Translate this page into:
Story of a superfluous muscle accessory soleus muscle sprain: Imaging and diagnostic approach!
*Corresponding author: Suvinay Saxena, Department of Diagnostic and Interventional Radiology, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India. suvinaysaxena@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Saxena S, Khera P, Rai B, Gonnade N. Story of a superfluous muscle accessory soleus muscle sprain: Imaging and diagnostic approach! Indian J Med Sci 2021;73(2):260-3.
Abstract
Accessory soleus muscle is a rare supererogatory variant, which presents as a mass in posterior compartment of ankle. It can present through a myriad of clinical features ranging from asymptomatic to sprain to complete tear. The pain with accessory soleus can be attributed to either compression of tibial nerve, exertional compartment syndrome and very rarely can be secondary to sprain or tears of the accessory soleus muscle. Very few cases have been documented with soleus muscle injuries. We would like to highlight the importance of imaging in diagnosis and management.
Keywords
Accessory soleus
Ultrasonography
Magnetic resonance imaging
Muscle injury
Sprain
INTRODUCTION
Accessory soleus muscle is a seldomly encountered congenital anatomical variation. It is also termed as soleus secundus or supernumerary soleus and has a prevalence in the range of 0.5–5.5%.[1,2]
Often is exists asymptomatically in patients, however if enlarged in bulk can present as mass like swelling along posterior medial ankle and lower leg. Imaging with radiographs, ultrasonography (USG), and magnetic resonance imaging (MRI) aids in diagnosis and assessment of the associated pathology and is an integral part of diagnostic work-up.
CASE REPORT
A 19-year-old boy presented to the hospital with complaints of the right foot pain for 6 months. The patient was training for army entrance and was regularly involved in athletic activities including running for 2 years. He gave a history of joining a training academy for 1 year, where he was involved in intensive physical activity averaging to more than 4 h/day. There was no history of direct trauma. On clinical examination, the patient had swelling along the posterior aspect of ankle, which increased on dorsiflexion of foot [Figure 1a,b]. The patient had full range of motion with slight tenderness along the lower aspect of the swelling. Clinical diagnosis of the right posterior tibialis posterior subluxation versus accessory soleus muscle was made, and the patient was referred to the department of radiology for diagnostic evaluation.
Radiograph of bilateral leg with foot revealed obliteration of Kager’s fat pad by a soft-tissue opacity on the right side. No evidence of cortical break, fracture, or dislocation was seen [Figure 1c].
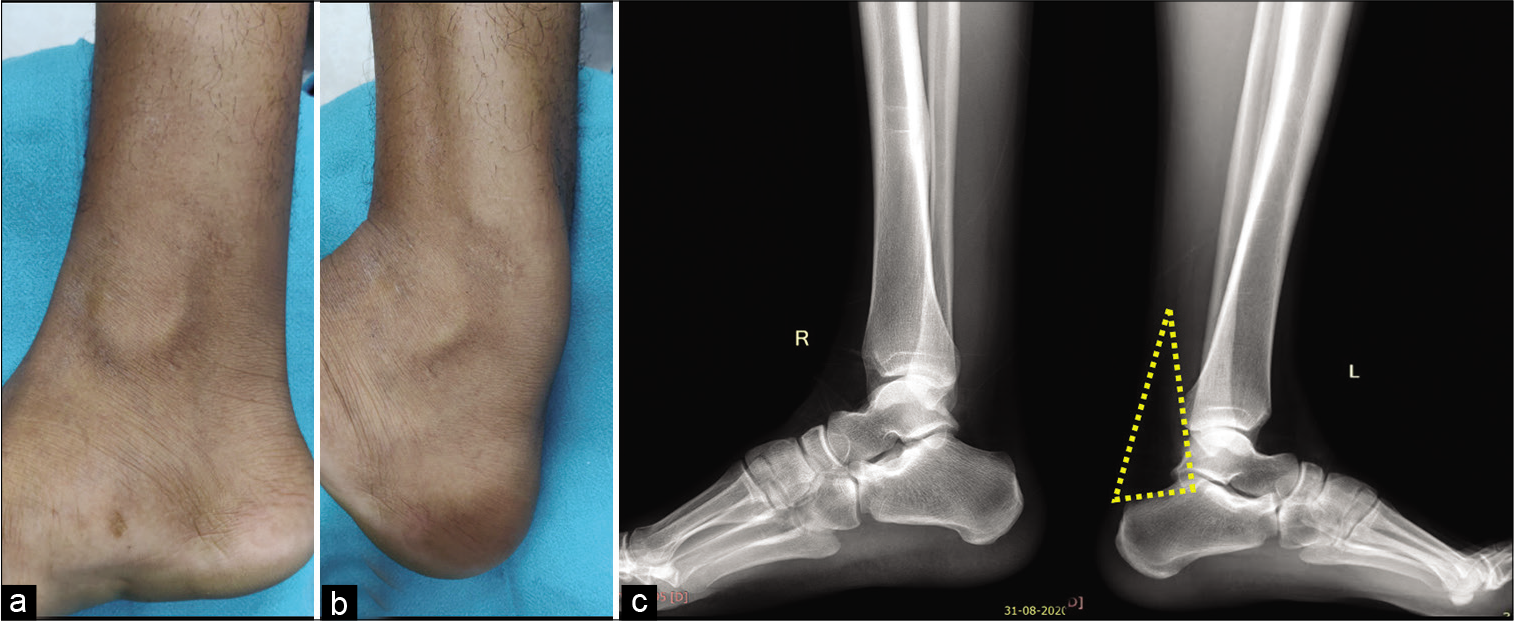
- Clinical examination reveals soft-tissue bulge along the medial aspect of leg and ankle on dorsiflexion (a and b). Lateral radiographs of both ankles with lower legs reveal obscuration of normal radiolucency of Kager’s fat pad on the right side (c).
Subsequently, highly resolution ultrasound (9–12 MHz) of ankle and leg was performed using linear probe which revealed the presence of an anomalous muscle situated in between the tendoachilles and posterior neurovascular bundle. The muscle belly was seen inserting into the medial aspect of the calcaneal tuberosity through a tendinous insertion [Figure 2a,b]. There was a presence of a focal area of hypoechogenicity along the myotendinous junction of this muscle involving less 5% area suggestive of Grade I sprain with minimal intrinsic serohematoma formation [Figure 2c]. Dynamic USG was performed which revealed no significant compression over the tibial nerve.
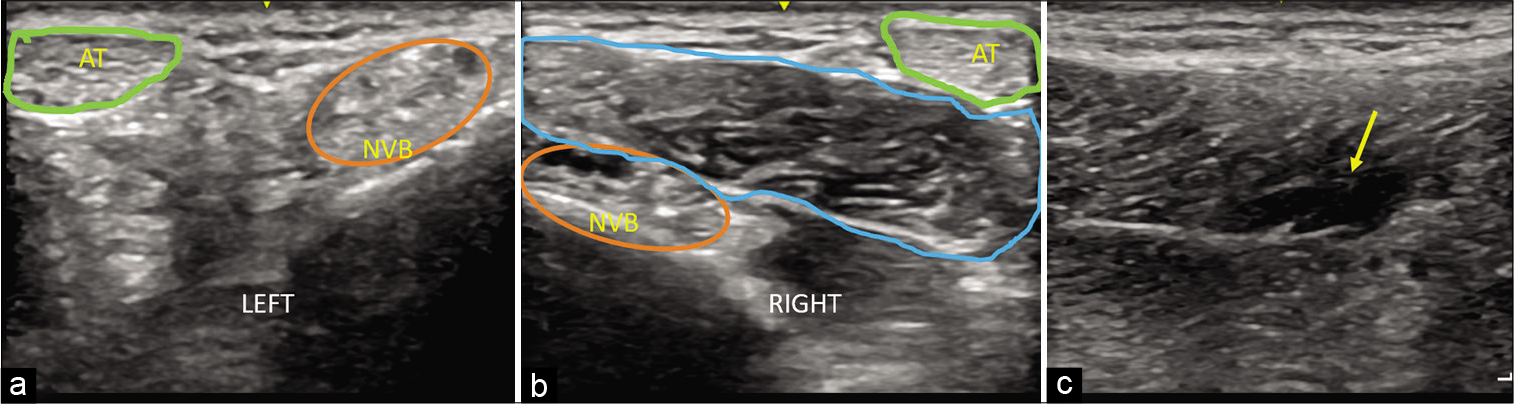
- High-frequency linear ultrasound transverse-oblique images along the postero-medial ankle (a) normal left side, (b) abnormal right side and (c) longitudinal scan right side. Green circle demarcates the Achilles tendon (AT), orange circle indicates the posterior tibial neurovascular bundle (NVB). There is presence of muscle like structure (blue circle) displacing AT and NVB on right side (2b). Longitudinal scan (c) along the right inferior myo-tendinous junction of the accessory soleus muscle shows ill-defined hypoechogenicity with loss of muscle fiber continuity (~5% muscle involvement) s/o sprain (yellow arrow).
MRI of the right ankle was performed which revealed the presence of a bulky muscle along the posteromedial compartment, with a tendinous insertion along medial aspect of calcaneum. It showed interfascicular edema along the lateral aspect with proton density fat-suppressed images (PDFS) revealing focal hyperintensity along the myotendinous junction, suggestive of Grade II sprain. There was focal PDFS hyperintensity along the muscle belly of flexor hallucis tendon suggestive of Grade I sprain. No abnormal hyperintensity was seen along the tibial nerve or along Achilles tendon [Figure 3].
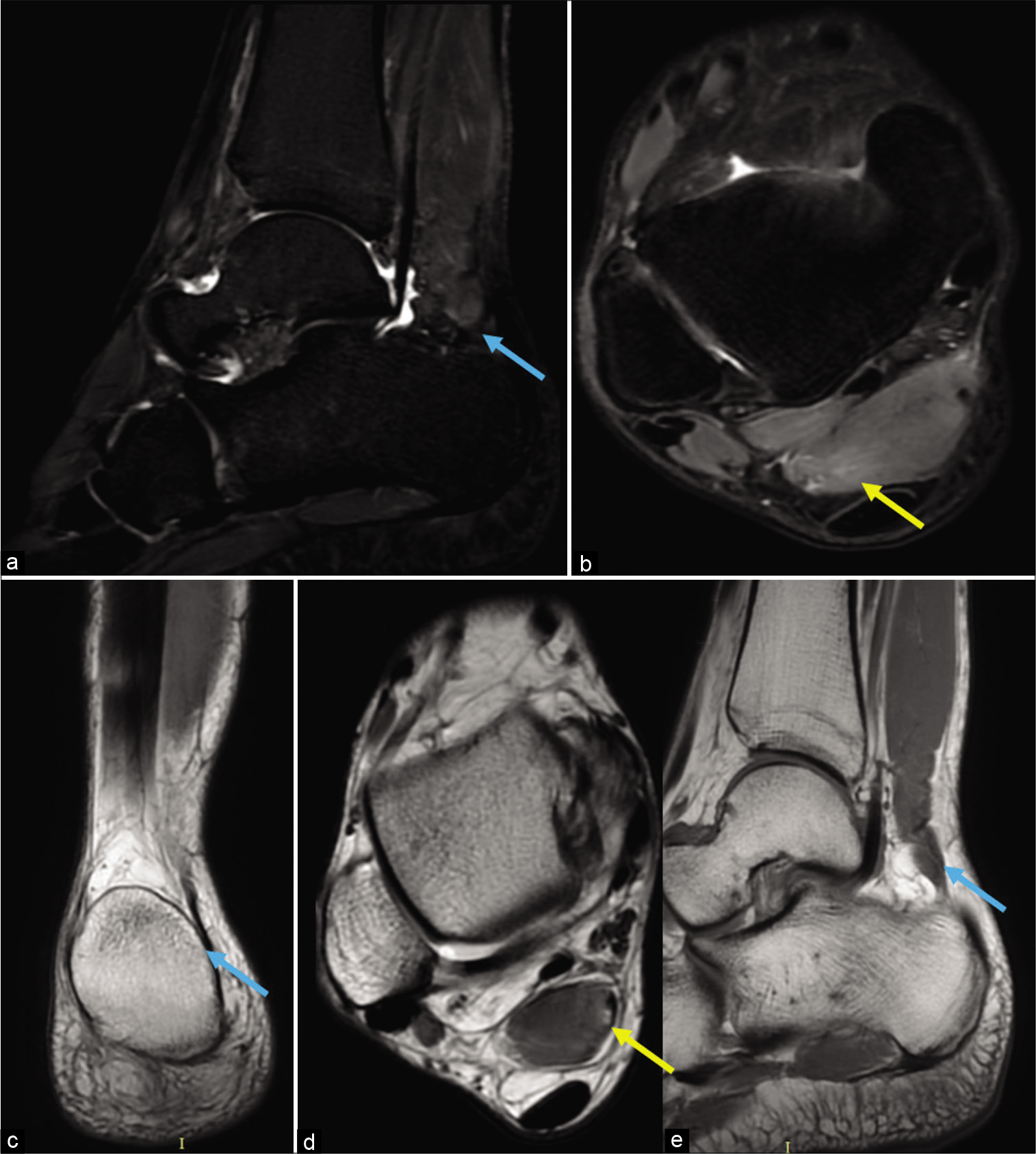
- Sagittal Short time to inversion recovery (STIR) (a), Axial proton density fat-suppressed (PDFS) images (b), Coronal PD (c), Axial PD (d) and Sagittal T1 weighted MRI images (e). An abnormal structure isointense to muscle anterior to Achilles tendon is seen inserting along the medial aspect of the calcaneum (a,c,e) (blue arrows). Axial PDFS and PD non fat suppressed images (b and d) reveal focal intrafascicular edema in the form of hyperintensity along the inferior aspect of the muscle with focal discontinuity along the myotendinous junction (yellow arrows). Posterior tibial nerve appears normal.
The patient was explained about the medical and surgical treatment options and started on analgesics and physical therapy. The patient is on medical follow-up presently.
DISCUSSION
Accessory soleus muscle is a rarely encountered entity. The prevalence of accessory soleus muscle imaging has been documented to be around 3%.[3] Early splitting of the soleal anlage embryologically results in formation of accessory soleus muscle. Proximally, it attaches to the native soleus muscle along the anterior surface of soleus, soleal line of tibia, or fibula.[4] Distally various anatomical types of insertion have been defined, namely – Type A: Insertion along the superior aspect of the calcaneal tuberosity directly (fleshy insertion) or through separate tendon, Type B when directly inserted on the Achilles tendon, Type C involves insertion along the medial aspect of the tuberosity through fleshy fibers or a separate tendon, and Type D involves insertion along the superomedial aspect through bifid tendon. In Type E, there is fusion with the insertion of plantaris muscle.[5]
It is encased within its own fascia and posterior tibial nerve and posterior tibial artery form its neurovascular supply. Accessory soleus may masquerade as soft-tissue tumor along the posterior leg with differential diagnosis that includes lipoma, hemangioma, hematoma, and sarcoma.[6]
It can present with pain along the lower leg and ankle with attributable pathophysiologies being tibial nerve compression, vascular insufficiency due to vascular compression, and exertional compartment syndrome.[7] Achilles tendon paratenonitis can also precipitate pain secondary to deranged biomechanics.[8]
Less than 10 cases with injuries (partial or complete) tear or sprain of accessory soleus have been documented in literature.[9-12] Treatment depends on the severity of the symptoms and functional disability. In cases of mild-to-moderate symptoms, conservative treatment in the form of rest, physical therapy, activity modification, analgesics, and orthoses like heel pads may be initiated.[13] In cases with severe discomfort leading to functional impairment, surgical techniques are effective in the form of fasciotomy and excision of accessory soleus muscle.[14]
CONCLUSION
Accessory soleus muscle is an important anatomical variation, and its varying pathologies can masquerade a variety of clinical scenarios. A thorough clinical understanding of the biomechanics and multiple pathologies of the accessory muscle is important for clinicians as well as radiologists are foremost. Muscle injuries and sprains of accessory soleus muscle compounds the pre-existing symptoms of exertional claudication. Imaging with ultrasound and MRI helps in delineating the specific findings and helps in creating a road map for management.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Accessory soleus muscle. A report of 4 cases and review of literature. Clin Orthop Relat Res. 1997;337:180-6.
- [CrossRef] [PubMed] [Google Scholar]
- Symptomatic accessory soleus muscle: Diagnosis and follow-up on magnetic resonance imaging. Br J Radiol. 2006;79:e129-32.
- [CrossRef] [PubMed] [Google Scholar]
- MRI diagnosis of accessory soleus muscle: A case report and review of the literatures. Int J Foot Ankle. 2019;3:3-6.
- [CrossRef] [Google Scholar]
- Tran Minh V. Aspect IRM des variantes anatomiques des muscles, tendons et ligaments de la cheville [MR imaging of anatomical variants of ligaments, muscles and tendons at the ankle] J Radiol. 2002;83:27-38.
- [Google Scholar]
- Dissecting the accessory soleus muscle: A literature review, cadaveric study, and imaging study. Clin Anat. 2011;24:903-10.
- [CrossRef] [PubMed] [Google Scholar]
- Anomalous muscles simulating soft-tissue tumors in the lower extremities, Report of three cases. J Bone Joint Surg Am. 1965;47:1397-400.
- [CrossRef] [Google Scholar]
- Accessory soleus muscle: A difficult diagnosis: A case report and a review of the literature. Eur J Orthop Surg Traumatol. 2012;22:205-9.
- [CrossRef] [PubMed] [Google Scholar]
- High association between accessory soleus muscle and Achilles tendonopathy. Skeletal Radiol. 2008;37:1129-33.
- [CrossRef] [PubMed] [Google Scholar]
- MR imaging of the accessory soleus muscle appearance in six patients and a review of the literature. Skeletal Radiol. 1994;23:525-8.
- [CrossRef] [Google Scholar]
- MRI diagnosis of accessory soleus muscle strain. Br J Sports Med. 1995;29:277-8.
- [CrossRef] [PubMed] [Google Scholar]
- Isolated rupture of the accessory soleus tendon: An original and confusing picture. Skeletal Radiol. 2018;47:1455-9.
- [CrossRef] [PubMed] [Google Scholar]
- Accessory muscles: Anatomy, symptoms, and radiologic evaluation. Radiographics. 2008;28:481-99.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrasound and magnetic resonance imaging diagnosis of isolated tear of the accessory soleus tendon: A case report and review of the literatures. J Orthop Case Rep. 2020;10:84-7.
- [Google Scholar]
- The accessory soleus muscle: A report of 21 cases and a review of the literature. Rev Chir Orthop Reparatrice Appar Mot. 2005;91:232-8.
- [CrossRef] [Google Scholar]






