after giving oxygen @15 L/min. |
Red zone | Try to stabilize the patient as maximum as possible such as start oxygen therapy and other necessary measures which require. Call ambulance. Communicate to higher center about shifting. |
Guide the health worker to stabilize Arrange the bed and team to take such patient at earliest. Start the following treatment: • Maintain euvolemia. • Consider IV methylprednisolone 1 to 2 mg/kg per day for 5–7 days (in 2 divided doses) if not given already. • Enoxaparin 40 mg SC twice/day (if not a high risk of bleeding). • Consider intubation and ventilator management if indicated. • Manage septic shock/sepsis as per standard protocol. • Use sedation and nutrition therapy as per existing guidelines. |
Tocilizumab, Remdesivir, and Convalescent plasma may be considered as investigational therapies. COVID: Coronavirus disease; @: at the rate of ; OD: Once per day; BD: Twice per day. RR: Respiratory rate; CBC: Complete blood count; LFT: Liver function test; RFT: Renal function test; CRP: C-reactive protein.
PERCEIVED IMPACT
While all the big hospitals in the state were facing a rush of patients with symptoms of coronavirus, All India Institute of Medical Sciences, Patna, on July 18, 2020, launched community care for Covid-19 (CCC-19) as a Pilot project at Siwan with facility of telemedicine available by its doctors round-the-clock. The CCC-19 center has been set up with the help of an NGO in 7000 square feet area on the first floor of a building in Chari Bazar village under Barhariya block, about 26 km from Siwan. This center has been started with ten beds. Here, patients who have been tested positive with mild symptoms such as fever are being sent home with prescribed medicine by doctors of AIIMS Patna through telemedicine and considered as green patients. This center is equipped with oxygen cylinder and other equipments. Therefore, patients with moderate symptoms with low saturation of oxygen are being kept at center and oxygen therapy as per requirement has been started to treat such patients under the guidance of telemedicine operator and doctors of AIIMS Patna. On this concept, this center has treated many patients successfully, and till date, no patients were required to shift to a higher center [Figure 1]. Many people contacted doctors of AIIMS Patna to get a bed for admission. Unfortunately, beds were not available, so by recommending this concept, around more than 100 patients arranged all the necessary equipment at their home and followed the advice of doctors, and now, they have recovered completely and given many thanks to the doctor of AIIMS Patna for this novel idea which, in fact, was also cost effective for the patients as shared by recovered patients.
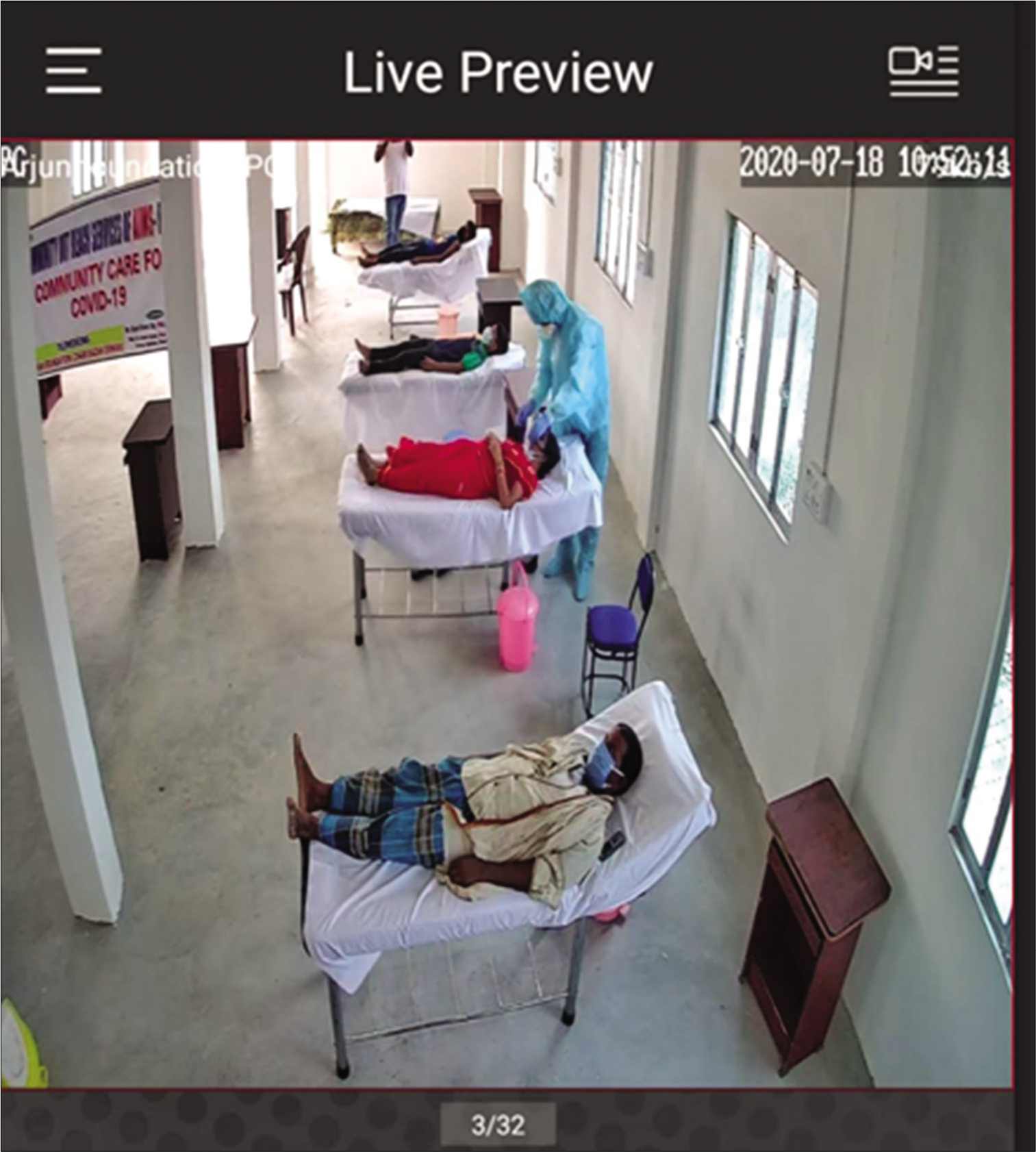
- Showing Community care centre for COVID-19
MONITORING
For every district, there must be one doctor and one administrative person as a nodal and administrative officer, respectively. They will supervise and take e-round every day of all ten centers of that district. They will also find out the trouble and other issues to sort out with the help of DM and competent authority of medical college. The competent authority of tertiary center/medical college as well as DM will also monitor all the beds through CCTV camera in real time and also through video conferencing or any other newly updated computer-based software at any time to assess the conditions of running centers to maintain the social distance while giving advice.[12]
TROUBLE SHOOTING
The patients can share any problems/issues on a given WhatsApp number on the wall of the center. The nodal officer may also contact the higher authority for any issue, feedback, or suggestions to improve the system.
The DM and authorized person of medical colleges will take immediate action to sort out the issue.
There must be a backup plan for financial support to keep the center running.
Every center should also have a backup workforce to take over the center in case the designated person gets ill or stops work due to any reason.
The required items and consumables should also be kept in reserve in case of emergency and shortage to supply at earliest when required.
The observed issues and its solution should be incorporated in standard operating procedure from time to time to make the model robust.
RECOMMENDATION FOR ESTABLISHING SUCH CENTERS IN STATE
Our recommendation is to establish ten centers in each district, and each center will cater ten beds with facility of oxygen therapy as well as medication for yellow and green zone patients. The sick and critical patients would be referred to a higher center with the facility of the dedicated ambulance in the district. We need the help of district administration to run this facility smoothly. The financial help to purchase the entire fixture as well as consumable may be procured by the state Government or NGO or with the help of some person with his/her consent to help their society. The state medical college should provide training to the identified resource person regarding all the skills, knowledge, and behavior which are required to run the center in the community in this pandemic situation. This is not only our responsibility but also on the human ground, we should take the initiative to provide health facility to the last man in the queue.[13] This is the hour of need that government should develop a robust mechanism to involve the common people to fight against corona infection.[14]
EXPERIENCES IN SETTING UP SUCH CENTERS
We established four more such centers with the help of local politicians. I have found the name of resource persons (telemedicine operator and trained health worker) from most of the districts. These persons are ready to take training and are enrolled in this training which will be held in the next few days. They will also arrange the space (community hall, panchayat bhavan, marriage hall, etc.) to establish the ten bedded centers. The only limitation is that I am not getting financial support to purchase the required items for all these centers, which can be run by our trained resource persons. I am trying my best to get financial help from the government as well as NGOs for the establishment of various centers.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Global COVID-19 snapshot with focus on top five. Indian J Med Sci. 2020;72:35-8.
- [CrossRef] [Google Scholar]
- Our fight against the rapidly evolving COVID-19 pandemic: A review of India's actions and proposed way forward. Indian J Community Med. 2020;45:117-24.
- [CrossRef] [PubMed] [Google Scholar]
- India and COVID-19 pandemic-standing at crossroad!!!!! Indian J Med Sci. 2020;72:1-2.
- [CrossRef] [Google Scholar]
- Hospital capacity and operations in the coronavirus disease 2019 (COVID-19) pandemic-planning for the Nth patient. JAMA Health Forum. 2020;1:e200345.
- [CrossRef] [Google Scholar]
- Low-income countries are more immune to COVID-19: A misconception. Indian J Med Sci. 2020;72:5-7.
- [CrossRef] [Google Scholar]
- All India institute of medical sciences triage protocol (ATP): ATP of a busy emergency department. J Emerg Trauma Shock. 2020;13:107-9.
- [CrossRef] [PubMed] [Google Scholar]
- Accountability in healthcare in India. Indian J Community Med. 2020;45:125-9.
- [CrossRef] [PubMed] [Google Scholar]
- COVID-19: Epidemiology and public health aspects. Indian J Community Med. 2020;45:111-6.
- [CrossRef] [PubMed] [Google Scholar]
- Suggested precautions for those under Covid-19 home quarantine/lockdown. Indian J Med Sci. 2019;71:100-1.
- [CrossRef] [Google Scholar]
- Clinical Management Protocol: COVID-19 New Delhi: Government of India, Ministry of Health and Family Welfare, Directorate General of Health Services; 2020.
- [Google Scholar]
- Use of artificial intelligence-based computer vision system to practice social distancing in hospitals to prevent transmission of COVID-19. Indian J Community Med. 2020;45:379-80.
- [CrossRef] [Google Scholar]
- Ethics-based decision-making in a COVID-19 pandemic crisis. Indian J Med Sci. 2020;72:39-40.
- [CrossRef] [Google Scholar]
- Time to win the war against COVID-19: How and where community medicine professionals can contribute? Indian J Community Fam Med. 2020;6:9-12.
- [CrossRef] [Google Scholar]






