Translate this page into:
Seminoma with intertubular growth pattern: A tumor with ambiguous clinical and gross morphology

*Corresponding author: Mohammed Al-Masqari, Department of Histopathology, The Royal Hospital, Muscat, Oman. mme9090@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Al-Masqari M, Al Hamdani A. Seminoma with intertubular growth pattern: A tumor with ambiguous clinical and gross morphology. Indian J Med Sci 2021;73(1):121-3.
Abstract
Seminoma constitutes around 30–40% of all testicular tumors. Intertubular seminoma signifies a distinct subtype and a rare growth pattern of seminoma. This type of tumor is usually discovered incidentally during microscopic examination since the lesion is inapparent clinically and macroscopically. It is characterized by distribution of seminoma cells between the seminiferous tubules. Hence, if careful microscopic examination is not performed, the intertubular seminoma can be missed. We report a case of Seminoma with exclusive intertubular growth pattern.
Keywords
Seminoma
Pathology
Urology
Testis
Tumor
INTRODUCTION
Testicular cancer is the most common cancer in men under the age of 45. Seminoma is the most common testicular tumor which is usually present with painless testicular enlargement. Histologically, seminoma can exhibit many morphological patterns which are not significant clinically. However, these patterns can pose diagnostic difficulties to pathologists. Since seminoma with intertubular growth pattern is clinically and histologically occult, awareness of this morphological pattern and careful microscopic examination is the only way to detect this ambiguous growth pattern.
CASE REPORT
A 21-year-old Omani gentleman was found to have undescended right testis during general medical checkup. Subsequently, he was referred to Sultan Qaboos University Hospital for further management. He undergone orchiectomy for unilateral intra-abdominal testis and the specimen was sent to pathology laboratory for histopathological examination.
HISTOPATHOLOGY
Macroscopic findings
Received is a specimen of the right testis with an attached spermatic cord. External examination of the specimen is unremarkable. The testis is bisected and shows atrophic testicular parenchyma with no evidence of gross lesions. Representative sections from the testis were taken for histopathological examination.
Microscopic findings
The hematoxylin and eosin (H&E) stained slides from the initial sections show extensive atrophy of the seminiferous tubules with germ cell neoplasia in situ, stromal fibrosis, and stromal infiltration by lymphocytes [Figure 1]. However, careful examination of the H&E stained sections revealed patchy areas with scattered intertubular large atypical cells exhibiting clear cytoplasm, large vesicular nuclei, and prominent nucleoli [Figure 2]. Some of these cells were seen in cords and small clusters intermingled with and obscured by the stromal lymphocytes. Immunohistochemistry studies were performed and show strong positivity for CD117, placental alkaline phosphatase (PLAP), and OCT3/4 supporting the diagnosis of intertubular seminoma [Figures 3a and b]. More sections were examined from the rest of the testis and show identical features. The tumor was confined to the testis and spermatic cord resection margin was negative.
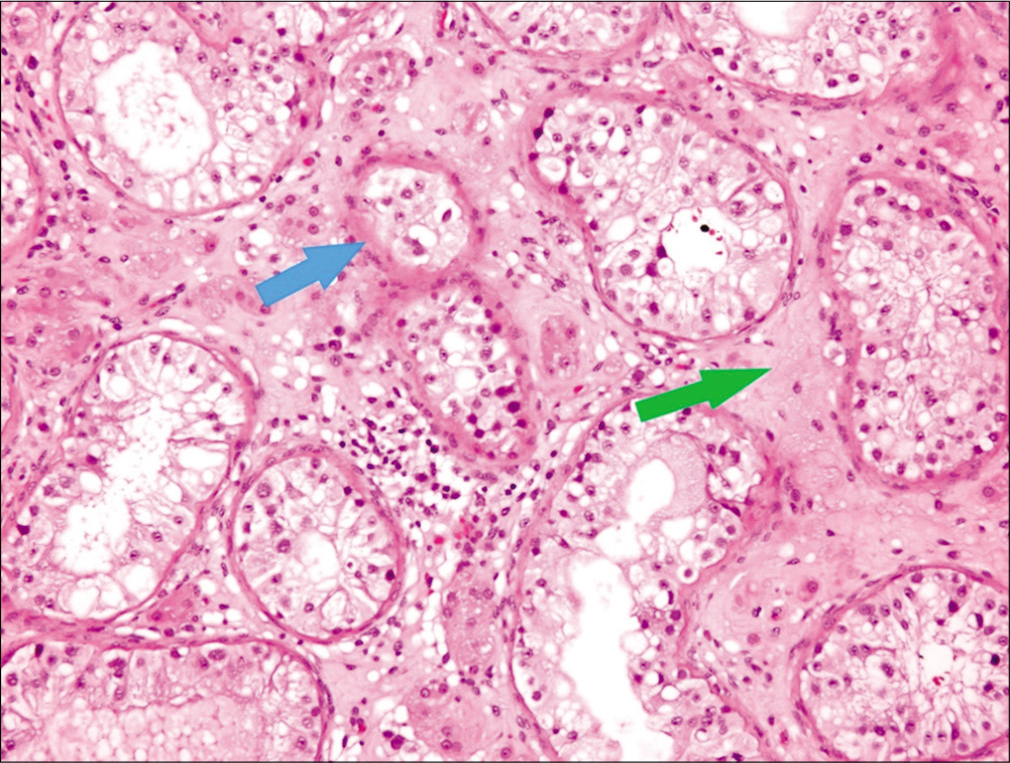
- H&E stained slide ×10 showing atrophic seminiferous tubules (blue arrow) and peritubular fibrosis (green arrow).
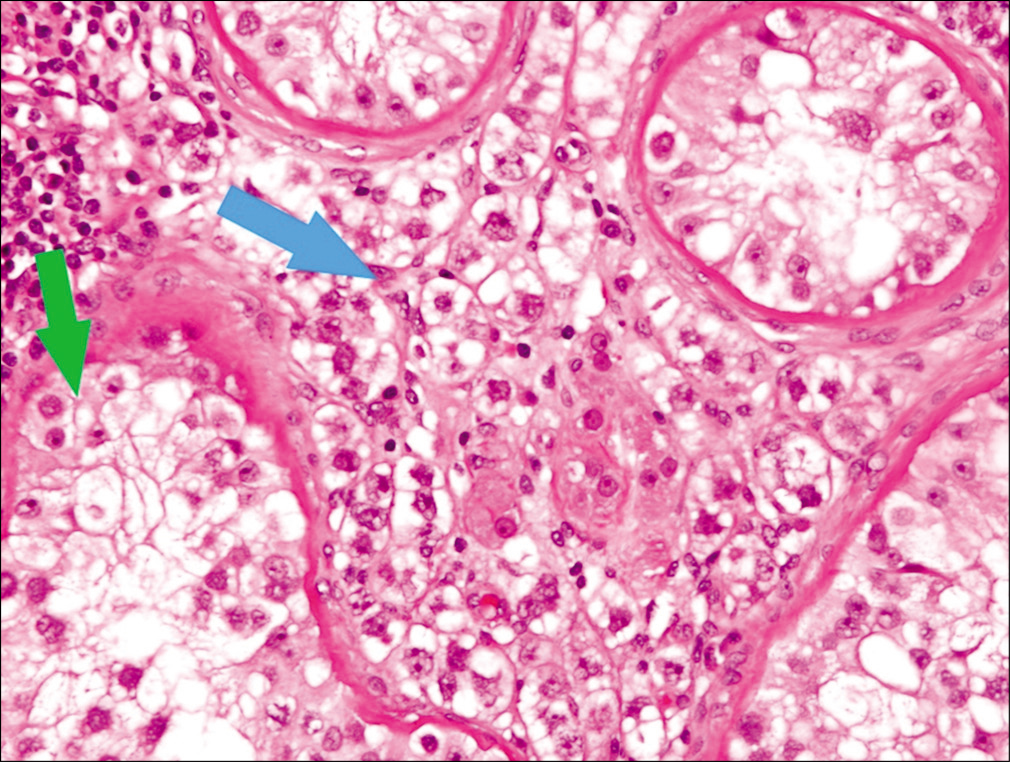
- H&E stained slide ×20 showing intertubular seminoma cells (blue arrow) and intratubular germ cell neoplasia (green arrow).
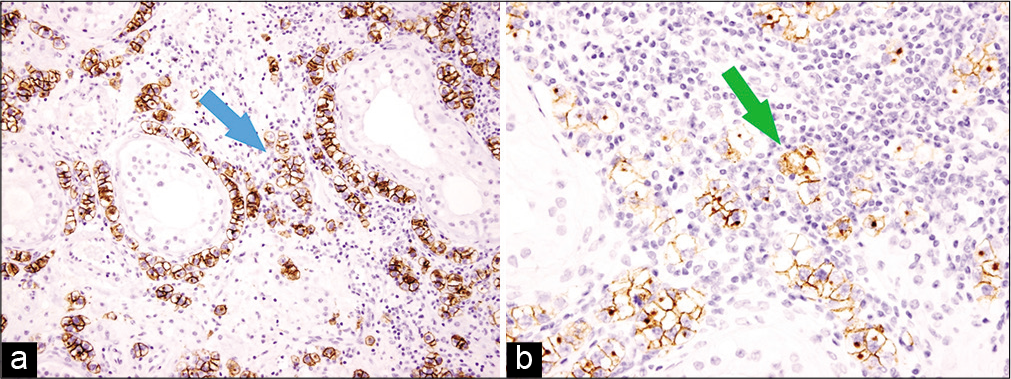
- Immunohistochemistry, ×40 showing intertubular tumor cells surrounded by stromal lymphocytes highlighted by CD117 (blue arrow, a) and placental alkaline phosphatase (green arrow, b).
DISCUSSION
Intertubular seminoma can be seen in association with classical seminoma or in a pure form.[1] The literature on seminoma with exclusive intertubular growth pattern is limited with only few published case reports. In contrast to classic seminoma which usually presents with clinically and grossly large testis, the testis in intertubular seminoma is normal or small.[2] In the largest case series of intertubular seminoma, 9 out of 11 cases showed no visible macroscopic tumor and two demonstrated ill-defined firm area or foci of whitish-brown discoloration.[3] Histologically, some of the reported cases including this case show moderate intertubular lymphocytic infiltrate which obscure the tumor cells making the diagnosis more difficult. Hence, such cases might be misdiagnosed as chronic orchitis. The combination of germ cell neoplasia in situ and chronic interstitial inflammation should raise concerns about presence of intertubular seminoma. Immunohistochemistry studies with PLAP and CD117 stains are very helpful markers in these cases since they highlight the seminoma cells especially those hidden within the stromal lymphocytosis. Although the tumor cells in intertubular seminoma are considerably less than the cells seen in conventional seminoma, cases with systemic metastasis were reported.[3] Moreover, it is also found that the concurrence of intertubular seminoma with classical seminoma is highly associated with rete testis invasion; hence, it is an important prognostic factor.[4]
CONCLUSION
Seminoma with exclusive intertubular growth pattern is a rare and unique clinicopathological entity. We suggest that careful examination of all sections should be carried out to identify this clinically occult and grossly inapparent tumor. Furthermore, the diagnosis of intertubular seminoma should be suspected in atrophic testis showing a dense interstitial lymphocytosis requiring careful search for atypical seminoma cells.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Intertubular growth in pure seminomas: Associations with poor prognostic parameters. Hum Pathol. 2005;36:640-5.
- [CrossRef] [PubMed] [Google Scholar]
- Seminoma with intertubular growth pattern: A clinically and grossly inapparent testicular tumour. Diagn Histopathol. 2009;15:104-6.
- [CrossRef] [Google Scholar]
- Seminomas with exclusive intertubular growth: A report of 12 clinically and grossly inconspicuous tumors. Am J Surg Pathol. 2004;28:1163-8.
- [CrossRef] [PubMed] [Google Scholar]
- Rosai and Ackerman's Surgical Pathology (10th ed). Edinburgh: Mosby Elsevier; 2011.
- [Google Scholar]






