Translate this page into:
COVID-19 recovery rate and its association with development

*Corresponding author: Akancha Singh, Research Scholar, International Institute for Population Sciences, Govandi Station Road, Mumbai - 400 088, Maharashtra, India. aksin176@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Singh A, Chattopadhyay A. COVID-19 recovery rate and its association with development. Indian J Med Sci 2021;73(1):8-14.
Abstract
Objectives:
The recovery rate is important to determine a country’s development towards controlling coronavirus. It is a function of myriad factors – death rate, cases requiring hospitalization, quality of care, and discharge policies, among others. India’s recovery rate is growing steadily from an earlier low of 10% to 11%. It is imperative to understand the determinants of recovery rate in a country to enable improvements in the same.
Material and Methods:
COVID-19 data have been compiled from several sources, including the Ministry of Health and Family Welfare, National Disaster Management Authority, and Indian Council of Medical Research and demographic and health data from Census of India, 2011, National Health Profile, 2019, and were used. The study uses linear regression to understand the relationship between recovery rate and development indicators in India.
Results:
Our analysis emphasizes the beneficial impacts of the health system and better economy on the recovery rate. Investment in health, urban stay, non-slum and non-poor population, and effective governance is instrumental in improving recovery rate.
Conclusion:
Scaling up health facilities and medical infrastructure, slum decongestion, focus on economically weaker sections, capacity building of health workers and ameliorating long-term investments in health, health research, and better quality of living are also essential to address recovery of COVID-19.
Keywords
COVID-19
Recovery
Health
Governance
Pandemic
INTRODUCTION
Emerging and epidemic infectious disease outbreaks not only pose an extensive public health problem but are also a menace for global health security.[1] With rapidly changing ecology, escalating urbanization levels increased travel and feeble public health systems, epidemics will become incessant and tougher to prevent and contain.[2] Epidemics are precarious because they not only cause death and debilitation but are also cumbersome for health-care systems and health-care workers and draw resources from services not directly linked to the epidemic. This can leave a legacy of distrust between people, governments, and health systems.[2] Having included the effect on health workers, long-term conditions of 17,000 Ebola survivors, and treatment costs, infection control, screening, and deployment of personnel, the social and economic costs of the Ebola outbreak in West Africa were estimated to be nearly 53 billion Dollars.[3]
As health-care resources become increasingly allocated to epidemic response, death, and disability from other ailments escalate quickly. Such pressure could cause countries, especially low-income countries, to reach a breaking point. Studies have suggested that the spread of infectious diseases is an imminent economic concern, and the annual global cost of moderately-severe to severe pandemics could cost nearly 0.7% of global income.[4,5] Thus, it is imperative to understand not only the pathways and mechanisms of disease transmission but also identify probable socioeconomic determinants of recovery from the disease so as to hasten the process of bringing back the economy and the health-care systems on track.
Amidst continuous burgeoning cases of coronavirus, India has now become the third worst-affected country hit by the novel coronavirus, shortly after the United States of America and Brazil.[6,7] With nearly 1.3 million people recovered till date, India is at the third position in terms of recovery rate [Figure 1]. The number of cases per million and the number of deaths per million across the states of India show wide variations, with the Southern states having both higher number of cases per million and deaths per million [Figure 2].
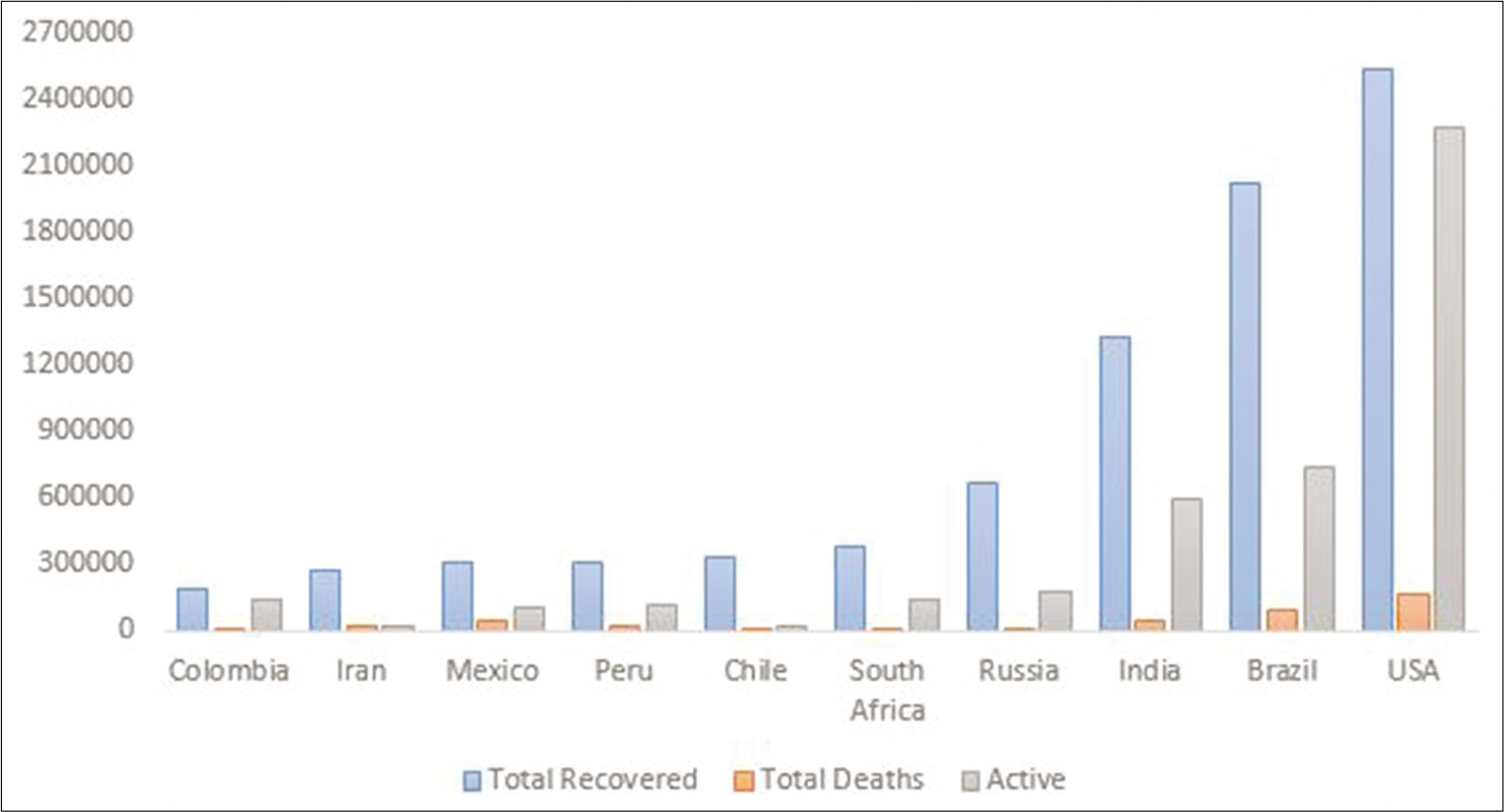
- Countries with the highest number of coronavirus cases. Source: Data obtained from worldometers info as on August 6, 2020.
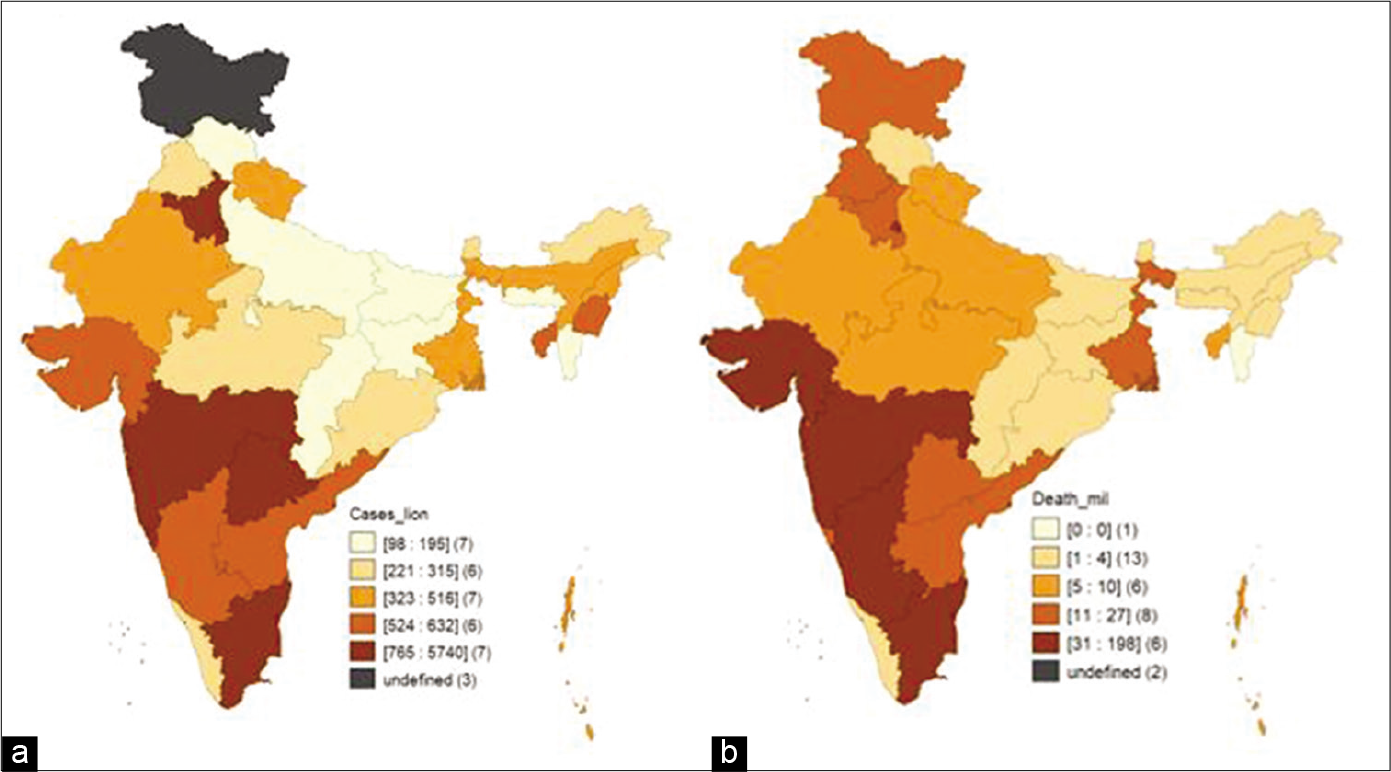
- Choropleth maps showing cases per million and deaths per million in Indian states (as on July 28, 2020). (a) Cases per million, (b) deaths per million.
Given that there are several randomized controlled trials going on worldwide to find a vaccine for the cure of coronavirus, it is important to understand the determinants of coronavirus to ensure the effective utilization of the vaccine once it is successfully found. At present, no particular treatment exists for COVID-19. Standard operating procedure of care focuses on the treatment of the clinical symptoms (pyrexia, cough, and acute respiratory distress syndromes) of patients with supportive care such as fluid management and auxiliary oxygen therapy. Although the clinical efficacy of none of the antiviral agents has been established as yet, some of them (remdesivir, hINFa-2b, ribavirin, chloroquine, and arbidol) are currently under clinical trials for COVID-19.[8,9]
There are several determinants of a country’s performance at its health and non-health fronts. These determinants are crucial when the entire world is waging war against an invisible and seemingly invincible enemy. These socioeconomic determinants form the basis of the current study. The current study attempts to understand the impact of such socio-economic determinants on health fronts during the current pandemic.
Recent data reveal that the top ten worst-affected countries by COVID-19 cases are those which are highly urbanized. Within these countries, the largest cities are the ones that have become the epicenter of the virus, that is, Wuhan in China (population 11 million), New York in the USA (8 million), and London in the UK (9 million).[10] With the most urbanized states being the top ten worst-affected by coronavirus, India’s case is no different. As on June 12, 2020, ten cities of India, Mumbai, Delhi, Chennai, Ahmedabad, Thane, Pune, Indore, Jaipur, Jodhpur, and Surat, had over half the coronavirus cases.[11] The factors responsible are higher population density, especially where the urban poor live and many public amenities such as toilets and water facilities are shared. In addition, urban activities require people to assemble, which negates the norm of social distancing.
As per Census of India, 2011, 17.4% of urban population live in slums. Overcrowding in slums, high population density and illegal settlements inhabited by people on the lower rungs of the economic ladder underpin the challenges of control over the pandemic. NSSO 76th round data, 2018, on Housing show that while 16% of households do not have sufficient availability of drinking water from principal sources, nearly 37% of households use common bathrooms, and 10.3% of the households practice open defecation. These factors further augment the vulnerability of the slums in the context of the current pandemic, and it is, thus, important to understand the socioeconomic linkages of the same.
Despite having several bottlenecks in health infrastructure, India has shown remarkable progress in terms of recovery of COVID-19 cases. The recovery rate of COVID-19 continues to steadily improve. As per the latest data, the recovery rate among COVID-19 patients is nearly 59% (Ministry of Health and Family Welfare [MOHFW], 2020). Over time, the spurt in active cases in India has been slower than the overall growth rate, which is an indication of the rising number of recoveries.[12]
Since the outbreak of the novel-coronavirus in China, there have been studies that talk about the pattern of disease transmission, its socioeconomic determinants, and the mathematical modeling of doubling time and resultant deaths.[13-15] There has been a severe dearth of studies that deal with another important aspect of the pandemic, that is, the recovery rate. The recovery rate from COVID-19, defined in the present analysis as the number of recovered cases per total positive coronavirus cases, has emerged to be one of the major indicators of measuring the accomplishment of a country in effectively restraining the spread of the current coronavirus pandemic. The current study, thus, tries to understand the association between recovery rate and several other socioeconomic determinants.
The study seeks to answer the following research questions:
What are the socioeconomic and political determinants of COVID-19 recovery rate in India?
What are the implications of good governance for the recovery rate?
How does investment in health infrastructure and training of health personnel aid the management of the current pandemic?
MATERIAL AND METHODS
Data
The data for the recovery rate and number of COVID-19 tests per million are compiled from several sources, including MoHFW, Indian Council of Medical Research, and National Disaster Management Authority. The data for number of health workers per 10,000 population have been taken from Karan et al., 2019.[16]
Social indicators such as percent urban, proportion of population living in slums, population density, and proportion of elderly are taken from Census, 2011.
The data on the Good Governance Index have been taken from the Ministry of Personnel, Public Grievances, and Pension. The Good Governance Index, a composite of 10 indicators, is a uniform tool across states to assess the status of governance and impact of various interventions taken up by the State Government and UTs.
Data on proportion of gross state domestic product spent on health are taken from the National Health Profile, 2019.[17]
The variables considered for the analysis have been categorized into four subcategories as per the conceptual framework that has been developed [Figure 3]:
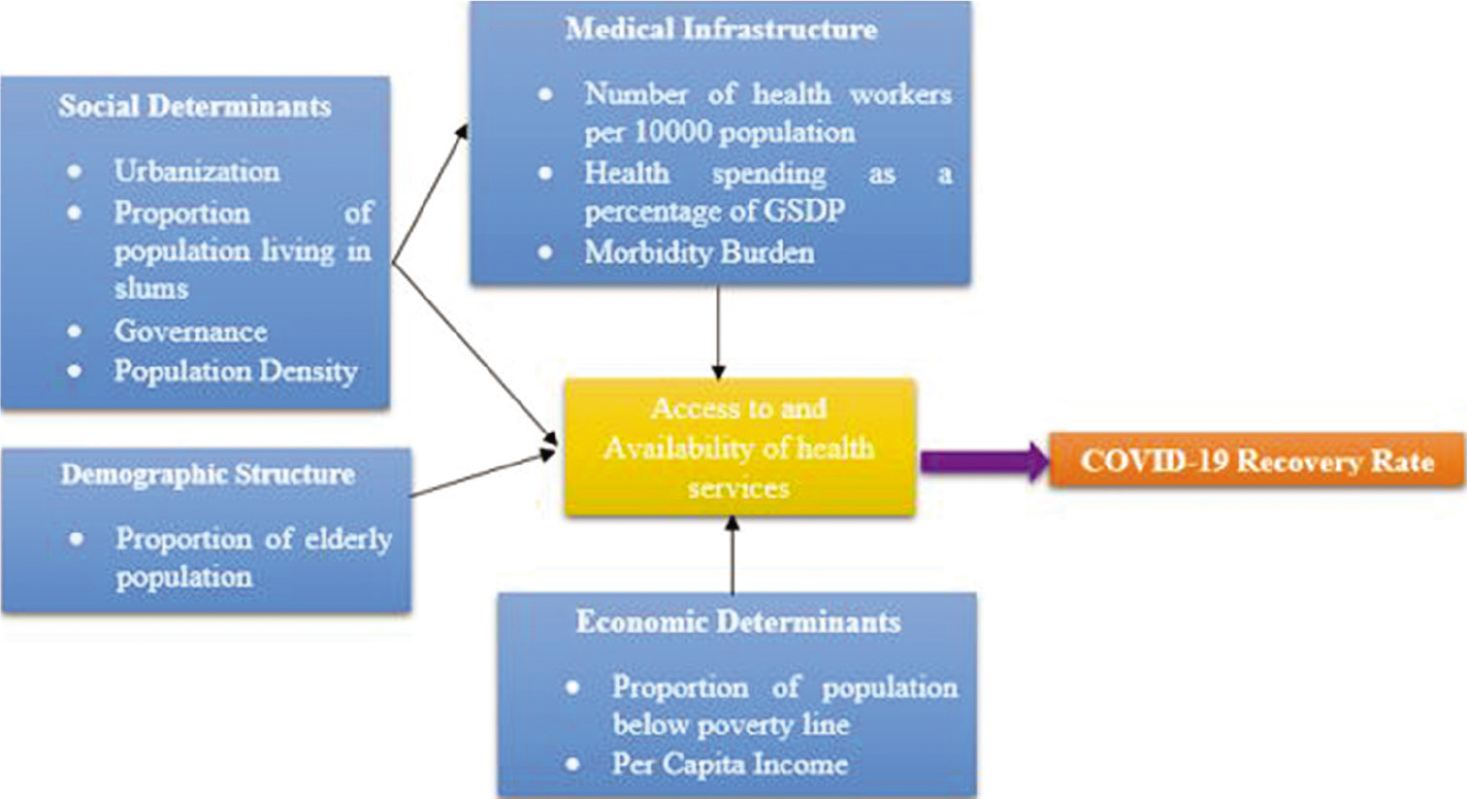
- Conceptual framework relating sociodemographic variables to a recovery rate.
Social determinants: These are helpful in understanding how society reacts to a particular situation. Governance encompasses many dimensions, including the level of democracy, corruption control, the existence of civil conflicts, among others. More democratic governments are more likely to focus on health and related infrastructure and honor human rights.[18-20] Similarly, the level of urbanization and proportion of the population living in slums is also important factors that determine the recovery rate because the geographical location may have an important impact on the disease and recovery pattern.[21-22] Variables under this category are – proportion of population living in slums, Good Governance Index, urbanization, and population density.
Demographic determinants: The demographic structure of a population determines the vulnerability of a population toward an epidemic and its recuperating capacity. This is because certain age groups may be more susceptible to acquiring a disease and might not be able to recover easily.[23,24] Variables under this category are – the proportion of the elderly population.
Medical infrastructure: The medical infrastructure determines the quality and quantity of health services received by people during an epidemic. Countries with advanced health infrastructure are able to deal with epidemics strategically[25-27] and also able to facilitate mass testing and better reporting.[28-30] Variables under this category are – COVID tests per million population, health spending as a proportion of gross state domestic product, and number of health workers per 10,000 population.
Economic determinants: Economic indicators represent a country’s ability to intervene in case of medical emergencies.[31] Variables under this category are – the proportion of population below the poverty line and per capita income.
Statistical analysis
Simple linear regression has been used to estimate the relationship between the rate of change in the recovery rate and various socioeconomic and factors. The rate of change in recovery rate has been calculated using the data on the recovery rate at two points of time, that is, June 27, 2020 and July 28, 2020. The rate of change in the recovery rate is calculated by subtracting the two values.
The econometric form of the model is as follows:
Where, Y = rate of change in recovery rate
β1……….β10 are coefficients for urbanization, slum population, governance, elderly population, population density, COVID-19 tests per million, health workers per 10,000 population, health spending as a percentage of GSDP, per capita income, and population below the poverty line, respectively.
RESULTS
Levels of recovery rate in Indian states
As per the status update by the Union Health Ministry, the recovery rate of India is about 60%. Chandigarh, with a recovery rate of nearly 83%, has the highest recovery rate among all states and UTs. Other states with impressive recovery rates are Uttarakhand, Rajasthan, Madhya Pradesh, Jharkhand, and Odisha (recovery rates above 70%) [Figure 4].
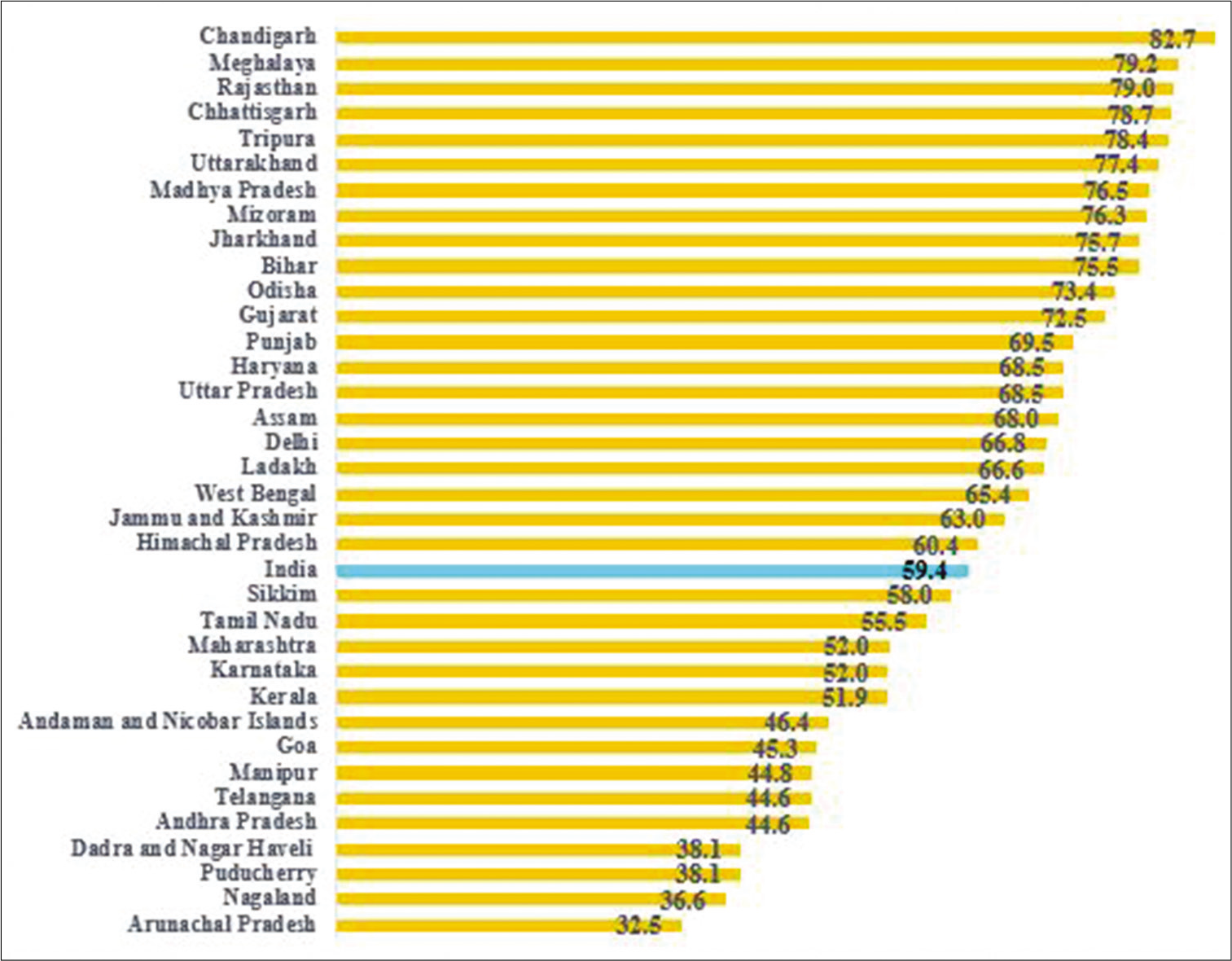
- Recovery rate in Indian states. Source: Data obtained from COVID-9 India organization as on June 30, 2020.
Determinants of COVID-19 recovery rate in India
The study highlights the determinants of recovery rates in India by applying a statistical model. Linear regression was applied to comprehend the relationship between recovery rates and state socioeconomic, spatial, and political variables [Table 1].
| Socioeconomic variables | Recovery rate |
|---|---|
| Social determinants | |
| Urbanization | 0.12** |
| Slum population | −1.43** |
| Good Governance Index | 4.11* |
| Ruling party (Ref. BJP+Allies) | |
| Congress+Allies | 3.80 |
| Others | 6.62 |
| Demographic determinants | |
| Proportion of elderly population | −3.49** |
| Medical infrastructure | |
| Number of health workers per 10,000 population | 0.05** |
| Health spending as a percentage of GSDP | 2.02* |
| Economic determinants | |
| Population below poverty line | −1.01** |
| R-squared | 0.56 |
Results indicate that the recovery rate goes down with an increase in the proportion of population below the poverty line, proportion of slum population, and elderly population. An increase in the proportion of GSDP spent on health, urbanization rate, good governance, and number of health workers per 10,000 populations leads to a significant improvement in the recovery rate. The results have been elaborated section-wise as follows:
Social determinants of recovery rate
A unit increase in urbanization leads to a 0.12 units increase in the recovery rate. Similarly, with unit increase in good governance index, the recovery rate increases by 4.11 units. On the contrary, an increase of 1 unit in the proportion of population living in slums leads to a decline of 1.43 units in the recovery rate.
Another interesting finding is that the recovery rate in the states ruled by the BJP+ allies or INC+ allies and other parties have no significant variation, indicating that COVID-19 recovery has no strong association with political parties, taken as proxy of administrative efficiency.
Demographic determinants
The proportion of the elderly also has a significant negative association with the recovery rate. A 1 unit increase in the proportion of the elderly population leads to a decline of 3.5 units in the recovery rate.
Medical infrastructure
The number of health workers per 10,000 population and the proportion of GSDP spent on health shows a significant positive association with the recovery rate. A 1 unit increase in the number of health workers per 10,000 population leads to an improvement of 0.05 units improvement in the recovery rate.
Economic determinants
Regression results show that a unit increase in the proportion of population below the poverty line leads to an almost equal decrease in the recovery rate.
The R-square value is 0.56, that is, 56% of the variation in recovery rate can be attributed to the socioeconomic, health-related, and political determinants considered in this analysis.
Footnotes: Health workers include doctors, health associates (includes health assistants, sanitarians, dietitians and nutritionists, optometrists and opticians, dental assistants, physiotherapy associates, pharmacists, and pharmaceutical assistants), and nurses and midwives; model has been controlled for population density, COVID tests per million, comorbidity status, and per capita income
DISCUSSION
Our analysis indicates the positive role of the health system, better economy, urbanization, and good governance. A good investment in the health system has proven the success of case recovery by furnishing easy access to health centers, good quality of care, and handling emergency health conditions by mobilizing health resources. States like Rajasthan and Chhattisgarh, which have the highest recovery rate in the country, also have a considerably higher proportion of their GSDP spent on health and a higher number of health workers per 10,000 population. Contrarily, states such as Arunachal Pradesh and Nagaland, which have the lowest recovery rates in the country, also have a meager proportion of their GSDP that is spent on health and a smaller number of health workers per 10,000 population.
Elderly, slum concentration and poverty are hurdles in COVID-19 recovery. Thus, slum population in areas with restricted space are disadvantaged, as observed in the Mega cities of India. It has been established that there are several factors that make the slum population extremely susceptible to the current pandemic. The analysis corroborates previous studies by adding that the recovery rates in slum areas are lower than those in non-slum areas. Further, the study also stresses the importance of allocating resources for the poor amidst the burgeoning disease burden.
There are myriad determinants of mortality rate and severity of COVID-19, the most important of them being age and comorbidities among different age groups. This is especially relevant for countries like India which has one of the highest outbreaks. Strategies to tackle the pandemic need to ensure that high-risk groups such as the elderly and those with underlying diseases such as hypertension, diabetes, and cancer are provided adequate medical assistance. Early access to medical care when infected is vital for improving chances of survival.
Targeting policy response appropriately toward the alleviation of ill-effects of COVID-19 is imperative and especially when the exponential rate of growth is being experienced by India. This, however, requires detailed information on aspects such as which sections of the society are being affected most, in which age groups are more susceptible to contracting the infection and, most importantly, what factors are responsible for the amelioration of recovery from the disease.
With India recording its highest spike in cases in the past 24 h, it becomes imperative to work toward improving the recovery rate.
The paradox of urbanization is evident from the findings of the current study. Although all major hotspots of the pandemic were recorded in the urban centers, especially low-income areas of cities and informal settlements, being in an urban settlement increases the chances of recovery. This entails that the health facilities available in the urban areas are playing a major role in the abetment of the pandemic. Hence, it is absolutely imperative to focus on the health infrastructure.
The analysis suggests that government spending is an important determinant of improving the recovery rate. There can be several plausible explanations for this. An increase in health spending points toward a more developed economy and it could also be instrumental in providing better testing and screening facilities. Large scale testing could be useful in identifying cases and could, thus, be useful in treatment and recovery.[32] There are studies that have classified districts into categories to assess the pandemic situation in them and suggest optimization of monitoring techniques (screening, closedown, curfews, lockdown, evacuations, legal actions, etc.), which could be immensely helpful not only for the government, the medical fraternity, and other frontline workers such as the police and sanitation workers but also for those involved in policymaking and program implementation.[33]
It is beyond doubt that COVID-19 continues to be an enigma and there is so much more to learn about the spread and severity of COVID-19 than what is already known. Epidemiological and clinical evidence suggests that there are myriad novel compounds, as well as medicines licensed for other conditions that have proven effective against COVID-19.[34,35] Death from and acerbity of COVID-19 are associated with several factors, with old age and comorbidities being of paramount importance. This is especially pertinent for countries like India with the highest outbreaks, where strategies must be employed to ensure that high-risk groups, such as old people and those with other underlying disease conditions and medical history such as diabetes and cancer, received adequate safeguard from COVID-19. Therefore, timely access to medical care to infected patients is crucial for improving chances of survival and buttressing the recovery rate in India. Additionally, placing case fatality rate alongside recovery rate after taking a detailed medical history may highlight the highest risk areas and guide the intervention to decrease the spread of the virus. This may enable the development of point-of-care tools to help clinicians in stratifying patients based on possible requirements in the level of care to improve probabilities of survival from COVID-19 disease.[36]
It is also important to understand that though the time taken for patients to recover is substantial, the recovery rate of confirmed cases in India is also quite high. With a rapid increase in the number of patients, the strain on the medical resource will also increase manifold and, thus, estimation of time taken for recovery is also required for proper arrangement and utilization of available resources and judicious use of resources.[37] The current study is, thus, important as it develops a comprehensive understanding of determinants of recovery rate. In the absence of an exhaustive framework pertaining to the recovery rate and its linkages with other socioeconomic variables, this study is a novel attempt to address the issue and its policy connotations. With a better understanding of the dynamics of recovery rate and related determinants, this study can contribute toward the development of appropriate policy interventions.
CONCLUSION
There is an ardent need to understand that apart from the hospitals and health facilities, there are many fronts that the government needs to work on. It is imperative that the government identifies the bottlenecks in the health infrastructure and utilizes its resources judiciously in overcoming theses hurdles because improved management is the key to identifying and alleviating future challenges.[38] It is also important to enhance the involvement of community leaders in identifying the challenges and mobilizing them to inculcate and encourage the norms of social distancing and frequent hand washing and hygiene practices.[39] Equally important is the need for systematic vigilant contact tracing and rational testing, along with other infection prevention and control measures. Contact tracing is an important public health intervention because it is instrumental in ensuring the safety of the in-service health workers and upkeeps the availability of an adequate workforce for health-care service delivery.[40] In addition to the technical aspects, the government also needs to consider the ethical principles of reasonableness, inclusiveness, openness, responsiveness, and accountability to contain the spread of the virus and bring about an amelioration in the recovery rate.[41]
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Modernising epidemic science: Enabling patient-centred research during epidemics. BMC Med. 2016;14:212.
- [CrossRef] [PubMed] [Google Scholar]
- A new twenty-first century science for effective epidemic response. Nature. 2019;575:130-6.
- [CrossRef] [PubMed] [Google Scholar]
- The economic and social burden of the 2014 Ebola outbreak in West Africa. J Infect Dis. 2018;218:S698-704.
- [CrossRef] [PubMed] [Google Scholar]
- The Inclusive Cost of Pandemic Influenza Risk (No. w22137) United States: National Bureau of Economic Research; 2016.
- [CrossRef] [Google Scholar]
- Assessment of economic vulnerability to infectious disease crises. Lancet. 2016;388:2443-8.
- [CrossRef] [Google Scholar]
- Available from: https://www.business-standard.com/article/current-affairs/coronavirus-live-updates-india-cases-at-720-346-delhi-tally-past-100-000-120070700108_1.html [Last accessed on 2020 Jun 30]
- Available from: https://www.theguardian.com/world/2020/jul/06/global-report-india-sees-record-daily-rise-as-capital-opens-giant-covid-19-hospital [Last accessed on 2020 Jun 30]
- Discovering drugs to treat coronavirus disease 2019 (COVID-19) Drug Discov Ther. 2020;14:58-60.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061-9.
- [CrossRef] [PubMed] [Google Scholar]
- Available from: https://www.worldometers.info/coronavirus [Last accessed on 2020 Aug 06]
- These are the 10 Most-affected Cities in India with the Highest Number of COVID-19 Cases Germany: Business Insider; 2020.
- [Google Scholar]
- Available from: https://www.indianexpress.com/article/cities/delhi/key-to-covid-fight-recovery-rate-almost-60-6474996 [Last accessed on 2020 Aug 01]
- Real-time estimation of the risk of death from novel coronavirus 21 (COVID-19) infection: Inference using exported cases. J Clin Med. 2020;9:523.
- [CrossRef] [PubMed] [Google Scholar]
- Early dynamics of transmission and control of COVID-19: A mathematical modelling study. Lancet Infect Dis. 2020;20:553-8.
- [CrossRef] [Google Scholar]
- Factors influencing the epidemiological characteristics of pandemic COVID 19: A TISM approach. Int J Healthc Manage. 2020;13:89-98.
- [CrossRef] [Google Scholar]
- Size, composition and distribution of human resource for health in India: New estimates using national sample survey and registry data. BMJ Open. 2019;9:10.
- [CrossRef] [PubMed] [Google Scholar]
- How potent is economic growth in reducing undernutrition? What are the pathways of impact? New cross-country evidence. Econ Dev Cult Change. 2002;51:55-76.
- [CrossRef] [Google Scholar]
- Governing the Commons: The Evolution of Institutions for Collective Action. Vol 1990. United Kingdom: Cambridge University Press;
- [CrossRef] [Google Scholar]
- The role of the state in governing the commons. Environ Sci Policy. 2014;36:8-10.
- [CrossRef] [Google Scholar]
- The contribution of social behaviour to the transmission of influenza a in a human population. PLoS Pathog. 2014;10:e1004206.
- [CrossRef] [PubMed] [Google Scholar]
- Do respiratory epidemics confound the association between air pollution and daily deaths? Eur Respir J. 2000;16:723-8.
- [CrossRef] [PubMed] [Google Scholar]
- Using data on social contacts to estimate age-specific transmission parameters for respiratory-spread infectious agents. Am J Epidemiol. 2006;164:936-44.
- [CrossRef] [PubMed] [Google Scholar]
- The Spanish influenza pandemic in occidental Europe (1918-1920) and victim age. Influenza Other Respir Viruses. 2010;4:81-9.
- [CrossRef] [PubMed] [Google Scholar]
- Socio-economic determinants of hiv/aids pandemic and nation's efficiencies. Eur J Oper Res. 2007;176:1811-38.
- [CrossRef] [Google Scholar]
- Pandemic influenza and critical infrastructure dependencies: Possible impact on hospitals. Med J Aust. 2006;185:S70-2.
- [CrossRef] [PubMed] [Google Scholar]
- Seasonal and pandemic influenza preparedness: A global threat. J Infect Dis. 2006;194:S65-9.
- [CrossRef] [PubMed] [Google Scholar]
- Predictive power of air travel and socio-economic data for early pandemic spread. PLoS One. 2010;5:e12763.
- [CrossRef] [PubMed] [Google Scholar]
- Health inequalities and infectious disease epidemics: A challenge for global health security. Biosecur Bioterror. 2014;12:263-73.
- [CrossRef] [PubMed] [Google Scholar]
- Monitoring universal health coverage within the sustainable development goals: Development and baseline data for an index of essential health services. Lancet Glob Health. 2018;6:e152-68.
- [CrossRef] [Google Scholar]
- The socio-economic determinants of the coronavirus disease (COVID-19) pandemic. SSRN Electron J. ;2020
- [CrossRef] [PubMed] [Google Scholar]
- Use of cluster analysis to monitor novel coronavirus-19 infections in Maharashtra, India. Indian J Med Sci. 2020;72:44-8.
- [CrossRef] [Google Scholar]
- Potential rapid diagnostics, vaccine and therapeutics for 2019 novel coronavirus (2019-nCoV): A systematic review. J Clin Med. 2020;9:E623.
- [CrossRef] [PubMed] [Google Scholar]
- Potential interventions for novel coronavirus in China: A systematic review. J Med Virol. 2020;92:479-90.
- [CrossRef] [PubMed] [Google Scholar]
- Cross-country comparison of case fatality rates of COVID-19/SARS-COV-2. Osong Public Health Res Perspect. 2020;11:74-80.
- [CrossRef] [PubMed] [Google Scholar]
- Prediction for the spread of COVID-19 in India and effectiveness of preventive measures. Sci Total Environ. 2020;728:138762.
- [CrossRef] [PubMed] [Google Scholar]
- India and COVID-19 pandemic-standing at crossroad? Indian J Med Sci. 2020;72:1-2.
- [CrossRef] [Google Scholar]
- Suggested precautions for those under COVID-19 home quarantine/lockdown. Indian J Med Sci. 2019;71:100-1.
- [CrossRef] [Google Scholar]
- Ensuring safety and availability of healthcare workers in the era of COVID-19: An experience from the Eastern state of India. Indian J Med Sci. 2020;72:58-64.
- [CrossRef] [Google Scholar]
- Ethics-based decision-making in a COVID-19 pandemic crisis. Indian J Med Sci. 2020;72:39-40.
- [CrossRef] [Google Scholar]







