Translate this page into:
Improving quality of life with sentinel lymph node biopsy in breast cancer patients – An overview
*Corresponding author: Mustafa Ismail, Department of Surgery, Baghdad Teaching Hospital, Baghdad, Iraq. mustafalorance2233@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mahmood AS, Al-Khazaali YM, Abbas AA, Ahmed Ahmed MS, Saleh SA, Bani Saad MA, et al. Improving quality of life with sentinel lymph node biopsy in breast cancer patients – An overview. Indian J Med Sci. 2025;77:28-33. doi: 10.25259/IJMS_137_2024
Abstract
Background:
Sentinel lymph node biopsy (SLNB) has emerged as a less invasive alternative to axillary lymph node dissection (ALND) for staging breast cancer (BC), offering significant reductions in morbidity. This review assesses the impact of SLNB on the quality-of-life (QoL) in BC patients compared to ALND.
Methods:
A comprehensive literature review was conducted using PubMed. The search phrase “(Breast cancer) AND (Sentinel Lymph Node Biopsy) AND (Quality of life)” identified studies comparing SLNB and ALND. A total of eight studies were included in the final analysis. A Preferred Reporting Items for Systematic Reviews and Meta-Analysis diagram illustrates the selection process.
Results:
The review found that SLNB is associated with significantly reduced rates of lymphedema and arm morbidity. Patients treated with SLNB reported better QoL scores in emotional functioning, pain management, and physical mobility compared to those treated with ALND.
Conclusion:
SLNB offers substantial benefits over ALND in terms of reducing post-operative complications and enhancing QoL in BC patients. These findings support the integration of SLNB into routine surgical management for eligible patients, emphasizing long-term patient welfare and functional outcomes.
Keywords
Sentinel lymph node biopsy
Quality of life
Breast cancer
Axillary lymph node dissection
Post-operative outcomes
INTRODUCTION
The shift to sentinel lymph node biopsy (SLNB) in the management of breast cancer (BC) patients is mainly based on the fact that it has huge benefits to be understood in quality-of-life (QoL) preservation after surgery. Justification for the use of SLNB over traditional axillary lymph node dissection (ALND) rests on its less invasive approach, resulting in minimal damage to lymphatic structures and reduced post-surgical complications such as lymphedema, chronic pain, and restricted arm mobility. These complications can profoundly affect physical functioning and, hence, general well-being, so the less invasive SLNB is preferred.[1-3]
The psychological benefits about SLNB cannot be understated either. Patients undergoing less invasive procedures often have less post-operative stress and anxiety, making a positive contribution to emotional and social well-being. These outcomes align with contemporary healthcare objectives that prioritize not only the survival but also the long-term QoL of BC patients.[2,3]
Given this, the following research seeks to perform a critical review on whether SLNB differs from traditional ALND in affecting the QoL among women diagnosed with BC to underline the advantages accruable from modern surgical approaches for the treatment of BC.
METHODS
Literature search strategy
A comprehensive literature search was conducted using PubMed as the primary database. The search was performed using the specific search phrase “(Breast cancer) AND (Sentinel Lymph Node Biopsy) AND (Quality of life)” to identify relevant studies that focus on the QoL outcomes associated with SLNB in BC patients. This search strategy aimed to capture a wide range of studies, including both historical and contemporary perspectives on the topic.
Study selection
Precise inclusion criteria were used to identify research that look at how SLNB affects BC patients’ QoL over the long term. The criteria concentrated on research that compared the physical, emotional, and social dimensions of QoL after SLNB with results from conventional ALND. Peer-reviewed literature and clinical trials with English publication only were taken into account. Studies that did not explicitly address QoL outcomes associated to SLNB and ALND, non-peer-reviewed articles, and articles not available in full text were among the exclusion criteria.
Data extraction and synthesis
In the present study, selected articles were qualitatively analyzed for data extraction on the comparative effectiveness of SLNB versus ALND concerning QoL outcomes. Information systematically recorded in this regard concerned study design, characteristics of participants, surgical techniques, QoL assessment tools, and significant findings. This synthesis followed a narrative approach in relation to significant trends or discrepancies in studies over time and essential changes in the field.
RESULTS
The search yielded a total of 264 records. These records were screened for relevance based on their titles and abstracts. After the initial screening, 249 records were excluded as they did not meet the inclusion criteria. The remaining 15 records were sought for full-text retrieval, but six reports were not retrieved. Consequently, nine full-text articles were assessed for eligibility. Of these, one article was excluded due to irrelevant data or study design, leaving eight studies included in the final review.
The process of study selection and inclusion is illustrated in the Preferred Reporting Items for Systematic Reviews and Meta-Analysis diagram provided [Figure 1].[4] This diagram details the flow of information through the different phases of the systematic review, ensuring transparency and reproducibility of the review process.
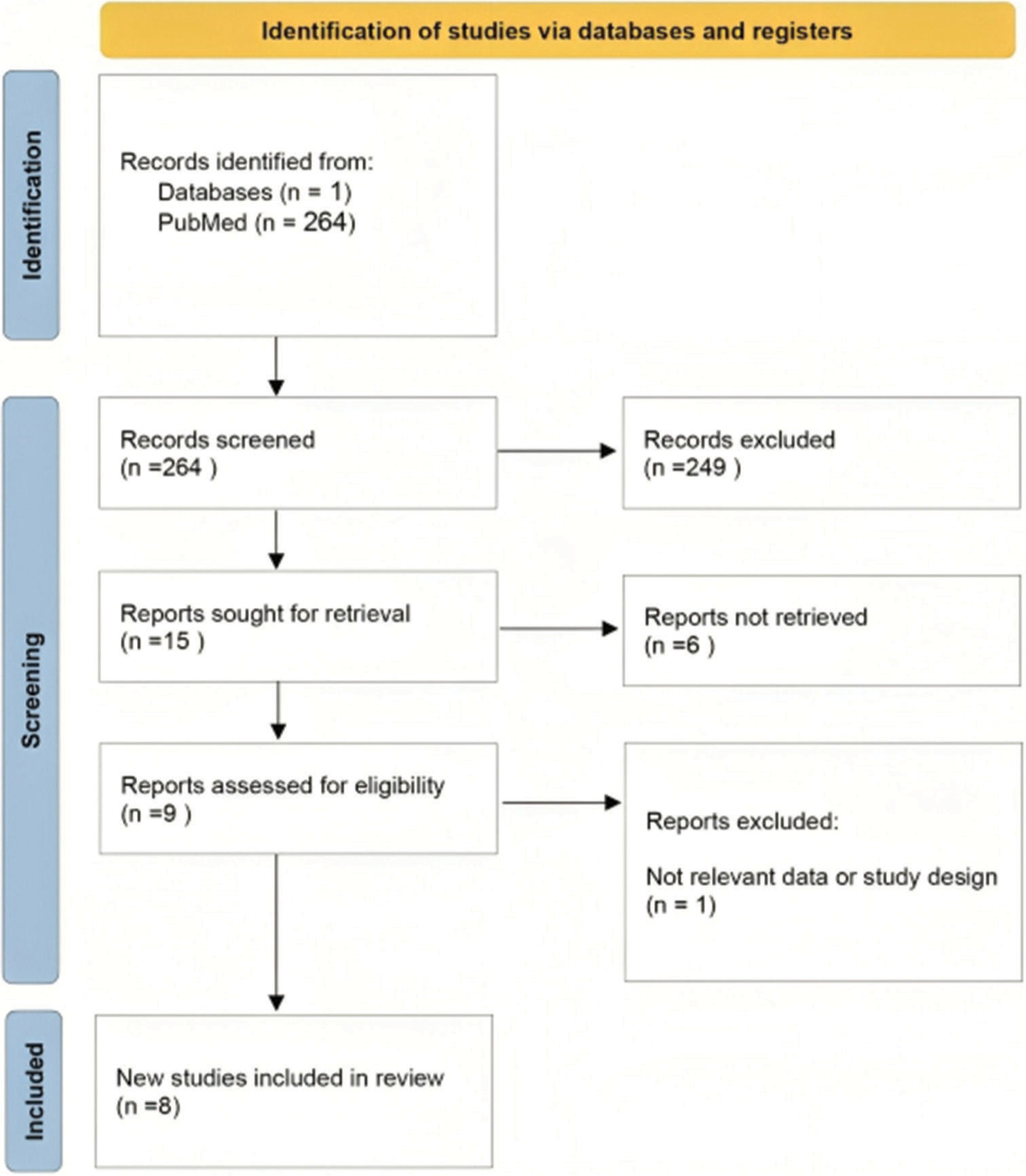
- Preferred Reporting Items for Systematic Reviews and Meta-Analysis diagram of the included studies.
The review identified eight studies that compared the QoL outcomes in BC patients undergoing SLNB versus ALND. The details of these studies are summarized in Table 1.[2,5-11]
| Study | Year | Patient count | Study design | Surgical procedures | QoL assessment tools | Key findings |
|---|---|---|---|---|---|---|
| Peintinger et al. (2003)[5] |
2003 | 56 | Prospective study | SLNB versus ALND | EORTC QLQ-C30, EORTC QLQ-BR23, McGill Pain Questionnaire |
SLNB associated with less arm/shoulder pain and sensory morbidity compared to ALND; faster recovery of global QoL in SLNB group. |
| Dubernard et al. (2004)[6] |
2004 | 179 | Clinical trial | SLNB versus ALND | FACT-B+4 | SLNB associated with delayed chemotherapy onset if SLN status was not diagnosed intra-operatively; younger patients and those undergoing chemotherapy experienced poorer physical well-being. |
| Del Bianco et al. (2008)[7] |
2008 | 677 | Randomized clinical trial | SLNB versus ALND, followed by axillary dissection if SLNB is positive | SF-36, PGWBI | Reduced arm morbidity and better psychological well-being in SLNB group compared to ALND, with effects diminishing over 24 months. |
| Kootstra et al. (2008)[8] | 2008 | 175 | Prospective longitudinal study | SLNB versus ALND | EORTC QLQ-C30 | Emotional functioning improved over time; physical and role functioning initially declined but later improved; SLNB patients reported better recovery to pre-operative levels compared to ALND patients. |
| Chen et al. (2009)[9] | 2009 | 221 | Prospective study | SLNB versus ALND | FACT-B | SLNB associated with better QoL and less morbidity; elevated BMI and ALND were risk factors for post-operative lymphedema. |
| Velloso et al. (2011)[10] | 2011 | 45 | Descriptive, cross-sectional, correlational study | SLNB | EORTC QLQ-C30, EORTC BR-23, DASH | SLNB caused small impairments and limitations in upper limb function during ADL; did not significantly impact HRQoL, which was considered good. |
| Boguševičius and Čepulienė (2013)[2] | 2013 | 48 | Prospective case–control | SLNB versus ALND | QLQ-C30 and QLQ-BR-23 | Improved emotional functioning, pain, sexual functioning, and future perspective in SLNB group over 3 years. |
| Appelgren et al. (2022)[11] |
2022 | 976 | Randomized clinical trial | SLNB versus SLNB+ALND | EORTC QLQ-C30, EORTC QLQ-BR23, Lymph-ICF |
SLNB alone resulted in significantly less arm morbidity and better function in physical, mental, and mobility domains compared to SLNB+ALND; no significant difference in overall HRQoL. |
ALND: Axillary lymph node dissection, DASH: Disabilities of the arm, shoulder and hand, EORTC QLQ-BR23: European organization for research and treatment of cancer quality-of-life questionnaire-breast cancer module, EORTC QLQ-C30: European organization for research and treatment of cancer quality-of-life questionnaire-core 30, FACT-B+4: Functional assessment of cancer therapy-breast plus additional items, Lymph-ICF: Lymphoedema functioning, disability and health questionnaire, McGill Pain Questionnaire: A tool to evaluate pain quality and intensity, PGWBI: Psychological general well-being index, QLQ-BR-23: Quality-of-life questionnaire - breast cancer module 23, QLQ-C30: Quality-of-life questionnaire core 30, SF-36: Short form (36) health survey, SLNB: Sentinel lymph node biopsy, SLN: Sentinel lymph node, ADL: Activities of daily living, HRQoL: Health-related quality of life, BMI: Body mass index, QoL: Quality of life
Peintinger et al.[5] conducted a prospective study involving 56 patients to compare SLNB and ALND. They found that SLNB was associated with less arm and shoulder pain and sensory morbidity compared to ALND. Moreover, patients who underwent SLNB experienced a faster recovery of global QoL. Dubernard et al.[6] performed a clinical trial with 179 patients and reported that SLNB was associated with a delay in the onset of chemotherapy if the sentinel lymph node (SLN) status was not diagnosed intraoperatively. Younger patients and those undergoing chemotherapy experienced poorer physical well-being.
Del Bianco et al.[7] conducted a randomized clinical trial with 677 participants. The study found that SLNB was associated with reduced arm morbidity and better psychological well-being compared to ALND, although these effects diminished over 24 months.
Kootstra et al.,[8] in a prospective longitudinal study involving 175 patients, reported that emotional functioning improved over time for patients undergoing SLNB. Although physical and role functioning initially declined, they later improved, and SLNB patients reported better recovery to pre-operative levels compared to ALND patients.
Chen et al.,[9] in a prospective study of 221 patients, observed that SLNB was associated with better QoL and less morbidity compared to ALND. The study also identified elevated body mass index (BMI) and ALND as risk factors for postoperative lymphedema.
Velloso et al.[10] conducted a descriptive cross-sectional correlational study involving 45 patients and found that SLNB caused small impairments and limitations in upper limb function during activities of daily living (ADL). However, it did not significantly impact the health-related quality of life (HRQoL), which was considered good.
Boguševičius and Čepulienė (2013),[2] in a prospective case-control study with 48 patients, demonstrated that SLNB improved emotional functioning, pain management, sexual functioning, and future perspective over a 3-year period compared to ALND.
Appelgren et al.[11] in a randomized clinical trial involving 976 patients, found that SLNB alone resulted in significantly less arm morbidity and better function in physical, mental, and mobility domains compared to SLNB + ALND. There was no significant difference in overall HRQoL between the groups.
These studies collectively show that SLNB is linked to a considerable decrease in post-operative morbidity and a long-lasting improvement in QoL compared to ALND. The consistent findings across these studies support the use of SLNB as a preferred surgical approach in BC management.
DISCUSSION
This review aimed to evaluate the impact of SLNB on the QoL of BC patients compared to ALND. Our comprehensive literature search using PubMed yielded eight relevant studies that were systematically reviewed and synthesized to provide a broad perspective on this topic. The findings indicate that SLNB offers significant advantages over ALND in terms of reducing post-operative morbidity and enhancing QoL in BC patients.
SLNB has emerged as a less invasive alternative to ALND, providing accurate staging of BC with minimal complications. Studies included in this review consistently showed that SLNB is associated with better QoL outcomes compared to ALND. For instance, Peintinger et al.[5] reported that patients undergoing SLNB experienced less arm and shoulder pain and faster recovery of global QoL compared to those undergoing ALND. This is corroborated by Dubernard et al.,[6] who found that while SLNB delayed chemotherapy onset if the SLN status was not diagnosed intraoperatively, younger patients and those undergoing chemotherapy experienced poorer physical well-being.
Del Bianco et al.[7] found that SLNB was associated with reduced arm morbidity and better psychological well-being, although these effects diminished over time. Similarly, Kootstra et al.[8] observed that emotional functioning improved over time in SLNB patients, and they reported better recovery to pre-operative levels compared to ALND patients.
Chen et al.[9] highlighted that SLNB was associated with better QoL and less morbidity, identifying elevated BMI and ALND as risk factors for post-operative lymphedema. Velloso et al.[10] indicated that SLNB caused small impairments in upper limb function during ADL but did not significantly impact overall HRQoL.
Boguševičius and Čepulienė[2] demonstrated that SLNB improved emotional functioning, pain management, sexual functioning, and future perspective over a 3-year period compared to ALND. Finally, Appelgren et al.[11] found that SLNB alone resulted in significantly less arm morbidity and better physical, mental, and mobility functions compared to SLNB combined with ALND, without significant differences in overall HRQoL.
Velanovich and Szymanski[12] reported significantly lower QoL scores related to bodily pain and emotional roles in patients with lymphedema following ALND. Their findings highlighted the severe impact of ALND-related lymphedema on the emotional and physical well-being of patients. This underscores the importance of less invasive procedures like SLNB in mitigating these adverse outcomes.
Mansel et al.[13] conducted a large randomized clinical trial and found that SLNB was linked to decreased arm morbidity and improved QoL compared to ALND. Their study supports the growing evidence that SLNB should be considered the standard approach for staging BC due to its favorable QoL outcomes.
Furthermore, Gärtner et al.[14] found that SLNB resulted in better functional and QoL outcomes compared to ALND, especially in terms of arm morbidity and lymphedema. Borm et al.[15] reported that SLNB led to significant improvements in postoperative QoL and less physical discomfort compared to ALND. Furlan et al.[16] observed that patients undergoing SLNB had better psychological well-being and less physical impairment, reinforcing the benefits of SLNB in BC management.
The findings from these studies highlight the significant benefits of SLNB over ALND, making it a preferred surgical approach for staging and treating BC.[15,17] Reduced arm morbidity and improved QoL are critical factors in patient-centered care, aligning with contemporary healthcare objectives that prioritize not only survival but also the long-term well-being of BC patients.
While this review presents strong evidence supporting SLNB, it is important to acknowledge certain limitations. Many studies relied on self-reported measures for QoL assessment, which may introduce subjective bias. In addition, most reviewed studies did not control for confounding variables such as patients’ pre-operative psychological status, cancer extent at diagnosis, and individual differences in postoperative care. Furthermore, the generalizability of findings to lower-resource settings may be limited, given that most data derive from high-resource environments.
Future research should address these limitations by incorporating objective QoL measures, controlling for confounding variables, and including diverse patient populations from various healthcare settings. Longitudinal studies with consistent follow-up periods are also essential to fully understand the long-term effects of SLNB and ALND.
In conclusion, SLNB offers significant benefits over ALND in reducing post-operative morbidity and enhancing QoL in BC patients. This review supports the integration of SLNB into standard surgical management for eligible patients, highlighting its role in improving long-term patient outcomes and overall well-being.
CONCLUSION
SLNB significantly improves the QoL for BC patients compared to ALND. The reviewed studies consistently show that SLNB results in less post-operative morbidity, reduced arm and shoulder pain, and faster recovery of global QoL. Emotional and psychological well-being is also better preserved with SLNB. These benefits underscore the importance of incorporating SLNB into standard BC surgical management, emphasizing patient-centered care that prioritizes long-term QoL and minimizes physical and emotional complications. Future research should continue to refine these findings and explore broader patient populations.
Availability of data and materials
This is a review article that all the data are already published in the literature.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Impact of sentinel node biopsy on long-term quality of life in breast cancer patients. Br J Cancer. 2013;109:2783-91.
- [CrossRef] [PubMed] [Google Scholar]
- Quality of life after sentinel lymph node biopsy versus complete axillary lymph node dissection in early breast cancer: A 3-year follow-up study. Medicina (Kaunas, Lithuania). 2013;49:111-7.
- [CrossRef] [Google Scholar]
- Implications of a postoperative rehabilitation program on quality of life in women with primary breast cancer treated with sentinel lymph node biopsy or complete axillary lymph node dissection. Ann Surg Oncol. 2008;15:3342-9.
- [CrossRef] [PubMed] [Google Scholar]
- The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of quality of life and arm complaints after sentinel lymph node biopsy and axillary lymph node dissection in breast cancer patients. Br J Cancer. 2003;89:1229-33.
- [CrossRef] [PubMed] [Google Scholar]
- Quality of life after sentinel lymph node biopsy versus complete axillary lymph node dissection in early breast cancer. Eur J Surg Oncol. 2004;30:771-9.
- [CrossRef] [PubMed] [Google Scholar]
- Morbidity comparison of sentinel lymph node biopsy versus conventional axillary lymph node dissection for breast cancer patients: Results of the sentinella-GIVOM Italian randomised clinical trial. Eur J Surg Oncol. 2008;34:508-13.
- [CrossRef] [PubMed] [Google Scholar]
- Quality of life after sentinel lymph node biopsy or axillary lymph node dissection in stage I/II breast cancer patients: A prospective longitudinal study. Ann Surg Oncol. 2008;15:2533-41.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of quality of life and complications after breast reconstruction, breast-conserving surgery and mastectomy for Chinese breast cancer patients. Am J Surg. 2009;198:817-22.
- [Google Scholar]
- Quality of life in breast cancer patients after sentinel lymph node biopsy or axillary lymph node dissection: A cross-sectional study. Support Care Cancer. 2011;19:1479-85.
- [Google Scholar]
- Arm morbidity after sentinel lymph node biopsy and axillary lymph node dissection in women with early breast cancer in the randomized SENOMAC trial. Eur J Surg Oncol. 2022;48:764-71.
- [Google Scholar]
- Quality of life of breast cancer patients with lymphedema. Am J Surg. 1999;177:184-8.
- [CrossRef] [PubMed] [Google Scholar]
- Randomized multicenter trial of sentinel node biopsy versus standard axillary treatment in operable breast cancer: The ALMANAC Trial. J Natl Cancer Inst. 2006;98:599-609.
- [CrossRef] [PubMed] [Google Scholar]
- Self-reported arm-lymphedema and functional impairment after breast cancer treatment-a nationwide study of prevalence and associated factors. Breast. 2010;19:506-15.
- [CrossRef] [PubMed] [Google Scholar]
- Acute toxicity and cosmetic outcome in the randomised phase III PBI trial: First results of patient-reported outcome and physicians' evaluation. Radiat Oncol. 2020;15:1-8.
- [Google Scholar]
- Quality of life after sentinel lymph node biopsy or axillary lymph node dissection in stage I/II breast cancer patients: A prospective longitudinal study. Ann Surg Oncol. 2020;27:2041-52.
- [Google Scholar]
- Sentinel lymph node biopsy vs no axillary surgery in patients with small breast cancer and negative results on ultrasonography of axillary lymph nodes: The SOUND randomized clinical trial. JAMA Oncol. 2023;9:1557-64.
- [CrossRef] [PubMed] [Google Scholar]






