Translate this page into:
Ensuring safety and availability of healthcare workers in the era of COVID-19: An experience from the Eastern State of India

*Corresponding author: Bijit Biswas, Department of Community and Family Medicine, All India Institute of Medical Sciences, Phulwarisharif, Patna - 801 507, Bihar, India. drbijitbiswas@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Agarwal N, Biswas B, Nair R. Ensuring safety and availability of healthcare workers in the era of COVID-19: An experience from the Eastern State of India. Indian J Med Sci 2020;72(2):58-64.
Abstract
Objectives:
The objective of this study was to design a contact tracing algorithm and contact investigation form for healthcare workers deployed in rendering essential health-care services in limitedly resourced healthcare settings during the COVID era.
Material and Methods:
It was an observational study, longitudinal in design. Based on the existing evidence as of April 15, 2020, we have designed a contact tracing algorithm and contact investigation form to determine the risk of infection among healthcare workers. Later, we have tested the developed contact tracing algorithm and contact investigation from among 28 suspected contacts of a confirmed COVID-19 case admitted in all India Institute of Medical Sciences Patna, Bihar, India.
Results:
Using the designed contact investigation form, all the 28 suspected contacts of the confirmed COVID-19 case were interviewed, among which only 7(25%) were found to be having high-risk exposure. All persons with high-risk exposure were home quarantined for 5 days, along with their direct contacts. Eventually, all high-risk contacts were tested negative on the 5th day after exposure and immediately joined their duties after that. Those who were at low risk of infection continued to work and self-monitor for COVID compatible symptoms for 14 days. Eventually, none of the low-risk exposure persons developed COVID compatible symptoms, therefore deferred testing.
Conclusion:
The contact tracing approach designed in the current study is a balanced one where we tried to balance health workers safety without compromising their availability for duty. This approach can also be implemented in other healthcare settings in the era of COVID-19.
Keywords
COVID-19
Health Personnel
Contact Tracing
Algorithms
Safety
Availability
INTRODUCTION
Contact tracing is a vital public health tool in the case of infectious diseases like COVID-19. It is a process of identification, assessment, and management of people who have been exposed to an infectious disease to prevent further spread.[1,2] When systematically applied for infectious diseases, contact tracing is vital in terms of breaking the chain of transmission, and thereby control disease spread. Contact tracing for COVID-19 requires identification and follow-up of contact for a minimum period of 14 days of suspected or confirmed COVID-19 case.[3,4]
COVID-19 is an overwhelming health-care system of the affected countries, and it is presenting several challenges in the delivery of essential health-care services. Ensuring healthy and adequate human resources to deliver these essential health-care services are one of the major challenges in the COVID-19 era.[5-7] Healthcare workers, due to frequent exposure to the patients, are at more risk of acquiring COVID-19 infection. The safety of every healthcare worker deployed in delivering essential health- care services in the COVID era is vital in terms of their own, colleagues, and visiting patient’s health. However, in healthcare settings with limited resources in terms of workforce, testing kits, etc., sparing all the contacts of a suspected or confirmed COVID-19 case irrespective of the risk of infection may not always be a feasible option. Thus, there was a need for a balanced approach between safety and availability of healthcare workers in limitedly resourced healthcare settings.[6,8] The current study aimed to develop a contact tracing algorithm and contact investigation form for healthcare workers serving in such healthcare settings. This will help health administrators in the determination of health workers level of exposure to a confirmed/suspected COVID-19 case need of testing, and quarantine in limitedly resourced healthcare settings. Further, this will also help them to plan and avail sufficient human resources to render essential health-care services in the COVID era. Through this paper, we would also share an experience of contact tracing among healthcare workers using the formulated contact tracing algorithm and contact investigation form.
MATERIAL AND METHODS
It was an observational study, longitudinal in design. As COVID-19 was disrupting general health-care services, authorities of All India Institute of Medical Sciences (AIIMS), Patna, had decided to deliver only emergency health- care services to keep a check on hospital visit of patients, protecting them from unnecessary risk of COVID infection. On April 15, 2020, a tested positive COVID-19 case had created panic among healthcare workers of the institute. This was because the patient was attended by many healthcare workers in the non-COVID area of the hospital before being admitted in the COVID suspect ward. Most of the healthcare workers working in the non-COVID area of the hospital demanded testing and 14-day home quarantine. Sparing that many health workers for quarantine were not feasible considering the range of services provided by the institute for the attending patients. This evoked need for the development of a contact tracing algorithm and contact investigation form for healthcare workers of the institute to determine their level of exposure, the need for testing, and quarantine. Thus, we formulated a contact tracing algorithm and contact investigation form based on the existing literature available till April 15, 2020.[3,9-12]
Ethical approval of Intuitional Ethics Committee of AIIMS – Patna was taken before drafting and submission of this manuscript. Informed written consent of every study participant was taken before their inclusion in the study. Identity of each study participant was concealed during the drafting of this manuscript.
RESULTS
For determination of the type of exposure, a contract investigation form was being developed to seek appropriate information to determine the type of exposure. The designed contact investigation form is depicted in Supplementary 1. Based on existing literature available, we had defined type of exposure as high risk and low risk. An algorithm for systematic contact tracing was also developed to bring about transparency in the contact tracing process, which is depicted in Figure 1. The conditions of high-risk and low- risk exposure formulated based on existing literature were as following:
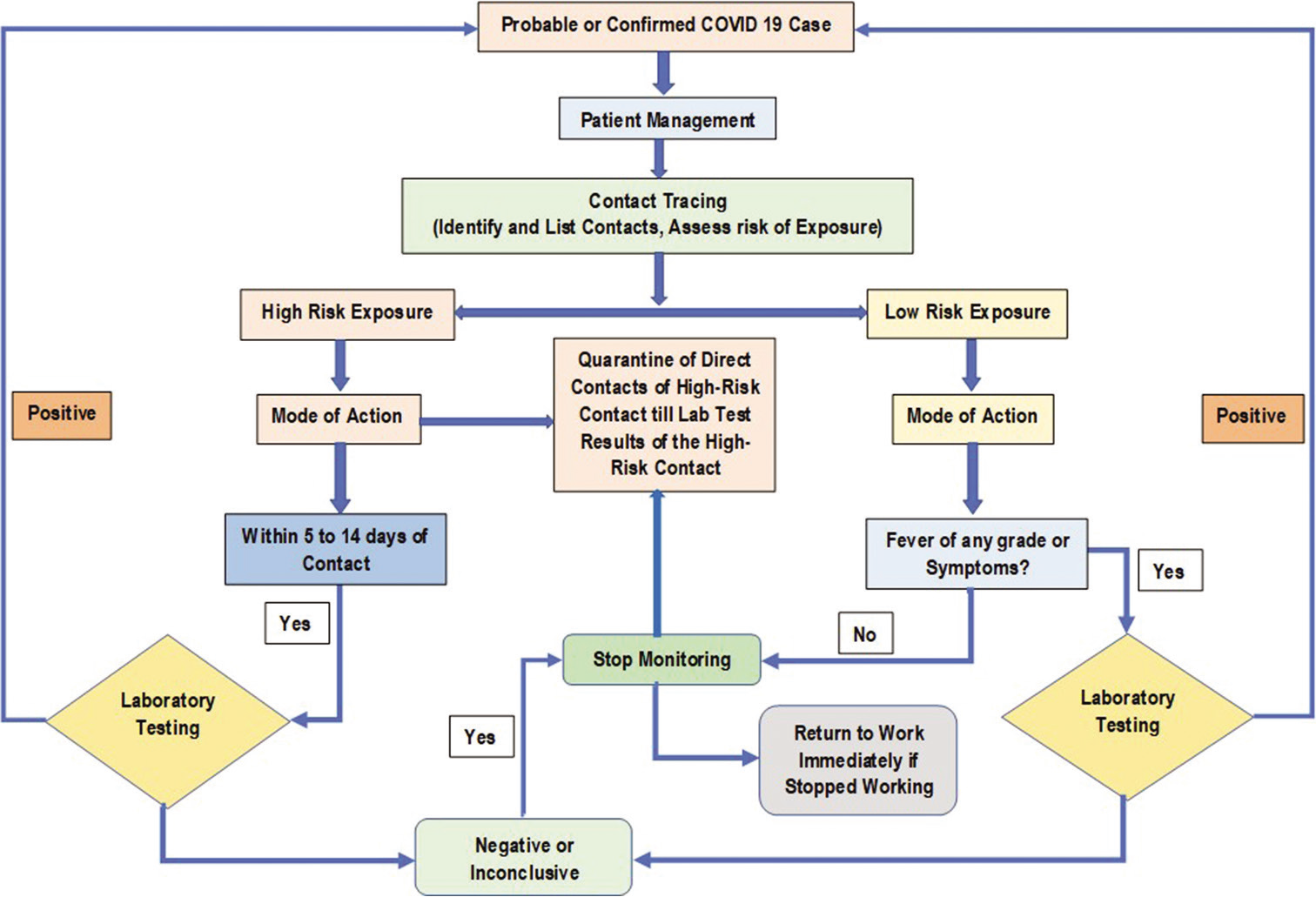
- Algorithm of contact tracing of probable or confirmed COVID-19 case in healthcare workers.
High-risk exposure
Unprotected direct contact with infectious secretions of a COVID-19 case. (i.e., being coughed on, touching used paper tissues or treatment-related documents with a bare hand, and handling swab for COVID testing).
Had direct physical contact with the body of the patient without adequate protection. (i.e., shaking hands and physical examination involving touching the patient).
Touched or cleaned the linens, clothes, or dishes of the patient without adequate protection (standard safety precauction not followed according to the area as per the ministry of health and family welfare [MOHFW]).
Any health worker in close proximity (within 3 ft) of the confirmed case without taking any precaution or adequate protection for more than 15 min. (i.e., accompanying the patient, cardiopulmonary examination of the patient, perform aerosol-generating procedures such as intubation, swab collection, and cardiopulmonary resuscitation).
Low-risk exposure
Shared the same space (worked in the same room/similar and not having a high-risk exposure to a confirmed or suspect case of COVID-19) within 3 ft for <15 min (i.e., measuring the temperature of the patient not involving direct physical contact).
A healthcare worker or other person providing care to a COVID-19 case or laboratory workers handling specimens from a COVID-19 case, wearing the recommended personal protective measures.
The mode of action for defined high-risk and low-risk exposure was also formulated based on existing literature. They were as the following:
Mode of action for high-risk exposure
Stop working and home quarantine till test results.
Quarantine of direct contacts of high-risk contact till laboratory test results of the high-risk contact.
Daily self-monitoring of COVID-19 compatible symptoms (i.e., fever, cough, breathlessness, sore throat, etc.) using apps like Aarogya Setu. In case of any such symptom, contact the affiliated health-care setting.
Maintain rigors hand hygiene and respiratory etiquette.
Maintain social distancing and movement restriction.
Test to be done within 5–14 days of exposure.
Mode of action for low-risk exposure
Continue to work unless developing symptoms.
Maintain social distancing and movement restriction.
Maintain rigors hand hygiene and respiratory etiquette.
Daily self-monitoring of COVID-19 compatible symptoms (i.e., fever, cough, breathlessness, sore throat, etc.) using apps like Arogya Setu. In case of any such symptom, contact the affiliated health-care setting.
COVID-19 case presentation
On April 14, 2020, a 35-year-old male unconscious patient with a space-occupying lesion (on CT brain) was referred to AIIMS, Patna, from a private hospital of Vaishali for further management. The said patient had complaints of severe headache for the past 6 months, history of fever 15 days back, which lasted for 5 days, and he was unconsciousness for past 3 days. The patient was initially screened for temperature, oxygen saturation, and travel history at the entrance of the emergency department and was labeled as a non-COVID suspect. This was followed by the initial management of the patient at the red area of the emergency department. On examination at the time of admission, the Glasgow Coma Score (GCS) of the patient was 4(E1V1M2), with pulse rate, blood pressure, random blood sugar, and oxygen saturation (SpO2) of 112 beats/min, 126/91 mm Hg, 160 mg/dl, and 95%, respectively. On the advice of the treating physician in the emergency, chest X-Ray PA view and CT scan of the brain were performed.
Meanwhile, the neurosurgeon doctor on duty was called for further assessment of the patient. After examining the patient, the neurosurgeon doctor advised for admission in a non- COVID intensive care unit (ICU). However, while transferring the patient to the ICU, the patient developed breathing difficulty with moderate grade fever (100.9°F). As patient developed COVID compatible symptoms, he was immediately transferred to ICU for COVID suspects and next day tested positive.
Contact tracing for COVID-19 among exposed healthcare workers
Using the designed contact investigation form, all the 28 suspected contacts of the confirmed COVID-19 case were interviewed, among which only 7 (25%) were found to be having high-risk exposure. All persons with high-risk exposure were home quarantined for 5 days along with their direct contacts and were advised to self-monitor themselves for COVID compatible symptoms. None of the high-risk contacts developed COVID compatible symptoms, and they all tested negative on the 5th day after exposure and immediately joined their duties after that. The low-risk exposure contacts continued to work and self-monitor for COVID compatible symptoms. Eventually, none of the low-risk exposure contacts developed COVID compatible symptoms, therefore deferred testing. The details of exposure and risk of infection of all 28 identified contacts are depicted in Table 1.
| S. No. | Designation | Details of exposure | PPE used | Risk of infection | |
|---|---|---|---|---|---|
| C-1 | Doctor | Assessed GCS of the patient | Single gloves, surgical mask, foot cover | High risk | |
| C-2 | Doctor | Done general examination and systemic examination of the patient. | Double gloves and surgical mask | High risk | |
| C-3 | Doctor | Taken history from the attendants of the patient while other doctors were examining the patient. During the procedure physical distancing was not maintained. | Single gloves, surgical mask | High risk | |
| C-4 | Doctor | Assisted C-1 in assessment of GCS score of the patient. | Single gloves, surgical mask | High risk | |
| C-5 | Nursing Officer | Accompanied the patient while shifting from emergency department to neurology ICU. Then, eventually to COVID suspect ICU. | Single gloves, surgical mask, foot cover | High risk | |
| C-6 | Hospital Attendant | Accompanied the patient while shifting from emergency department to neurology ICU. Then, eventually to COVID suspect ICU. | Single gloves, surgical mask, foot cover | High risk | |
| C-7 | Nursing Officer | Checked vitals of the patient, collected blood samples for testing, inserted IV cannula, done ABG test and given medication to the patient. | Double gloves, surgical mask, foot cover | High risk | |
| C-8 | Doctor | No direct contact with the patient. Was present in the room while the patient was being examined by other health workers. | Surgical mask | Low risk | |
| C-9 | Doctor | No direct contact with the patient. Was present in the room while the patient was being examined by other health workers. | Surgical mask | Low risk | |
| C-10 | Doctor | No direct contact with the patient. Visited the room while the patient was being examined by other health workers. | Single gloves, N95 mask, slash proof apron, headgear, goggles, foot cover. | Low risk | |
| C-11 | Doctor | No direct contact with the patient. Only patient observation was done. | Surgical mask, headgear, foot cover | Low risk | |
| C-12 | Doctor | No direct contact with the patient. Only patient observation was done. | Single gloves, surgical mask, headgear foot cover | Low risk | |
| C-13 | Doctor | Had not performed any procedure. Visited the room while the patient was being examined by other health workers. | Surgical mask, slash proof apron, headgear, goggles, foot cover | Low risk | |
| C-14 | Doctor | Had not performed any procedure. Visited the room while the patient was being examined by other health workers. | Surgical mask | Low risk | |
| C-15 | Doctor | Evaluated GCS score and intubated the patient. | Double gloves, N95 mask, slash proof apron, goggles, headgear, foot cover. | Low risk | |
| C-16 | Radiographer | Had performed CT scan of the patient. Did not had direct physical contact with the patient. | Double gloves, surgical mask, slash proof apron, headgear, foot cover | Low risk | |
| C-18 | Hospital Attendant | Contact was present in the CT scan room during the CT scan of the patient. No direct contact. During this the contact was wearing | Single gloves, surgical mask, slash proof apron, goggles, headgear, foot cover | Low risk | |
| C-19 | Assistant Radiographer | Assisted in X-ray of the patient. Always maintained at least one-meter distance from the patient. | Double gloves, surgical mask, headgear, foot cover | Low risk | |
| C-20 | Radiographer | Present in same room while X-ray of the patient was being done. No direct contact with the patient. | Single gloves, surgical mask, headgear, foot cover | Low risk | |
| C-21 | Radiographer | Present in same room while X-ray of the patient was being done. No direct contact with the patient. | Single gloves, surgical mask, headgear, foot cover | Low risk | |
| C-22 | Nursing Officer | Present in the same room of emergency where patient was kept initially. No direct contact with the patient. | Single gloves, surgical mask, headgear, foot cover | Low risk | |
| C-23 | Nursing Officer | Present in the same area of emergency where patient was kept initially. No direct contact with the patient. | Single gloves, surgical mask, headgear, foot cover | Low risk | |
| C-24 | Nursing Officer | Checked temperature of the patient by an infrared thermometer. Direct contact with C-5. No direct contact with the patient. | Single gloves, surgical mask, headgear, goggles, foot cover | Low risk | |
| C-25 | Nursing Officer | Checked temperature of the patient by an infrared thermometer. No direct contact with the patient. | Surgical mask | Low risk | |
| C-26 | Nursing Officer | Present in the same area of emergency where patient was kept initially. No direct contact with the patient. | Surgical mask | Low risk | |
| C-27 | Nursing Officer | Monitored vitals of the patient without touching the patient. | Single gloves, surgical mask, foot cover | Low risk | |
| C-28 | Nursing Officer | Monitored vitals of the patient without touching the patient. | Double gloves, surgical mask, foot cover | low risk | |
ABG: Arterial blood gas, COVID: Corona virus disease, C: Contact, GCS: Glasgow coma score, ICU: Intensive care unit, PPE: Personal protective equipment.
DISCUSSION
The current research was aimed at the development of a contact tracing algorithm and contact investigation form for healthcare workers working in limitedly resourced healthcare settings.
In the present study, we have successfully identified all the potential contacts of a COVID-19 case and ensured rational testing. In India, due to its vast population size, there is a potential risk of an increase in its COVID caseload in the coming days, especially after lifting the lockdown measures and initiation of gross population movement.[13-15] To deal with this increased COVID caseload, existing essential health-care services along with the gradual restoration of elective healthcare-related services, adequate healthy healthcare workforce will be required. Throughout the world, several healthcare workers are already infected by COVID-19. In western countries, healthcare workers constitute a significant chunk of their total COVID-19 caseload.[16,17] In India, the COVID situation in healthcare workers is not that worse yet in comparison to its western counterparts. On the other hand, testing every contact of a COVID-19 case may not be feasible for the country as it hinders health workforce availability for rendering healthcare services.[18] But for that, we cannot compromise on the safety of our healthcare workers.
Thus, to keep our health workers safe from COVID, there is a need for systematic vigilant contact tracing and rational testing along with other infection prevention and control measures. Contact tracing has the potential to be a game-changer public health intervention which will help in winning the battle against COVID. This may be because it helps in ensuring the safety of the in-service health workers and upkeeps availability of adequate workforce for health-care service delivery. We suggest that only those with a high risk of infection should be home quarantined for 5 days, along with their high-risk contacts.[9,10] Only high-risk contacts should be tested after initial quarantine for 5 days, while those who are at low risk for infection may continue to work and self-monitor for COVID compatible symptoms using mobile-based screening apps like Arogya Setu.[12] Low-risk contacts of a COVID case should only be tested in case of the development of COVID compatible symptoms. If high-risk contacts after testing found to be COVID negative, they should be immediately inducted in healthcare service delivery without any further delay.
CONCLUSION
The contact tracing approach designed in the current study is a balanced one, where we tried to balance health workers safety without compromising their availability for duty. This approach can also be implemented in other healthcare settings with limited resources to ensure their in-service health workers safety and availability in the era of COVID-19.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- evidence informing the UK's COVID-19 public health response must be transparent. Lancet. 2020;395:1036-7.
- [CrossRef] [Google Scholar]
- How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020;395:931-4.
- [CrossRef] [Google Scholar]
- Contact Tracing: Public Health Management of Persons, Including Healthcare Workers, Having Had Contact with COVID-19 Cases in the European Union-second Update. 2020. ECDC. Available from: https://www.ecdc.europa.eu/en/covid-19-contact-tracing-public-health-management [Last accessed on 2020 May 20]
- [Google Scholar]
- Reorganise and survive-a recommendation for healthcare services affected by COVID-19-the ophthalmology experience. Eye. ;2020
- [CrossRef] [PubMed] [Google Scholar]
- Challenges for NHS hospitals during covid-19 epidemic. BMJ. 2020;368:m1117.
- [CrossRef] [PubMed] [Google Scholar]
- Protecting dental manpower from COVID 19 infection. Oral Dis. ;2020
- [CrossRef] [PubMed] [Google Scholar]
- The Italian health system and the COVID-19 challenge. Lancet Public Health. 2020;5:e253.
- [CrossRef] [Google Scholar]
- Occupational risks for COVID-19 infection. Occup Med (Lond). 2020;70:3-5.
- [CrossRef] [PubMed] [Google Scholar]
- Available from: https://www.ncdc.gov.in/index1.php?lang=1&level=1&sublinkid=632&lid=542. [Last accessed on 2020 May 30]
- Strategy for COVID19 Testing in India. 2020. ICMR. Available from: https://www.icmr.nic.in/sites/default/files/upload_documents/Strategey_for_COVID19_Test_v4_09042020pdf. [Last accessed on 2020 May 21]
- [Google Scholar]
- Novel Coronavirus Disease 2019 (COVID-19) Guidelines on Rational Use of Personal Protective Equipment. 2020. MOHFW, GOI. Available from: https://www.mohfw.gov.in/pdf.GuidelinesonrationaluseofPersonalProtectiveEquipment.pdf. [Last accessed on 2020 May 20]
- [Google Scholar]
- Available from: https://www.play.google.com/store/apps/details?id=nic.goi.aarogyasetu&hl=en_IN. [Last accessed on 2020 May 30]
- Available from: https://www.data.worldbank.org/indicator/SP.POP.TOTL?locations=IN. [Last accessed on 2020 May 30]
- Real-time forecasts and risk assessment of novel coronavirus (COVID-19) cases: A data-driven analysis. Chaos Solitons Fractals. 2020;135:109850.
- [CrossRef] [PubMed] [Google Scholar]
- Outbreak trends of corona virus (COVID-19) in India: A prediction. Disaster Med Public Health Prep. ;2020
- [CrossRef] [PubMed] [Google Scholar]
- On the front lines of coronavirus: The Italian response to covid-19. BMJ. 2020;368:m1065.
- [CrossRef] [PubMed] [Google Scholar]
- Characteristics of health care personnel with COVID-19-United States 2020. MMWR Morb Mortal Wkly Rep. 2020;69:477-81.
- [CrossRef] [PubMed] [Google Scholar]
- Covid-19: How doctors and healthcare systems are tackling coronavirus worldwide. BMJ. 2020;368:m1090.
- [CrossRef] [PubMed] [Google Scholar]







