Translate this page into:
Early Intervention of Physiotherapy Helps to Reduce Hospital Stay and Improve Functional Capacity of Patients with Severe COVID – ARDS

*Corresponding author: Akhila Natesan, Department of Physiotherapy, Physiotherapy School and Centre, Topiwala National Medical College and B.Y.L Nair Charitable Hospital, Physiotherapy School and Centre, Topiwala National Medical College and B.Y.L Nair Hospital, Dr. A. L. Nair Road, Mumbai Central, Mumbai - 400 008, Maharashtra, India. akhila.natesan05@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mistry HM, Natesan A, Verma CV. Early Intervention of Physiotherapy Helps to Reduce Hospital Stay and Improve Functional Capacity of Patients with Severe COVID – ARDS. Indian J Med Sci 2021;73(1):75-6.
Dear Editor,
In India, the decision of when physiotherapy should be given to any patient is made by the treating physician. Guidelines of our institute for physiotherapy management in acute care of COVID 19 also stated that physiotherapy intervention was to be given only after the patient has been screened by the treating physician.[1] Evidence on the correct time to refer a COVID patient suffering from severe acute respiratory disease syndrome (ARDS) to a physiotherapist is lacking.
The severe cases manifest as pneumonia followed by cytokine storm resulting in ARDS.[2] It is characterized by three stages, namely, the – acute, organizing, and the healing stage resulting in scar tissues formation and fibrosis.[3]
We observed the effects of evidence based physiotherapy intervention on length of hospital stay and functional capacity (FC) of patients in 4 COVID patients who, were referred by treating physicians in different stages of severe ARDS. Details of the 4 cases is summarized in Table 1.
| Case 1 | Case 2 | Case 3 | Case 4 | |
|---|---|---|---|---|
| Age/gender | 42/Male | 60/Male | 40/Male | 54/Male |
| Comorbidities | Obstructive sleep apnoea, Hypertension |
None | None | None |
| Medications | IL 6 Blocker, Antibiotics, Corticosteroids, Low molecular weight heparin, Hydroxychloroquine, Lopinavir+Ritonavir, Nifedipine |
IL 6 Blocker, Antibiotics, Corticosteroids, Low molecular weight heparin, Hydroxychloroquine |
IL 6 Blocker, Antibiotics, Corticosteroids, Low molecular weight heparin, Hydroxychloroquine |
IL 6 Blocker, Antibiotics, Corticosteroids, Low molecular weight heparin, Hydroxychloroquine |
| Day of admission post first symptom | 8thDay | 9thDay | 5thDay | 3rdDay |
| Physiotherapy referral day post-admission | 38thDay | 13thDay | 3rdDay | 3rdDay |
| Stage of ARDS at the time of physiotherapyreferral | Healing | Organizing | Acute | Acute |
| Total days of oxygen dependency | 47 days | 26 days | 11 days | 9 days |
| Total length of hospital stay | 44 days | 35 days | 25 days | 11 days |
As seen in Table 1, total days of hospital stay can be summarized as, Case 1 > Case 2 > Cases 3 > Case 4.
COVID affected the FC of patients such that they were unable to accomplish even basic activities of daily living (BADLs) such as self-care, ablutions, standing, and walking at ≤ 2.5 mph. Metabolic energy equivalents (METs) are a standardized system used to quantify energy cost of different physical activities. 1 MET equals to the amount of oxygen consumed by a person at rest which is 3.5 ml O2/kg body weight/min. BADLs require ≤ 3 METs.[4]
As seen in Figure 1, case 1 was deconditioned in a span of 55 days during which he received no physiotherapy treatment. Case 2 attained 1.5 METs by the second session; he was more independent than case 1 throughout his hospital stay. Cases 3 and 4 did not have much decline in FC; therefore, they recovered faster than Cases 1 and 2. Case 4 recovered most rapidly.
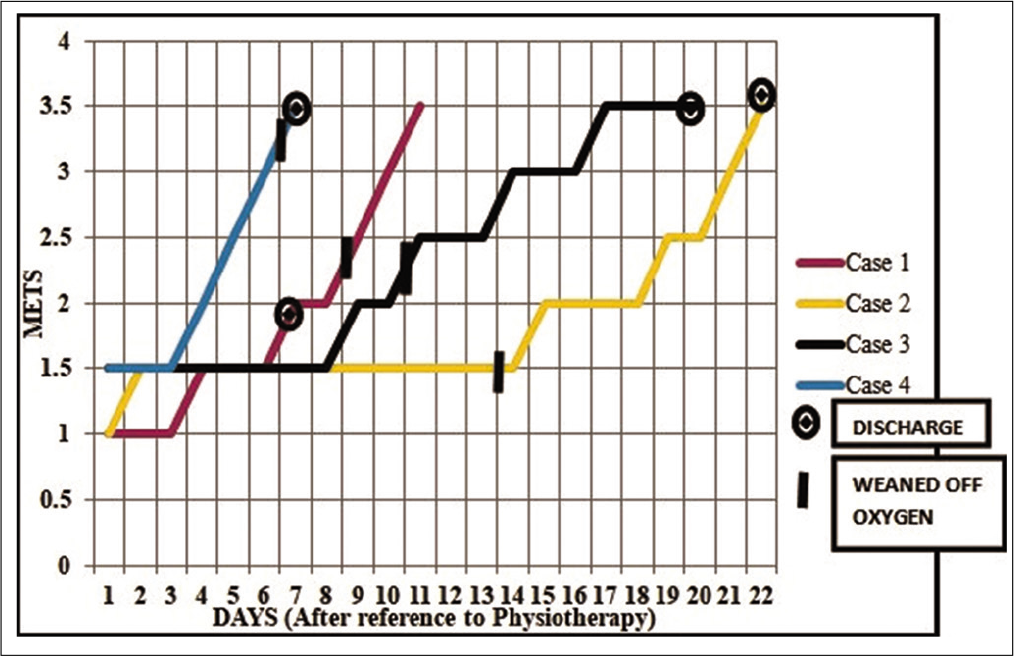
- Functional capacities in terms of METs attained in number of days by all four cases after they were referred for physiotherapy.
At the time of discharge, Case 1 was still dependent on oxygen supplementation and had achieved a capacity of only 1.5 METs; he eventually achieved 3.5 METs with telerehabilitation.
Outcomes of our study were influenced by following factors, increase in awareness of the disease in community, day of hospital admission, medial management, age, and comorbidities.[5,6] Only Case 1 had comorbidities, this may have contributed to the delay in recovery.
Our Municipal Tertiary Care Hospital was converted into a dedicated COVID 19 management facility on April 18, 2020 (2nd lockdown period). Ours was the first government hospital to incorporate physiotherapy in COVID management (May 13, 2020 – the 3rd lockdown period). All four cases were referred for physiotherapy during the 3rd and 4th lockdown period. We observed that as medical management of COVID cases evolved, perceptions of the referring physician regarding the role of physiotherapist also changed over time. Subsequently, patients were referred much earlier for physiotherapy.
To achieve a common goal of weaning off oxygen support, reducing the length of hospital stay and improving functional capacity of COVID patients with severe ARDS, treating physicians should consider reference to physiotherapy as an adjunct to medical management in the early stages.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Guidelines of physiotherapy management in acute care of COVID-19 at dedicated COVID center in Mumbai. Physiother J Indian Assoc Physiother. 2020;14:55-60.
- [CrossRef] [Google Scholar]
- COVID-19: An insight into the developments in diagnostics and therapeutics in India. Indian J Med Sci. 2020;72:77-82.
- [CrossRef] [Google Scholar]
- COVID 19 acute respiratory distress (ARDS): Clinical features and differences from typical preCOVID 19 ARDS. Med J Aust. 2020;213:54-6.
- [CrossRef] [PubMed] [Google Scholar]
- The Compendium of Physical Activities Tracking Guide. Healthy Lifestyles Research Center, College of Nursing and Health Innovation, Arizona State University. World Wide Web. Available from: https://www.sites.google.com/site/compendiumofphysicalactivities [Last accessed on 2020 Sep 04]
- [Google Scholar]
- Coronavirus: Hotspot on coronavirus disease 2019 in India. Indian J Med Sci. 2020;72:29-34.
- [CrossRef] [Google Scholar]





