Translate this page into:
Sentinel lymph node biopsy versus complete axillary dissection in breast cancer: Oncological outcomes and lifestyle improvements – An Iraqi perspective
*Corresponding author: Aqeel Shakir Mahmood, Department of Surgery, College of Medicine, University of Baghdad, Baghdad, Iraq. aqeel.shakir.mahmood@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mahmood AS, Sfyyih AN, Ahmed HA, Hussein RJ, Turkey FA, Kamal MS, et al. Sentinel lymph node biopsy versus complete axillary dissection in breast cancer: Oncological outcomes and lifestyle improvements – An Iraqi perspective. Indian J Med Sci. 2025;77:18-23. doi: 10.25259/IJMS_260_2024
Abstract
Objectives
To evaluate and compare the impact of ALND and SLNB on the oncological outcomes of BC patients.
Materials and Methods
This is a prospective cohort study that included 160 patients with breast carcinoma who were scheduled to receive total axillary dissection. Patients were randomly assigned to undergo, together with breast surgery, either SLNB and ALND or SLNB followed by ALND only if the SLN was found positive. Follow-up included clinical examination every 4 months for the first 3 years, every 6 months for the following 2 years, and once a year thereafter. A mammography was scheduled annually.
Results
After 6 months follow-up, eight types of complications were reported. In particular, lymphedema was reported in 4 women (5%) among sentinel LN group and 17 women (21.25%) in complete dissection group, with a highly significant difference. Collectively, 31 women (38.75%) among axillary dissection group had one or more complications compared with 17 women (21.25%) among sentinel LN group who had such complications with a significant difference. In multivariate analysis, each of older age (odds ratio [OR] = 2.62, 95% confidence interval [CI] = 1.24–10.86, P = 0.027), T2 tumor stage (OR = 11.3, 95% CI = 1.06–19.9, P = 0.044), and ALND (OR = 3.2, 95% CI = 1.12–5.31, P = 0.042) were significantly associated with increase the incidence of post-operative complications.
Conclusion
SLNB is a highly efficient technique for evaluating the stage of the early BC. It is associated with less complication after surgery when compared to ALND. Increased post-operative complications in BC patients, whether handled with SLNB or ALND, are independently linked with advanced age and tumor stage.
Keywords
Sentinel lymph node biopsy
Axillary lymph node dissection
Breast cancer oncological outcomes
Post-operative complications
Iraqi breast cancer management
INTRODUCTION
The second most common cause of global cancer incidence in 2022 is female breast cancer (BC), which accounts for 11.6% of all cancer cases and is estimated to have 2.3 million new cases.[1] Between 2000 and 2019, a total of 72,022 BC cases were identified in women in Iraq. In fact, BC is the primary cause of mortality among Iraqi women, accounting for approximately one-third of all cancer cases recorded in the country.[2] Surgery is a crucial component of the comprehensive treatment strategy for the early-stage BC.[3] Advancements in surgical techniques have improved the esthetic outcomes of breast conservation and reconstruction procedures for women after mastectomy.[4]
The sentinel lymph node (SLN) is the first node to which cancer metastases spread. A biopsy is indicated for every invasive and micro-invasive breast carcinoma, and for Ductal Carcinoma in situ, but only when a mastectomy is done. Definite indications for SLN biopsy (SLNB) include largely early stage T1 and T2 carcinomas, while contraindications are inflammatory, ulcerated, and skin infiltrating carcinomas. In BC staging, T1 refers to a tumor that is up to 2 cm in size, while T2 refers to a tumor that is more than 2 cm but not more than 5 cm in its greatest dimension.
Sentinel biopsy is not suggested in malignant stromal breast tumors, as they disseminate hematogenously.[5] Recent guidelines state that axillary dissection is unnecessary if the SLN is negative. Research has indicated that axillary irradiation offers comparable results to axillary dissection, but without the added negative effects, such as lymphedema, which are commonly linked with surgical dissection.[6] Axillary lymphadenectomy is a surgical operation that involves the removal of the bottom two layers of axillary lymph nodes (LNs).[7]
In the context of Iraqi BC patients, the purpose of this study is to examine the impact of total axillary LN dissection (ALND) in comparison to SLN metastases on the oncological prognosis of the patients.
MATERIALS AND METHODS
Study design and settings
This study is a prospective cohort investigation that involved 160 patients diagnosed with breast carcinoma. These patients were selected based on established criteria[8] and were scheduled to undergo total axillary dissection at the Department of Surgery/Baghdad Medical City between August 01, 2018, and April 01, 2021. The study received approval from the Arabic Council of Medical Specializations. The inclusion criteria consisted of patients who had been diagnosed with unilateral BC and had no unsuspicious nodal status in clinical examination and sonogram. These patients also had a clinical rationale for primary BC surgery, which involved performing a SLNB followed by ALND. The exclusion criteria encompassed those who had undergone prior surgery on the ipsilateral breast or axilla, patients with chronic life-threatening conditions that could potentially hinder adjuvant therapy, pregnant or lactating individuals, those with non-infiltrating cancer, and individuals who had previously undergone excision biopsy of the breast. Patients were assigned in a random manner to have either SLNB with ALND, or SLNB followed by ALND if the SLN is found to be positive.
Ethical consideration
A written consent from each participant was obtained before data collection after explaining the aim of study. Each patient was given the complete unconditioned choice to withdraw anytime. The confidentiality of data throughout the study was guaranteed and the patients were assured that data will be used for research purpose only.
Identification of SLN
The administration of methylene blue injection was employed to identify and assess the SLN. An amount of approximately 5 mL of this dye was administered through injection into the peri-tumoral region, specifically in all four quadrants. Subsequently, a massage was performed on the area encompassing the tumor for 5 min, directed toward the axilla. Based on the tumor stage, either a modified radical mastectomy or breast conserving surgery was performed. SLNs were identified and removed during axillary dissection. The SLNs that were obtained were analyzed using the frozen section technique. Subsequently, both the SLN and axillary dissection specimens were evaluated using histological techniques.
Surgery, adjuvant therapy, and follow-up
Patients who underwent surgery had radiotherapy to the ipsilateral breast (50-Gy dose over 8 weeks). However, the axilla did not have radiotherapy. The protocol of adjuvant chemo- and/or hormone therapy was determined according to the main prognostic factors of the primary tumor. These included tumor size and grading, nodal status, and hormonal receptor status. Patients were followed for 1 year, during which clinical examination was performed every 4 months.
Statistical analysis
Statistical analysis was carried out using the Statistical Package for the Social Sciences (SPSS), version 25 (SPSS Inc., Chicago, Illinois, USA). Quantitative variables were expressed as mean and standard deviation (SD), while categorical variables were expressed as frequencies and percentage. Student‘s t-test were used to compare quantitative variables and χ2-test was used to compare the categorical variables. The level of statistical significance was set at P ≤ 0.05. Mammography was scheduled annually.
RESULTS
Demographic characteristics of the patients
The mean age of women in sentinel LN group was 47.48 ± 8.82 years (range 34–65 years) which was lower than that of women in complete dissection group (mean= 52.48 ± 10.71, range 32–70 years) with a highly significant difference [Figure 1]. Postmenopausal women were more frequent in complete dissection than sentinel LN group (52, 65% vs. 40, 50%) with a difference very close to significant [Figure 2].
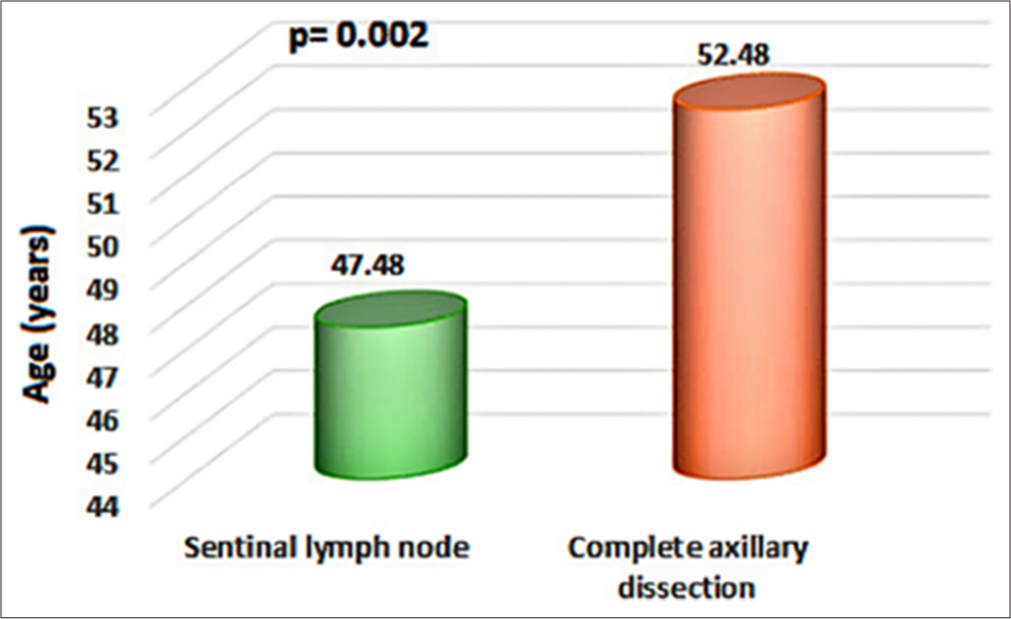
- Mean age of women in sentinel lymph node (SLN) and complete dissection groups. Green: Mean age of SLN group, Red: Mean age of Complete axillary dissection group.
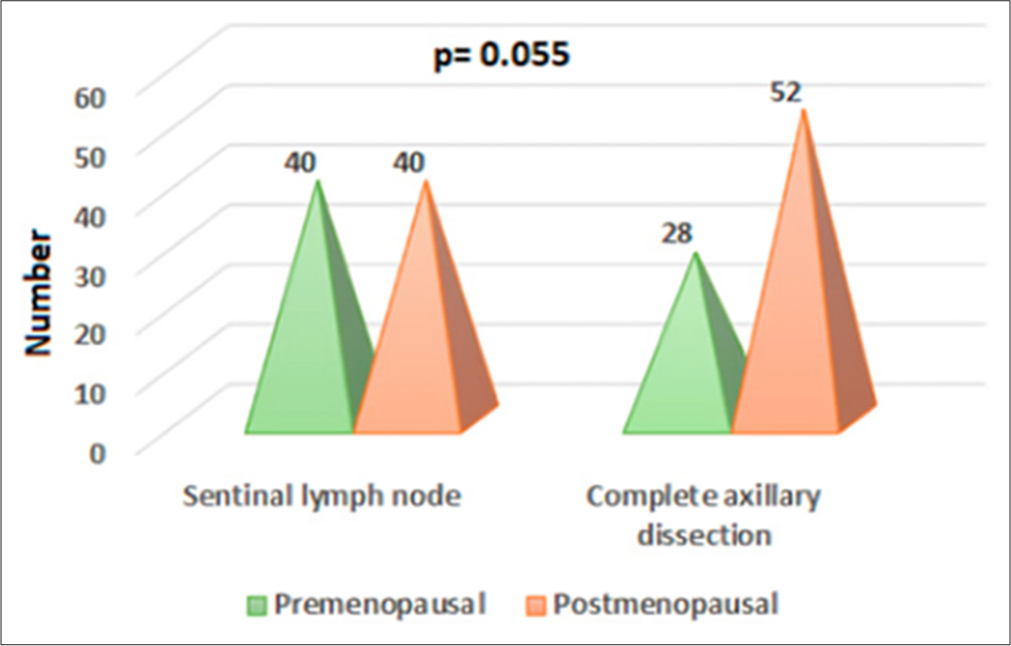
- Menopausal status in sentinel lymph node (SLN) and complete dissection groups.
Clinical characteristics of the patients
The two groups were comparable in the side of tumor and positivity of LNs with no significant difference. However, more advance stage of the tumor (T2) was more common in complete dissection than sentinel LN group (33.75% vs. 21%), although the difference exceeded the acceptable limit of significance [Table 1].
| Variables | Sentinel LN (n=80) | Complete axillary dissection (n=80) | P value |
|---|---|---|---|
| Side of tumor | |||
| Right | 48 (60%) | 44 (55%) | 0.522 |
| Left | 32 (40%) | 36 (45%) | 0.522 |
| Stage of breast cancer | |||
| T1a | 4 (5%) | 3 (3.75%) | 0.699 |
| T1b | 18 (22.5%) | 17 (21.25%) | 0.848 |
| T1c | 41 (51.25%) | 33 (41.25%) | 0.205 |
| T2 | 17 (21.25%) | 27 (33.75%) | 0.077 |
| Lymph node result | |||
| Negative | 58 (72.5%) | 53 (66.25%) | 0.391 |
| Positive | 22 (27.5%) | 27 (33.75%) | 0.391 |
LN: Lymph node
In the setting of BC staging, T1 describes a tumor that is 2 cm or less in its greatest dimension. It is subdivided into: T1a: Tumor not larger than 1 cm; T1b: Tumor larger than 1 cm but not larger than 2 cm; and T1c: Tumor larger than 2 cm but not larger than 2 cm. On the other hand, T2 describes a tumor that is more than 2 cm but not more than 5 cm in its greatest dimension. These classifications are helpful in describing the extent of the tumor, which is very important in staging the cancer and planning treatment strategies.
Post-operative complications
After 6 months follow-up, eight types of complications were reported. In particular, lymphedema was reported in 4 women (5%) among sentinel LN group and 17 women (21.25%) in complete dissection group, with a highly significant difference. Although infection, numbness, seroma, and axillary vein thrombophlebitis were more common among women in axillary dissection group (10%, 5%, 11.25%, and 3.75%, respectively) than women in sentinel LN group (3.75%, 3.75%, 7.5%, and 2.5%, respectively), the differences were not significant [Table 2].
| Variables | Sentinel LN (n=80) | Complete axillary dissection (n=80) | P value |
|---|---|---|---|
| Lymphedema | |||
| No | 76 (95%) | 63 (78.75%) | 0.002* |
| Yes | 4 (5%) | 17 (21.25%) | |
| Infection | |||
| No | 77 (96.25%) | 72 (90%) | 0.118 |
| Yes | 3 (3.75%) | 8 (10%) | |
| Numbness | |||
| No | 77 (96.25%) | 76 (95%) | 0.699 |
| Yes | 3 (3.75%) | 4 (5%) | |
| Seroma | |||
| No | 74 (92.5%) | 71 (88.75%) | 0.416 |
| Yes | 6 (7.5%) | 9 (11.25%) | |
| Axillary vein thrombophlebitis | |||
| No | 78 (97.5%) | 77 (96.25%) | 0.650 |
| Yes | 2 (2.5%) | 3 (3.75%) | |
| Hematoma | |||
| No | 78 (97.5%) | 80 (100%) | 0.155 |
| Yes | 2 (2.5%) | 0 (0%) | |
| Dye allergy | |||
| No | 78 (97.5%) | 80 (100%) | 0.155 |
| Yes | 2 (2.5%) | 0 (0%) | |
| Winging of scapula | |||
| No | 80 (100%) | 79 (98.75%) | 0.316 |
| Yes | 0 (0%) | 1 (1.25%) | |
LN: Lymph node, The asterisk (*) indicates statistical significance (P< 0.05)
Overall complications
Collectively, 31 women (38.75%) among axillary dissection group had one or more complications compared with 17 women (21.25%) among SLNB group who had such complications with a significant difference [Figure 3].
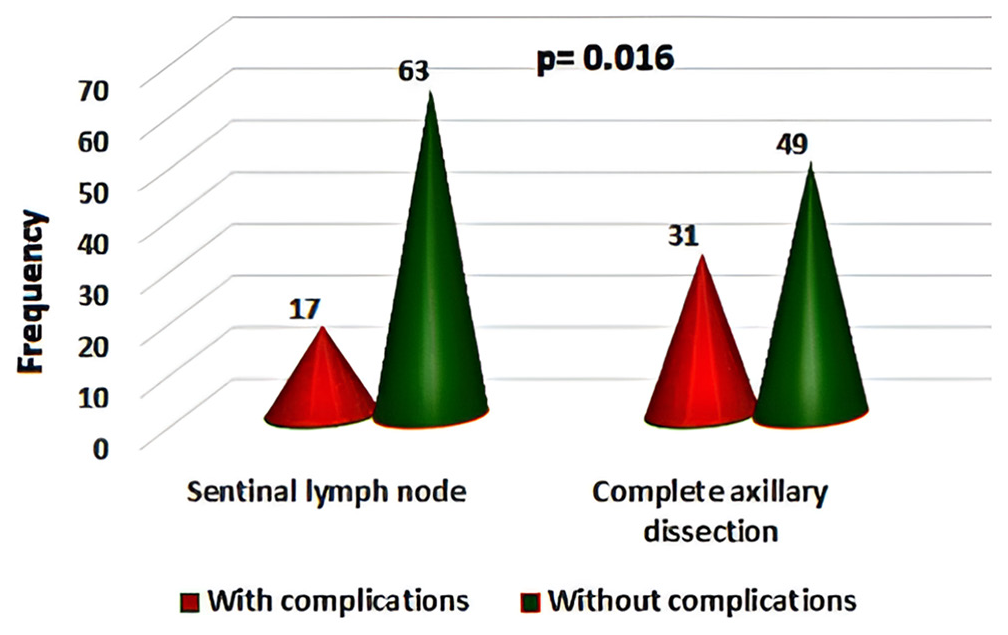
- The overall post-operative complications in sentinel lymph node and complete dissection groups.
Multivariate analysis
To find out if the SLN dissection is protective against postoperative complication, or the result just because the difference in age and menopausal status between the two groups, multivariate analysis was used. In this analysis, age was divided into two categories. In addition, menopausal state and tumor stage were included in the model [Table 3]. Older age (≥50 years) was significantly associated increased post-operative complication regardless of management (odds ratio [OR] = 2.62, 95% confidence interval [CI] = 1.24–10.86, P = 0.027). Furthermore, two-third (66.67%) of patients with complication had T2 tumor stage compared with only 10.71% of patients without complications who had this stage with a significant difference (OR = 11.3, 95% CI = 1.06–19.9, P = 0.044). Finally, 64.58% of patients with 16 complication were managed with complete axillary dissection versus 43.7% of patients without complications with a significant difference (OR= 3.2, 95% CI = 1.12–5.31, P = 0.042). Thus, SLN is independent protective factors against the development of post-operative complications. In contrast, menopausal status had no significant association with complications.
| Variables | Without complications (n=112) | With complications (n=48) | P value | OR (95%CI) |
|---|---|---|---|---|
| Age in years | ||||
| < 50 | 77 (68.75%) | 10 (20.83%) | 0.027* | 1.0 |
| ≥ 50 | 35 (31.25%) | 38 (79.17%) | 0.027* | 2.62 (1.24-10.86) |
| Menopausal status | ||||
| Premenopausal | 60 (53.57%) | 8 (16.67%) | 0.141 | 1.0 |
| Postmenopausal | 52 (46.43%) | 40 (83.33%) | 0.141 | 1.3 (0.42-6.03) |
| Stage | ||||
| T1a | 7 (6.25%) | 0 (0%) | 0.042* | 1.0 |
| T1b | 34 (30.36%) | 1 (2.08%) | 0.293 | 0.21 (0.01-3.86) |
| T1c | 59 (52.69%) | 15 (31.25%) | 0.658 | 1.65 (0.18-15.3) |
| T2 | 12 (10.71%) | 32 (66.67%) | 0.044* | 11.3 (1.06-19.9) |
| Management | ||||
| Sentinel LN | 63 (56.25%) | 17 (35.42%) | 0.042* | 1.0 |
| Axillary dissection | 49 (43.75%) | 31 (64.58%) | 0.042* | 3.2 (1.12-5.31) |
LN: Lymph node, OR: Odds ratio, CI: Confidence interval, The asterisk (*) indicates statistical significance
DISCUSSION
The present study found that the incidence of postoperative complications was considerably higher in the ALND group compared to the SLNB group. Specifically, the occurrence of lymphedema was more prevalent in after SLND + ALND (21.5%) compared to SLNB (5%), with a statistically significant distinction. Patients in the SLND combined with ALND group exhibited a higher incidence of wound infections, seromas, and numbness compared to those in the SLND alone group, with statistically significant disparities. These results are in line with many older studies. For instance, Fleissig et al.[9] and Wilke et al.[10] conducted extensive prospective clinical trials in the past, and both of them came to the same conclusion: Postoperative lymphoedema, whether measured subjectively or objectively, occurs in 6% of patients who are simply receiving SLND. On the other hand, in a different study that was conducted out by Glechner et al.,[11] which included 891 patients who were followed up to about 6 years after the procedure, post-ALND lymphedema was found in 11% of the patients. Moreover, a meta-analysis of four clinical trials demonstrated two primary outcomes associated with the implementation of SLNB. The survival rate of a patient with pathologically negative sentinel nodes is unchanged regardless of whether she receives total axillary dissection or sentinel node mapping. Furthermore, a significant number of patients have the potential to prevent the difficulties associated with these treatments, resulting in clear benefits in terms of both time and cost savings for the healthcare system.[12] These findings aligns with recent studies like Li et al.[13] study who investigated whether SLNB is a viable alternative to ALND for female patients with larger breast tumors. The study included 864 patients, with a mean follow-up period of 75 months. The overall survival was 78.2% for the SLNB group and 78.7% for the ALND group. Subgroup analyses based on age, TNM stage, BC subtypes, surgical approaches, radiation therapy, and chemotherapy showed no significant differences in survival outcomes between the two groups. This finding supports the use of SLNB to potentially avoid the higher morbidity associated with ALND, such as lymphedema, pain, and sensory loss, thus improving patients’ quality of life.
An additional benefit of SLNB is that it enables the pathologist to conduct a more comprehensive examination of one or a few LNs that are most likely to contain metastases, in contrast to LNs obtained through ALND. The presence of metastases that are not detected through classical hematoxylin and eosin staining can be easily detected through immuno-histochemical analysis.[12] Another potential clinical application of the SLNB is the staging of the axilla in patients who are candidates for neoadjuvant chemotherapy. Before initiating pre-operative chemotherapy, it is important to possess a basic understanding of the pathological state of the axillary LNs. This is due to the possibility that a negative result following the treatment could be the result of sterilization or a previous lack of involvement.[14] Furthermore, SLNB is a more cost-effective option compared to ALND. Verry et al.[15] formulated a model to calculate the expense of a SLNB in comparison to an ALND. According to the study, over a 20-year period, SLNB was found to be a more efficient and cost-effective method for staging compared to ALND. On evaluating individuals with a low likelihood of axillary metastases, it was determined that the advantages of skipping lymphedema treatment exceeded the potential minimal long-term risks associated with a false-negative SLNB incidence of 5.5%, resulting in a slight cost reduction of $883 per patient over a 20-year period. ALND is connected with extended hospitalization and higher risk of lymphedema.
In our study, it emerged that both age and tumor stage were independently associated with the occurrence of post-operative complications, along with the treatment decision. The OR for the development of complications in T2 patients was 11.3 (95% CI = 1.06–19.9). This indicates that patients in the T2 stage will have an 11.3-fold higher risk of developing a post-operative complication than those in the T1a stage. In a study conducted by Bokhari et al.,[16] the researchers examined the occurrence of early problems after breast surgery in 100 Pakistani patients. They reported that application complications were more common in older patients, in particular seroma, in comparison with younger patients. This may be related to other comorbidities compounded in the elderly, such as diabetes and hypertension. Moreover, Obadiel[17] also explored the postoperative complication rate in 50 Yemeni female patients with cancer of the breast who underwent surgery of the breast. Those during the advanced stages of the tumor were experiencing more of these issues than their counterparts in the early stages, irrespective of age, and adjuvant therapy. However, the authors failed to calculate the OR. The above trend can be explained because the patients presenting themselves at an advanced disease stage are subjected to more intrusive surgical interventions with extended hospital stays. In summary, findings from this study confirm the clinical advantages of SLNB over ALND in terms of minimalizing post-operative complications and enhancing patients’ quality of life. It is important in axillary staging, especially within the neoadjuvant chemotherapy setting; cost-effective; and lesser morbidity, making it a favored option in BC surgery. Further studies will need to refine these results and address long-term outcomes associated with the SLNB to further optimize BC management strategies.
CONCLUSION
In comparison to ALND, SLNB is a more effective technique to assess early BC and is associated with fewer postoperative complications. Advanced age and tumor stage are independent risk factors of increased post-operative complications following surgical intervention in BC treated with either SLNB or ALND.
These results confirm the recommendation of the routine performance of SLNB before axillary dissection in all stages, especially the early stages, of BC patients. This study is the first in Iraq comparing SLNB with ALND, so more studies should be done to gather more data and further results.
Ethical approval
This study was conducted as part of the mandatory training and research duties assigned to board residents under the supervision of the Iraqi Board for Medical Specializations and experienced surgical specialists. At the time of conducting the study, formal approval from an ethics committee was not a requirement, as the research was integrated into the standard clinical training framework. The certification provided by the examining committee serves as confirmation of compliance with institutional standards and oversight. Institutional Review Board (IRB) approval was subsequently obtained specifically for publication purposes, ensuring alignment with international ethical standards.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394-424.
- [CrossRef] [PubMed] [Google Scholar]
- Trends in breast cancer incidence in Iraq during the period 2000-2019. Asian Pac J Cancer Prev. 2021;22:3889-96.
- [CrossRef] [PubMed] [Google Scholar]
- Sentinel lymph node biopsy for patients with early-stage breast cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2017;35:561-4.
- [CrossRef] [PubMed] [Google Scholar]
- Oncoplastic breast-conserving surgery for tumors larger than 2 centimeters: Is it oncologically safe? A matched-cohort analysis. Ann Surg Oncol. 2016;23:1852-9.
- [CrossRef] [Google Scholar]
- Sentinel lymph node as a new marker for therapeutic planning in breast cancer patients. J Surg Oncol. 2004;85:102-11.
- [CrossRef] [PubMed] [Google Scholar]
- Oncological safety of skipping axillary lymph node dissection in patients with clinical no, sentinel node-positive breast cancer undergoing total mastectomy. Ann Surg Oncol. 2024;31:3168-76.
- [CrossRef] [PubMed] [Google Scholar]
- Axillary nodal burden in breast cancer patients with pre-operative fine needle aspiration-proven positive lymph nodes compared to those with positive sentinel nodes. In Vivo. 2020;34:729-34.
- [CrossRef] [PubMed] [Google Scholar]
- Invasive breast cancer version 1.2016, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw. 2016;14:324-54.
- [CrossRef] [PubMed] [Google Scholar]
- Post-operative arm morbidity and quality of life. Results of the ALMANAC randomised trial comparing sentinel node biopsy with standard axillary treatment in the management of patients with early breast cancer. Breast Cancer Res Treat. 2006;95:279-93.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical complications associated with sentinel lymph node biopsy: Results from a prospective international cooperative group trial. Ann Surg Oncol. 2006;13:491-500.
- [CrossRef] [PubMed] [Google Scholar]
- Sentinel lymph node dissection only versus complete axillary lymph node dissection in early invasive breast cancer: A systematic review and meta-analysis. Eur J Cancer. 2013;49:812-25.
- [CrossRef] [PubMed] [Google Scholar]
- Axillary dissection compared to sentinel node biopsy for the treatment of pathologically node-negative breast cancer: A meta-analysis of four randomized trials with long-term follow up. Oncol Rev. 2012;6:e20.
- [CrossRef] [PubMed] [Google Scholar]
- Survival after sentinel lymph node biopsy compared with axillary lymph node dissection for female patients with T3-4c breast cancer. Oncologist. 2023;28:e591-9.
- [CrossRef] [PubMed] [Google Scholar]
- Axillary staging in node-positive breast cancer converting to node negativity through neoadjuvant chemotherapy: Current evidence and perspectives. Scand J Surg. 2023;112:117-25.
- [CrossRef] [PubMed] [Google Scholar]
- Effectiveness and cost-effectiveness of sentinel lymph node biopsy compared with axillary node dissection in patients with early-stage breast cancer: A decision model analysis. Br J Cancer. 2012;106:1045-52.
- [CrossRef] [PubMed] [Google Scholar]
- Early complications of mastectomy with axillary clearance in patients with stage II and III carcinoma breast. J Surg Pak (Int). 2010;15:182-5.
- [Google Scholar]
- Early complications following modified radical mastectomy-among breast cancer patients admitted to AL Gomhory teaching hospital, Sana'a, Yemen between Jan. 2019-Jan. 2020. Open Access Libr J. 2020;7:e6992.
- [CrossRef] [Google Scholar]






