Translate this page into:
Multisite cutaneous tuberculosis in an immunocompetent patient – A mysterious presentation of yet common disease
*Corresponding author: Hena Butta, Department of Microbiology, Indraprastha Apollo Hospitals, New Delhi, Delhi, India. henavasdeva@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Butta H, Ahuja J, Mendiratta L, Sardana R. Multisite cutaneous tuberculosis in an immunocompetent patient – A mysterious presentation of yet common disease. Indian J Med Sci. doi: 10.25259/IJMS_121_2024
Abstract
Cutaneous form of tuberculosis depicts a rare entity despite high occurrence of pulmonary tuberculosis. We report a case of cutaneous tuberculosis in a 24 years immunocompetent female who presented with multiple subcutaneous lesions over acral parts with discharging pus since past 6 months. The diagnosis was microbiologically confirmed by acid-fast bacilli (AFB) stain, AFB culture, and molecular testing for tuberculosis. The patient showed good response to antitubercular therapy with no relapse. Patient being dog rescuer, highlights the possibility of transmission of tuberculosis from dogs, and generates a new area of research.
Keywords
Cutaneous tuberculosis
Immunocompetent
Mycobacterium
Multisite
Dogs
INTRODUCTION
Cutaneous form of tuberculosis depicts as a rare entity despite high occurrence of pulmonary tuberculosis and availability of newer diagnostic tests for tuberculosis. It is more prevalent in regions around the globe, where infections such as human immunodeficiency virus (HIV) are common, or in immunodeficient populations.[1] The disease happens due to cutaneous invasion of Mycobacterium tuberculosis complex which can be exogenous (direct inoculation) or endogenous (hematogenous or lymphatic dissemination) resulting in granuloma formation. It is important to differentiate between varied lesions of cutaneous tuberculosis from other dermatological lesions for the timely management of the patients. Here, we report a case of cutaneous tuberculosis in an immunocompetent female which is a rarity amongst rare lesions of tuberculosis.
CASE REPORT
A 24-year-old female presented in the outpatient department of our hospital in September 2021 with multiple subcutaneous lesions over acral parts with discharging pus since past 6 months. Initially, multiple small lesions were noticed at the base of left thumb nail. It was followed by a big pustular lesion on the thenar aspect of left hand which turned into abscess for which incision and drainage were done in May 2021. Few days after incision and drainage, similar type of lesion occurred on the thenar aspect of the right hand followed by reappearance of lesion on thenar aspect of left hand and then spread of lesion on both hands including fingers. After that, the lesions started appearing on lower extremities, that is, toes and sole of both the feet. It was followed by appearance of lesion near eyebrows. Furthermore, there was continuous oozing from the incision and drainage site and that site remained unhealed. Before presenting to our facility, the patient had multiple courses of multiple antibiotics but without any clinical response. The patient gave history of on and off fever for the past 6 months. There was no obvious weight loss, loss of appetite, and cough. The patient was a dog rescuer and used to play with stray dogs. The patient also gave history of exposure with her close relative who was on antitubercular treatment for incidentally diagnosed lymph node tuberculosis. On examination, there were large fluid filled lesions mostly non-discharging over right hand and left hand [Figure 1]. Lesions were also seen on bilateral feet [Figure 2] and over eyebrows. All the lesions were minimally tender. Her weight was 55 kg. Basic investigations done prior showed total leucocyte count – 6100/mm3, hemoglobin – 10.1 g/dL, erythrocyte sedimentation rate 34 mm/h, random blood sugar – 95.8 mg/dL, and Mantoux test 15 mm induration. Differential diagnosis of cutaneous tuberculosis and fungal infection (mycetoma/histoplasmosis) was made and pus aspirate from right hand was evaluated mainly for tubercular and fungal etiology. Gram stain and fungal smear (KOH) examination were negative. Ziehl-Neelsen stain showed acid-fast bacilli (AFB) lying singly in smear [Figure 3]. Tuberculosis real time polymerase chain reaction was positive for M. tuberculosis complex and in cartridge-based nucleic acid amplification test (CBNAAT) for tuberculosis, M. tuberculosis complex was detected and rifampicin resistance was not detected. Fungal culture inoculated on two tubes of Sabouraud’s dextrose agar and brain heart infusion) agar at 25°C and 37°C remained sterile after 3 weeks of incubation. AFB culture was done by both mycobacteria growth indicator tube (MGIT) method and conventional method using Lowenstein Jensen (LJ) media. Mycobacteria were grown after 15 days of incubation which was further identified as M. tuberculosis complex using MPT64 protein detection-based immunochomatographic test (SD Bioline Kit, Standard Diagnostics, Inc., Korea). Growth was also observed on LJ media after 20 days.

- Fluid filled lesion over left hand (orange arrow).

- Lesion on right foot (orange arrow).
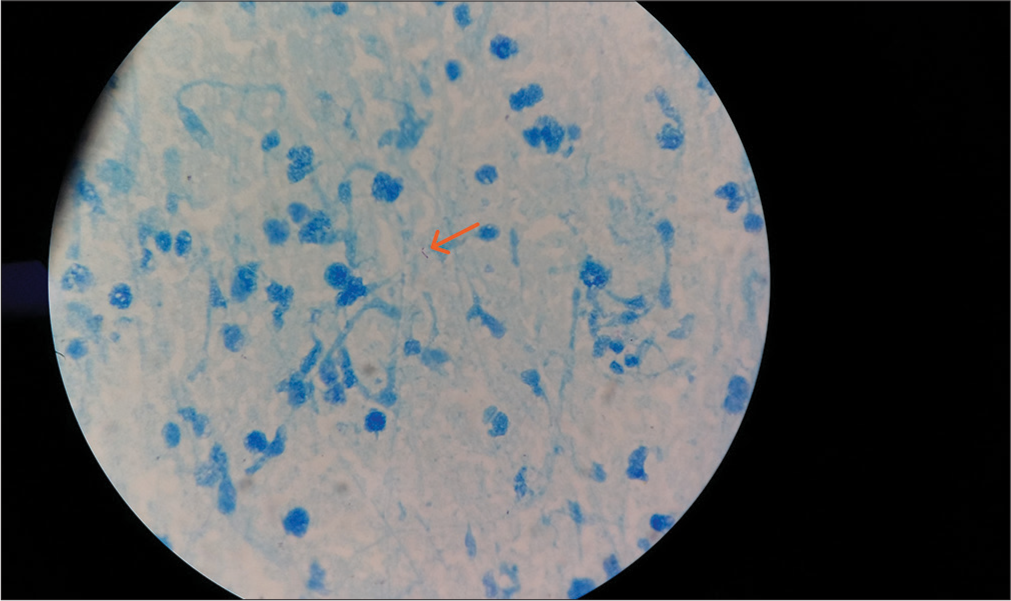
- Ziehl Neelsen stain-Acid fast bacilli lying singly (orange arrow) (×1000).
Serological tests such as HIV, venereal disease research laboratory, hepatitis B surface antigen, and hepatitis C virus tests were all non-reactive. AFB susceptibility testing was done by proportion method using MGIT-960 for both first- and second-line drugs and the isolate was susceptible to all the antitubercular drugs tested (Rifampicin, isoniazid, ethambutol, pyrazinamide, streptomycin, kanamycin, amikacin, capreomycin, ciprofloxacin, and p-aminosalicylic acid). After AFB stain and CBNAAT reports, diagnosis of cutaneous tuberculosis was made and anti-tubercular treatment was started. The patient was given rifampicin (600 mg OD), isoniazid (300 mg OD), ethambutol (1200 mg OD), and pyrazinamide (1250 mg OD). The patient was advised to get her liver function test done every week and report after 1 month. After 1 month, all the lesions were drastically regressed and patient was continued with the same treatment for 1 more month. After 2 months of treatment, all lesions were resolved and patient gained around 3 kg weight. Hence, other tests for immunodeficiency were not indicated and patient was shifted from intensive phase regimen to continuation regimen of antitubercular treatment. The patient was prescribed rifampicin (600 mg OD), isoniazid (300 mg OD), and ethambutol (1200 mg OD) for 4 months with follow-up every 2 months. Few days after discontinuation of pyrazinamide, the patient noticed slightly fluid-filled lesion on her right hand. Pyrazinamide was started again for 1 more month followed by continuation regimen. Treatment of total 6 months was given and there is no recurrence of infection till date.
DISCUSSION
Cutaneous tuberculosis is an uncommon manifestation of extra-pulmonary tuberculosis and comprises only a miniscule proportion (<1–2%) of all cases of tuberculosis.[2] Although not life threatening, it does cause significant mental distress to the patient due to discomfort and disfigurement. Among the exogenous tuberculosis, tuberculous chancre, tuberculosis verrucosa cutis, and lupus vulgaris are most common lesions.[3] Endogenous cutaneous tuberculosis due to contiguous spread or autoinoculation include scrofuloderma, a few cases of lupus vulgaris, tuberculosis cutis orificialis, and the ones occurring due to hematogenous spread include most of lupus vulgaris, tuberculous gumma, and acute miliary tuberculosis.[4] The mode of transmission and the type of cutaneous tuberculosis in our immunocompetent patient is difficult to infer. However, most likely, this is presentation of tuberculosis verrucosa cutis which is mostly seen in locations which are prone to trauma such as fingers and toes. We tried to decipher the mode of transmission of cutaneous tuberculosis in the patient. There were two incidences before development of skin lesions; one was close exposure to stray dogs and other was exposure with her relative who was incidentally diagnosed with latent lymph node tuberculosis. The patient was engineer by profession and was doing work from home during COVID when she developed interest in caring street pup dogs and used to hold them in her lap and bring them home for feeding and care. She used to wash her hands after leaving them back in their shelter but never washed/ changed/cleaned her belongings after contact with the street pup dogs. Although association of dogs in acquisition of human tuberculosis is unclear; yet, dogs may rarely be infected by M. tuberculosis. Furthermore, dogs may become infected in the first place from one of their human contacts, who is also a source of exposure to other people; however, it remains uncertain whether dogs become infected primarily from human subjects.[5] There are series of cases in which human owner has been implicated as the source of infection in canine (dog and cat) tuberculosis.[6] Furthermore, there has been a case report of epidemiological linking between human and canine (dog) case by M. tuberculosis genotyping.[7] However, the association between dogs as a source of infection for cutaneous tuberculosis in human beings could not be seen in published literature searched by us. Acquisition of infection from a case of latent lymph node tuberculosis remains a very remote possibility at best, because lymph node tuberculosis is supposed to be non-contagious and there was history of casual exposure only. The presence of multiple skin lesions on exposed parts of the body from head-to-toe points toward possibility of acquisition of infection through contaminated body of stray dogs and autoinoculation from one site to another. The patient does not remember any contact with open wound of pup dogs but she was a dog rescuer and used to take care of them in every way. Genomic sequencing is a pre-requisite for the epidemiological linking of dogs and human cases which could not be done in our case.
The standard guidelines for the treatment of cutaneous tuberculosis consist of 2 months of intensive phase with four drugs (RHZE) and continuation phase of three drugs (RHE).[8] In the present case, the total duration of treatment was 6 months with 3 months of Intensive phase with four drugs (RHZE) and 3 months of continuation phase with three drugs (RHE) because when pyrazinamide was discontinued after 2 months, the patient again developed some discharge from the hand lesion. Hence, pyrazinamide was administered for 1 more month.
In Indian literature, there are case reports and case series of cutaneous tuberculosis in immunocompetent and immunocompromised individuals mainly diagnosed histopathologically.[9-11] Our case is unique as cutaneous tuberculosis is microbiologically proven in an immunocompetent patient with complete resolution of lesion after treatment and dogs being the possibility of source of infection.
CONCLUSION
Cutaneous tuberculosis in an immunocompetent individual is a rare condition and may masquerade with many dermatological conditions leading to difficult diagnosis due to varied morphology, paucibacillary nature, and unavailability of diagnostic techniques to diagnose tuberculosis. It is very important to microbiologically confirm cutaneous tuberculosis for the definitive treatment and to prevent unnecessary surgical interventions. Transmission of cutaneous tuberculosis from animals to human being by contiguous route is an area of research and should be explored.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Cutaneous tuberculosis In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482220 [Last accessed on 2024 May 23]
- [Google Scholar]
- Cutaneous tuberculosis-A practical case report and review for the dermatologist. J Clin Aesthetic Dermatol. 2009;2:19-27.
- [Google Scholar]
- Cutaneous tuberculosis: Epidemiologic, etiopathogenic and clinical aspects-part I. An Bras Dermatol. 2014;89:219-28.
- [CrossRef] [PubMed] [Google Scholar]
- Tuberculosis exposure from a dog by Scott Weese. 2010. Available from: https://www.wormsandgermsblog.com/2010/12/articles/animals/dogs/tuberculosis-exposure-from-a-dog [Last accessed on 2024 May 23]
- [Google Scholar]
- Mycobacterium tuberculosis transmission from human to canine. Emerg Infect Dis. 2002;10:2258-60.
- [CrossRef] [PubMed] [Google Scholar]
- Index-TB guidelines- guidelines on extra-pulmonary tuberculosis for India Geneva: World Health Organization; 2016.
- [Google Scholar]
- Varied presentation of cutaneous tuberculosis in a patient. Indian J Dermatopathol Diagn Dermatol. 2020;7:36-7.
- [CrossRef] [Google Scholar]
- An interesting case report of cutaneous tuberculosis of the foot. Int J Surg Case Rep. 2022;100:107763.
- [CrossRef] [PubMed] [Google Scholar]
- Atypical presentations of cutaneous tuberculosis: Series of 10 cases. Indian J Tuberc. 2022;69:113-9.
- [CrossRef] [PubMed] [Google Scholar]






