Translate this page into:
Severe impact of COVID-19 pandemic on non-COVID patient care and health delivery: An observational study from a large multispecialty hospital of India
*Corresponding author: Raju Vaishya, Indraprastha Apollo Hospitals, Mathura Rd, Sarita Vihar, New Delhi, India. raju.vaishya@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Vaishya R, Sibal A, Kumar PS. Severe impact of COVID-19 pandemic on non-COVID patient care and health delivery: An observational study from a large multispecialty hospital of India. Indian J Med Sci 2021;73(2):159-63.
Abstract
Objectives:
The COVID-19 pandemic has severely impacted health-care delivery globally, especially for non-COVID diseases. These cases received suboptimal attention and care during the pandemic. In this observational cohort study, we have studied the impact of the COVID-19 pandemic on various aspects of medical and surgical practices.
Material and Methods:
This observational, cross-sectional cohort study was performed on the data of a 710 bedded, multispecialty, and tertiary care corporate hospital of the national capital of India. The data of the pandemic period (April 1, 2020–March 31, 2021) were divided into three main groups and were then compared with the patient data of the preceding non-pandemic year (April 1, 2019–March 31, 2020) of more than six hundred thousand cases.
Results:
From the data of 677,237 cases in these 2 years, we found a significant effect of COVID-19 pandemic on most spheres of clinical practice (P < 0.05), including outpatient attendance and surgical work. The specialties providing critical and emergency care were less affected. Although the total hospital admissions reduced by 34.07%, these were not statistically significant (P = 0.506), as the number of COVID-19 admissions took place during this time and compensated for the drop.
Conclusion:
The COVID-19 pandemic has significantly impacted health-care delivery to non-COVID cases across all the major medical and surgical specialties. Still, major urgent surgical and interventional work for cases was undertaken with due precautions, without waiting for the ongoing pandemic to end, as the delay in their treatment could have been catastrophic.
Keywords
COVID-19
Pandemic
Health care
India
Hospital
Clinical practice
INTRODUCTION
The COVID-19 pandemic has disrupted health-care delivery across the globe. It has been more than 1 year since its onset in India, and it has continued to spread through most parts of the world and is posing a profound impact on all the spheres of life, mainly health and health-care delivery.[1,2] COVID-19 was announced as a pandemic by the World Health Organization (WHO) on March 11, 2020.[3] It is still raging across the world, and India is witnessing a terrible second wave with an alarmingly increased number of cases and deaths despite the ongoing vaccination program.[4] The first case of COVID-19 in the national capital of India, Delhi, was seen on March 3, 2020,[3] and the Government of India imposed a nationwide lockdown from March 25, 2020, until May 31, 2020, in four phases.[5] These mandatory restrictions and ever-increasing COVID cases have had a significant impact on the health-care delivery to the cases in all the medical and surgical specialties. There was a substantial reorganization of the health-care delivery and infrastructure in combating this highly contagious and rapidly spreading viral disease. Several dedicated COVID hospital beds and entire hospitals were prepared for the increasing number of these cases. The guidelines and government rules and regulations were changed multiple times for the hospitals and health-care providers to follow, from time to time.
There have been some reports based on doctor’s surveys and institutional data on the impact of COVID-19 on various medical and surgical specialties across the globe.[6-15] In this observational cohort study of nearly six hundred thousand cases, we have studied in detail the impact of the COVID-19 pandemic on various medical and surgical specialties for the entire year of the pandemic and compared it with the preceding pre-pandemic period.
MATERIAL AND METHODS
This observational, cross-sectional cohort study was performed on the data of a 710 bedded, multispecialty, and tertiary care corporate hospital of the national capital of India.[16] We retrieved the cases’ data from our medical records department (MRD) of the past 2 years (April 1, 2019–March 30, 2021). The data of the pandemic period (April, 2020– March 31, 2021) were divided into three main groups and were then compared with the patient data of the preceding non-pandemic year (April 1, 2019–March 31, 2020):
Lockdown pandemic period (LPP) – April 1, 2020–May 31, 2020
Non-LPP – June 1, 2020–March 31, 2021
Full pandemic period – April 1, 2020–March 31, 2021.
Although the national lockdown in India was imposed from March 25 midnight until May 31, 2020, we included the data of the lockdown period from April 1, 2020.
We included the data of out patient’s attendance, hospital admissions, and the surgical work of all the major medical and surgical specialties. These data were compared between the pandemic year and the preceding non-pandemic year, to analyze the impact of COVID-19 pandemic on several parameters. We also investigated the admissions related to the COVID-19 during the pandemic.
The statistical analysis was performed using IBM-SPSS version 20.[17] The percentage change in the data was calculated between the similar times in the pandemic and pre-pandemic periods. Different variables were used in the study: New and follow-up (repeat) outpatient cases, hospital admissions and the surgery, etc. Paired t-test was used to find the comparison between the pre-pandemic and pandemic years. P < 0.05 was considered of statistical significance.
RESULTS
This study evaluated the data of 677,237 cases (599,281 out cases and 77,956 hospital admissions) in 2 years (pandemic and pre-pandemic years). We found that there was a significant effect of the COVID-19 pandemic on most spheres of clinical practice (P < 0.05), including the outpatient attendance and the surgical work [Table 1]. Both the new and follow-up out cases’ attendance dropped, with a total reduction of 57.65%. The surgeries were less by 43.78%, more so the minor surgeries (52.93%). Although the total hospital admissions reduced by 34.07%, these were not statistically significant (P = 0.506), as the number of COVID-19 admissions took place during this time and compensated for the drop.
| Patients | Pandemic year (1st April, 2020–31st March, 2021) | Pre-pandemic year (1st April, 2019–31st March, 2020) | Percentage change | P-value |
|---|---|---|---|---|
| Outpatients | ||||
| New | 72,201 | 161,756 | –55.36 | <.001 |
| Follow-ups | 106,119 | 259,205 | –59.06 | <.001 |
| Total | 178,320 | 420,961 | –57.65 | <.001 |
| Inpatients | ||||
| Admissions | 30,975 | 46,981 | –34.07 | 0.506 |
| Surgery | ||||
| Major | 7783 | 13,340 | –41.66 | <.001 |
| Minor | 1460 | 3102 | –52.93 | <.001 |
| Total | 9243 | 16,442 | –43.78 | <.001 |
The impact of lockdown (1st April, 2020–31st May, 2020) was more severe on all aspects of the clinical practice [Table 2]. There was a significant reduction in the out cases’ attendance (89.2%), hospital admissions (59.8%), and surgical work (80.75%). These findings were statistically highly significant with P < 0.05.
| Patients | Lockdown period (1st April, 2020–31st May, 2020) | Pre-pandemic year (1st April, 2019–31st May, 2019) | Percentage change | P-value |
|---|---|---|---|---|
| Outpatients | ||||
| New | 2901 | 27,233 | –89.31 | <.001 |
| Follow-ups | 5310 | 48,787 | –89.11 | <.001 |
| Total | 8211 | 76,020 | –89.20 | <.001 |
| Inpatients | ||||
| Admissions | 3287 | 8177 | –59.80 | <.001 |
| Surgery | ||||
| Major | 463 | 2472 | –81.27 | <.001 |
| Minor | 120 | 557 | –78.46 | <.001 |
| Total | 583 | 3029 | –80.75 | <.001 |
We also noticed recovery trends in all the clinical practice parameters after the lockdown was removed from 1st June, 2020 [Table 3]. The outpatients’ attendance, hospital admissions, and the number of surgery (both major and minor) improved gradually. These were not influenced negatively by the increasing number of COVID-19 cases’ admissions in the hospital and numbers in the city.
| Patients | Non-lockdown pandemic period (1st June, 2020–31st March, 2021) | Pre-pandemic year (1st June, 2019–31st March, 2020) | Percentage change | P-value |
|---|---|---|---|---|
| Outpatients | ||||
| New | 69,300 | 134,523 | –48.48 | <.001 |
| Follow-ups | 100,809 | 210,418 | –52.09 | <.001 |
| Total | 170,109 | 344,941 | –50.68 | <.001 |
| Inpatients | ||||
| Admissions | 27,688 | 38,804 | –28.65 | <.001 |
| Surgery | ||||
| Major | 7320 | 10,868 | –32.65 | <.001 |
| Minor | 1340 | 2545 | –47.35 | <.001 |
| Total | 8660 | 13,413 | –35.44 | <.001 |
In the pandemic period of 1 year (April 2020–March 2021), the number of admissions for COVID-19 was 3746. The COVID-19 admissions gradually increased in numbers as the pandemic grew, reaching its peak in November 2020 [Figure 1]. The number of admissions for COVID-19 cases accounted for 12.09% of the total number of admissions (30,975) in that year.
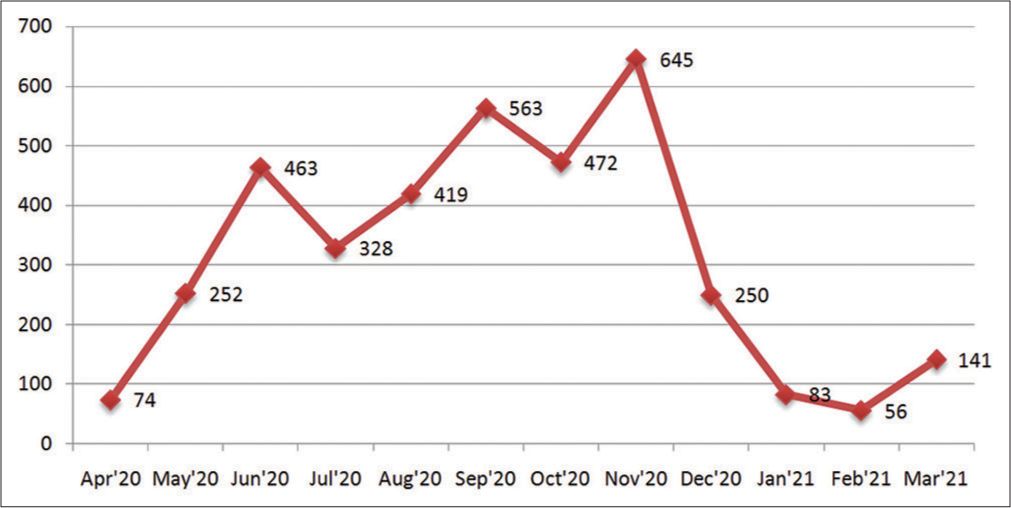
- Pattern of hospital admissions of COVID-19 cases in the pandemic period, over 1 year.
The COVID-19 pandemic has had a significant impact on both the hospital’s major medical and surgical specialties. All the medical specialties had reduced numbers of outpatients and admissions (between 35.11% and 76.92%). The only medical specialty of respiratory medicine saw a significant increase of 314.04%, in their admissions, because COVID-19 is primarily a respiratory disease.
The surgical work was reduced significantly across all the specialties, with bariatric surgery (87.5%) and ophthalmology (65.45%) were affected the most and general surgery (32.28%), and neurosurgery the least. We observed that all the medical and surgical specialties dealing more with critical and emergency care were less affected than the others. The most urgent surgical and interventional work for the required cases was undertaken with due precautions, such as liver (56.46%) and Kidney (54.89%) transplants, urgent neurosurgery (65.62%), cardiac surgery (44.56%), and surgical oncology (53.6%). However, there was an overall reduction of 40%, in the surgical specialties in the pandemic year.
DISCUSSION
During this pandemic, the focus of patient care was primarily shifted to the management of COVID-19 cases and medical or surgical emergencies, avoiding any non-emergency treatments. It has drastically changed health-care delivery practices. This ongoing pandemic is a major challenge for the health-care systems globally. Gomes et al. in a survey of 766 Brazilian urologists found a significant reduction of the outpatient visits, elective and emergency surgeries were reported by 83.2%, 89.6%, and 54.8%, respectively.[7] Vaishya et al. from the same institution have recently reported the impact of the COVID-19 pandemic on the orthopedics and trauma practice. They observed a significant reduction in outpatient attendance and orthopedic surgeries during the pandemic, especially during the lockdown period, with a drop in 90.77% and 84.63%, respectively.[9]
While the number of admissions for COVID-19 cases accounted for 12.09% of the total number of admissions in that year, due to several reasons, the number of non-COVID cases treated was to a lesser extent than the hospital would have liked. The hospital was asked to reserve 20–80% of the beds and ICUs at different times, as per Delhi government orders which decreased capacity for non-COVID work. In addition, many cases had reservations about coming for treatment for the fear of acquiring the infection in a health-care setting. There were also several travel restrictions during the lockdown period which did not allow cases to come to the hospital for neighboring states and other countries.
COVID-19 emergency had a direct and profound impact on the health-care delivery of non-COVID medical and surgical conditions. One of the worst affected groups was non-communicable diseases (NCDs), as these chronic diseases require continuous care. If not received, these cases may face devastating consequences in the long or short term. The NCDs are accountable for over 70% of all deaths. Approximately 80% of these deaths occur in low- and middle-income countries (LMICs), like India. In a survey of 155 countries, the WHO reported a significant disruption of prevention and treatment services for NCDs since the beginning of the COVID-19 pandemic. It affected the cases with other serious illnesses such as cancer, cardiac and kidney diseases, diabetes, and trauma care. These non-COVID cases were often unable to receive the required medical services, and these effects were found most pronounced in LMICs.[10]
Individuals with diabetes are at increased risk of severe COVID-19 and its complications due to multiple potential reasons, with up to 50% higher mortality rates reported.[18] Fersia et al. reported from a single-center study in the UK that the COVID-19 pandemic had a significant impact on their cardiology services, with more than 50% reduction in all the sections, including the patient’s footfalls, investigations, and treatment for various cardiac problems.[12] Ischemic heart disease is a leading cause of death globally. Hence, it has been suggested that the cardiology services need to prepare them for a significant increase in workload in the recovery phase and develop new strategies to help cases denied appropriate treatment during the pandemic period. As the lockdowns were taken away, the patient visits to the hospital for the required treatment gradually increased. Vaishya et al. have described a “lazy V-shaped” recovery in the number of cases attending the hospital after lifting the lockdown in India.[9] Similarly, cancer care is significantly affected by the pandemic. In a cross-sectional study of 356 centers from 54 countries, most of them (88.2%) reported facing challenges in delivering cancer care during the pandemic.[13] These authors have suggested that the cancer care continuum be effectively managed during pandemics or other major crises. In a retrospective study, from a cancer care center of the West India, it was noted that there was a substantial impact of the nationwide lockdown on the cancer care of patients, both in terms of reduced patient visits and the number of treatments received. The authors found that 4363 cancer patients visited hospital in the pre-lockdown period, compared to only 895 visiting during the lockdown period.[15]
The health-care delivery and resources are further constrained in the LMICs and are daunting. Several challenges exist, such as limited access to health care in remote areas, poverty, lack of education, and prevalent comorbid diseases have compounded the problems for the public and health-care providers in India.[15] Furthermore, many residents of LMICs cannot afford to miss work and rely on the daily wages for their living, and therefore cannot withstand any significant lockdowns.
There has been a noticeable impact of this pandemic on the economic and the health-care sectors globally. The health-care sector was found unprepared to deal with such a severe pandemic. Resumption of medical and surgical care in various specialties was done with caution, and different medical societies have formulated the guidelines for their members to follow.[19,20] The COVID-19 pandemic necessitated significant and rapid changes in our medical practices. Many of these changes may prove to “blessings in disguise” by adding value to care and creating opportunities to go forward.[21]
Limitations and strengths of the study
We only studied and analyzed the clinical aspects of the impact of the COVID-19 pandemic on various medical specialties. Different implications such as mortality, economic implications, healthcare providers’ safety, medical education, and research need to be studied in future studies. Since this study was done on the data of a large corporate, private hospital of the national capital of India, its findings may not apply to the government institutions, the smaller hospitals of India, and health care institutions overseas.
This unique study has looked at the impact of the pandemic for the entire year, including during the lockdown period, in a large tertiary care multispecialty hospital in India. Such an analysis of clinical data has not been done before for the full pandemic year and in such a large population of cases (more than six hundred thousand cases). The observations of this study should help the hospital administrators judiciously allocate their resources in the ongoing pandemic and future adverse health calamities.
CONCLUSION
The COVID-19 pandemic has had a significant impact on the health-care delivery to non-COVID cases across all the major medical and surgical specialties. The specialties that deal with critical and emergency care were less affected than the others. Major urgent surgical and interventional work for the required cases was undertaken with due precautions, such as liver and kidney transplants, urgent neurosurgery, cardiac surgery, and surgical oncology. These were done as life-saving measures, without waiting for the ongoing pandemic to end, as the delay to their treatment would have catastrophic. Resumption of clinical work should be done in a graded manner and with due precautions to safeguard the cases and health care workers engaged in their management.
Acknowledgment
We are grateful to Ms. Tanu Sharma of the MRD of our hospital for providing the required clinical data for our study. The help of Ms. Meenakshi Khatri was of immense help in analyzing the study’s data.
Authors’ contributions
RV: Concept, data collection and analysis, literature search, and manuscript writing AS: Concept, manuscript writing, data analysis, and editing PSK: Concept, manuscript writing, data analysis, and editing.
Ethical approval
Being a retrospective, observational study based on the hospital data and not disclosing the identity of any individuals, the ethical approval was not required.
Data sharing
We are ready to share the raw data with the journal for their assessment, as a supplementary file.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
All the authors are working for the Apollo Hospital, which is the same institution of this study.
References
- Effects of COVID 19 pandemic in daily life. Curr Med Res Pract. 2020;10:78-9.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of COVID-19 pandemic in the field of orthopaedics. J Clin Orthop Trauma. 2020;11:498-9.
- [CrossRef] [PubMed] [Google Scholar]
- WHO Announces COVID-19 Outbreak a Pandemic. https://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic [Last accessed on 2021 Apr 25]
- [Google Scholar]
- Covid-19: India sees new spike in cases despite vaccine rollout. BMJ. 2021;372:n854.
- [CrossRef] [PubMed] [Google Scholar]
- COVID-19 Lockdown in India. https://www.en.wikipedia.org/wiki/COVID-19_lockdown_in_India [Last accessed on 2021 Apr 25]
- [Google Scholar]
- Impact of COVID-19 on clinical practices during lockdown: A pan India survey of orthopaedic surgeons. Malaysian Orthop J. 2021;15:55-62.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of COVID-19 on clinical practice, income, health and lifestyle behavior of Brazilian urologists. Int Braz J Urol. 2020;46:1042-71.
- [CrossRef] [PubMed] [Google Scholar]
- The Impact of the COVID-19 pandemic on genitourinary cancer care: Re-envisioning the future. Eur Urol. 2020;78:731-42.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of COVID-19 on the practice of orthopaedics and trauma an epidemiological study of the full pandemic year of a tertiary care centre of New Delhi. Int Orthop. 2021;45:1391-7.
- [CrossRef] [PubMed] [Google Scholar]
- The Impact of the COVID-19 Pandemic on Noncommunicable Disease Resources and Services: Results of a Rapid Assessment. 2020. Geneva: World Health Organization; https://www.who.int/publications/i/item/ncds-covid-rapid-assessment [Last accessed on 2020 Sep 03]
- [Google Scholar]
- Impact of the COVID-19 pandemic on neurosurgical practice in India: Results of an anonymized national survey. Neurol India. 2020;68:595-602.
- [CrossRef] [PubMed] [Google Scholar]
- The impact of the COVID-19 pandemic on cardiology services. Open Heart. 2020;7:e001359.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of the COVID-19 pandemic on cancer care: A global collaborative study. JCO Glob Oncol. 2020;6:1428-38.
- [CrossRef] [PubMed] [Google Scholar]
- COVID-19 and orthopaedic surgeon: The Indian scenario. Trop Doct. 2020;50:108-10.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of nationwide lockdown on cancer care during COVID-19 pandemic: A retrospective analysis from Western India. Diabetes Metab Syndr. 2021;2021:1-8.
- [CrossRef] [PubMed] [Google Scholar]
- Indraprastha Apollo Hospital. Available from: https://www.delhi.apollohospitals.com/corporate/indraprastha-apollo-hospitals [Last accessed on 2021 Apr 25]
- [Google Scholar]
- IBM SPSS Statistics 27.0.0.0 Detailed System Requirements. https://www.ibm.com/software/reports/compatibility/clarity-reports/report/html/softwareReqsForProduct?deliverableId=DAE86200D8CC11E7AD0EC24C9513D95F [Last accessed on 2021 Jun 08]
- [Google Scholar]
- Diabetes care during COVID-19 lockdown at a tertiary care centre in India. Diabetes Res Clin Pract. 2020;66:108316.
- [CrossRef] [PubMed] [Google Scholar]
- Resuming elective surgery during the COVID-19 pandemic. J Bone Joint Surg Am. 2020;102:1205-12.
- [CrossRef] [PubMed] [Google Scholar]
- Resuming arthroplasty amidst the COVID-19 pandemic: A well aligned and a balanced approach. J Clin Orthop Trauma. 2020;11:423-5.
- [CrossRef] [PubMed] [Google Scholar]
- Learning opportunities from COVID-19 and future effects on health care system. Diabetes Metab Syndr. 2020;14:943-6.
- [CrossRef] [PubMed] [Google Scholar]






