Translate this page into:
Surgical oncology residents’ perspective in the COVID-19 pandemic: Standing at crossroads

*Corresponding author: Kaival K. Gundavda, Department of Surgical Oncology, Tata Memorial Hospital, Homi Bhabha National Institute, Mumbai, Maharashtra, India. gundavdakaival@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gundavda KK, Patkar S, Gulia A. Surgical oncology residents’ perspective in the COVID-19 pandemic: Standing at crossroads. Indian J Med Sci, 2021;73(1):66-9.
Abstract
The COVID-19 pandemic has hampered health-care delivery, with non-emergent consultations and surgical procedures being brought to a standstill. However, a delay in comprehensive cancer care may result in disease progression and poorer outcomes. Surgical oncology residents often form the front line responders for cancer patients, but now also have to function outside of their specialty to serve in COVID-19 units. With the uncertainty and unpredictability of this pandemic, surgical oncology residents find themselves at a crossroads. The need to keep abreast with COVID-19 treatment guidelines and recommendations comes at the expense of their surgical training. There is also a rising concern about personal safety, wellness, psychosocial well-being, and burnout. We highlight various elements concerning residents and suggest strategies that may be undertaken to allay anxiety and fatigue and facilitate surgical education.
Keywords
Surgical oncology
COVID-19
Pandemic
Residency training
Burnout
INTRODUCTION
Coronavirus disease 2019 (COVID-19) was first identified during an outbreak of pneumonia in the city of Wuhan, China, in December 2019. However, it was not until the virus had affected over 100,000 people across 100 countries that the WHO declared it as a pandemic.[1]
At the time of writing this article, over 7,365,000 individuals were affected by the virus across India, with 112,144 fatalities.[2] Maharashtra alone hosts over a fifth of the cases, Mumbai being severely affected. At the heart of the city lies our hospital, an apex cancer institute dedicated to serving cancer patients from across the country.
THE NEED TO CONTINUE CANCER CARE
Annually, India sees over one million new cancer cases, of which over 0.2 million require surgery.[3] Of these, nearly 785,000 individuals succumbed to their disease in 2018 alone.[4] Without timely surgical resection, the death rate due to progressive malignancy is likely to exceed the COVID-19 specific mortality rate. In view of resource constraints and the potential overburden on health care, various international guidelines were formulated for triage of non-emergent surgical procedures. The American College of Surgeons (ACS) recommends following the elective surgery acuity scale from St. Louis University. Most cancer surgeries are categorized as Tier 3a surgeries and should not be postponed.[5] We continued to perform elective cancer surgery besides dedicating a section of hospital resources to care for cancer patients diagnosed with the COVID-19 infection.
ONCOLOGY RESIDENTS: THE FIRST-LINE RESPONDERS
Surgical oncology residents comprise a large portion of the workforce in a tertiary cancer hospital. The work profile of oncology residents is now expanded to include care of COVID-19 patients in addition to routine cancer care, as depicted in Figure 1. After years of surgical training, rotations in COVID-19 isolation wards and fever OPDs compelled us to revisit our medicine roots.
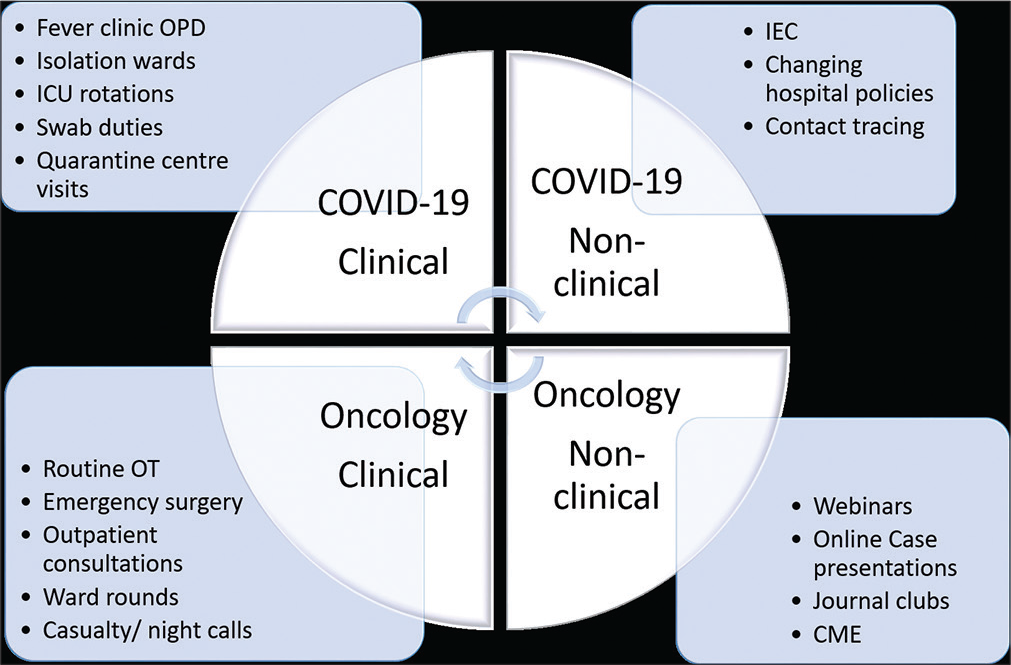
- Managing cancer and COVID-19 duties: The work spectrum of a surgical oncology resident.
Meticulous attention to hand hygiene, adequate use of protective equipment, and the need to physically distance have become the new norm. This caution is not only limited to the workplace but also in the staff cafeteria and hostel accommodations.
The management of cancer patients also posed novel and unanticipated challenges. Extensive implementation of lockdown measures across the nation affected patients, health-care personnel, and the supply of essential services alike. Patients scheduled for surgery often found themselves stranded; those who reported to the hospital were subjected to pre-operative COVID-19 testing. The uncertainty was confounded by innumerable factors such as availability of type-specific blood products, uninterrupted supply of surgical implants, and other essential materials. As a result, 0-h cancellation of surgeries led to a waste of precious theatre time. Finally, the smooth functioning of elective surgeries was realizable largely by the well-being and adequacy of the operation theater (OT) staff.
COVID-19 AND ITS IMPACT ON SURGICAL ONCOLOGY TRAINING
The decrease in case volume and a subsequent reduction in clinical exposure has put the surgical oncology resident training program in jeopardy. Grand rounds, multidisciplinary joint clinics, continuing medical education, and classroom lecture series, which were once the mainstay of learning for oncology residents, have come to a standstill. In an attempt to minimize exposure, time spent eliciting history and examining patients were inadvertently curtailed. Oncology residents felt the need to familiarize themselves with the adaptation of digital platforms such as teleconferencing, webinars, and virtual case presentations. These innovative solutions may enable us to reach out to a wider audience, and the use of technology may help bridge the educational gap in these unprecedented times.[6]
Judicious use of OT resources, curtailing of non-essential surgeries where possible, and a reduced patient volume is likely to hamper “hands-on” surgical training. Workdays lost on account of shift-duties, rotations in COVID-19 wards and the unfortunate need to quarantine only makes matters worse.
Teaching hospitals should view this as an opportunity to establish surgical simulators and dry labs for skill training as part of their routine training program. In addition, COVID-19 literature should be discussed as part of the journal club to better understand the challenges of this pandemic and its global impact on surgical practice. It is of paramount importance that institutes tailor their resident program to mitigate the impact of this novel disease on surgical education and look to optimize clinical exposure without a compromise in safety [Table 1].
| S. No | Resident concerns | Measures to mitigate |
|---|---|---|
| 1. | Exposure to COVID-19 and testing | Triage criteria for stratifying exposure[11] Designated testing sites for employees Guidelines for quarantine and testing in suspected or COVID-19 positive staff |
| 2. | Consequences of quarantine | Restrict length of quarantine[9] Provision of adequate supplies Improved communication Coping and stress management techniques |
| 3. | Personal well-being and family safety | Availability and institutional protocol for PPE use Emphasize training of surgical staff on PPE- donning and doffing procedures Physical distancing measures in OPD and wards Preserving human resources Providing facilities for self-isolation |
| 4. | Ward and OPD logistics | Implementing social distancing and physical barriers Minimize patient attendants and visiting hours Transition outpatient clinics to telemedicine Creation of rotating surgical teams for inpatient care Combination of inpatient surgical services with decreased resident complement Supervision by infection control teams |
| 5. | OT limitations | Pre-operative COVID-19 testing for all surgical patients Safe operating room practices – adequate protective gear, safety COVID-19 checklists Limiting operating room staff to essential members only Develop dedicated COVID-19 OT |
| 6. | Reduced academic and surgical experience | Flexible teleconferencing COVID-19 journal clubs Virtual multidisciplinary joint clinics, case presentations Use of surgical videos Virtual classroom models Simulation laboratories |
| 7. | Psychological safety | Access to licensed medical support teams – clinical psychologist/ staff physicians Mentorship programs Flexible working hours[10] Workshops on stress management and coping strategies[10] |
SURGEON PROTECTION AND USE OF PERSONAL PROTECTIVE EQUIPMENT (PPE)
Spending long hours in PPE are a challenge for every health-care professional, more so for surgeons. The use of PPE leads to altered temperature perception, excessive perspiration, dehydration, and headaches.[7] Fogging of protective eye gear from the FF3/N95 masks and shields impairs vision,[8] and the use of double gloves decreases haptic feedback while performing fine motor tasks. The use of multiple masks and face shields limits communication between the operating surgeon and assistants. Skin breakdown behind the ears and the bridge of the nose have become a common occurrence, accompanied by musculoskeletal aches leading to early fatigue.
RESIDENTS’ PERSONAL SAFETY AND WELLNESS
The negative psychosocial impacts of COVID-19 on residents across specialties have been reviewed extensively. A recently published survey of a global oncology workforce showed that an alarming 78% had felt increased concern for their personal safety since the onset of the pandemic.[9,10] Post-traumatic stress symptoms, confusion, and anger have been reported in quarantined residents.[11] Besides their personal safety, the thought of potentially infecting patients, colleagues, and family bear heavy on their mind. To minimize exposure, residents should be made to work in shifts, with a back-up team standing by to address unanticipated absences or exposures. Preserving human resources are of utmost importance to tackle this pandemic. PPE should be made readily available, and its use should be optimized as per guidelines.[12] A triage system for stratifying risk of exposure should be introduced and implemented [Table 1].[13] Contact tracing should be meticulous, and “at risk” residents should be identified and isolated early.
Six months into the pandemic, with no end in sight, attention must be paid to mental health and psychosocial well-being of residents. The phenomenon of burnout was reported in 49% of cancer professionals,[9,10] and well-being of residents must be prioritized. They should be provided anonymous access to a qualified team comprising clinical psychologists and staff physicians. Initiating mentorship programs, wellness, and burnout coping workshops may help alleviate resident anxiety in these challenging times.
LESSONS LEARNED AND LOOKING AHEAD
Surgical oncology residents can use this opportunity to hone their leadership and enhance managerial skills. Interested residents should volunteer to work alongside critical care- trained staff in dedicated COVID-19 ICUs and fever clinics. Clear and transparent communication at all levels is of paramount importance. Being first-line responders for cancer care, surgical oncology residents should be included in pertinent administrative discussions. This will enable administrators to understand challenges faced at the grassroots and will provide residents the opportunity to imbibe leadership qualities which may be useful in their future. Residents should also strive to be a portal to reinforce patients and relatives about safe practices in the times of COVID-19 and to caution against “pandemic fatigue.” A surgical oncology resident is caught at the crossroads between providing COVID-19 care to the best of his abilities at the expense of their surgical training. The long-term implications of this pandemic on surgical oncology training and preparedness and future well-being of residents remain to be seen.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
Kaival K. Gundavda and Ashish Gulia are on the editorial board.
References
- WHO Director-General's Opening Remarks at the Media Briefing on COVID-19. 2020. Available from: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19[Last accessed on 2020 Mar 11]
- [Google Scholar]
- Available from: https://www.worldometers.info/coronavirus/country/india [Last accessed on 2020 Oct 16]
- Outcomes of elective major cancer surgery during COVID 19 at Tata Memorial Centre: Implications for cancer care policy. Ann Surg. 2020;272:e249-52.
- [CrossRef] [PubMed] [Google Scholar]
- Available from: https://www.gco.iarc.fr/today/data/factsheets/populations/356-india-fact-sheets.pdf [Last accessed on 2020 Sep 28]
- ACS, COVID-19 Guidelines for Triage of Cancer Surgery Patients. 2020. Available from: https://www.facs.org/covid-19/clinical-guidance/elective-case/cancer-surgery [Last accessed on 2020 Sep 29]
- [Google Scholar]
- Using technology to maintain the education of residents during the COVID-19 pandemic. J Surg Educ. 2020;77:729-32.
- [CrossRef] [PubMed] [Google Scholar]
- Limiting factors for wearing personal protective equipment (PPE) in a health care environment evaluated in a randomised study. PLoS One. 2019;14:e0210775.
- [CrossRef] [PubMed] [Google Scholar]
- Compliance and perception about personal protective equipment among health care workers involved in the surgery of COVID-19 negative cancer patients during the pandemic. J Surg Oncol. ;2020
- [CrossRef] [PubMed] [Google Scholar]
- The impact of COVID-19 on oncology professionals: Initial results of the ESMO resilience task force survey collaboration. Ann Oncol. 2020;31(Suppl 4):S1142-215.
- [CrossRef] [Google Scholar]
- The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet. 2020;395:912-20.
- [CrossRef] [Google Scholar]
- ACS, COVID-19: Considerations for Optimum Surgeon Protection Before, During, and After Operation. 2020. Available from: https://www.facs.org/covid-19/clinical-guidance/surgeon-protection [Last accessed on 2020 Sep 29]
- [Google Scholar]
- Optimization of surgical resident safety and education during the COVID-19 pandemic-lessons learned. J Surg Educ. ;2020
- [CrossRef] [PubMed] [Google Scholar]






