Translate this page into:
Utilization of clinical autopsy services in a Nigerian teaching hospital

*Corresponding author: Samuel Robsam Ohayi, Department of Histopathology, Enugu State University Teaching Hospital and College of Medicine, Enugu, Nigeria. robohayi@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Ohayi SR, Edeh AJ, Onyishi NT. Utilization of clinical autopsy services in a Nigerian teaching hospital. Indian J Med Sci 2021;73(1):77-81.
Abstract
Objectives:
The aim of this study was to ascertain the rate of uptake of clinical autopsy services in our hospital and also determine the associated factors. Autopsy is an important part of clinical practice. It serves as an audit and quality control for diagnosis and treatment of diseases. It also provides families with “informed grieving” by giving clearer understanding of the nature of illness and cause of death and may reveal inheritable or communicable diseases among other benefits. Despite these benefits, the rate of autopsy is low and declining globally.
Material and Methods:
A retrospective study of hospital autopsies performed from January 2013 to December 2017 was carried out. The mortuary and autopsy records of our hospital over the period were retrieved and reviewed. Deaths reported to the police, namely, coroner deaths and deaths before arriving at the hospital (brought in dead, BID) were excluded from the study.
Results:
A total of 1976 bodies was studied, 1078 males and 898 females (M:F = 1:1.2). Consent for autopsy was sought in 22 (1.1%) cases: 13 (0.66%) from pediatrics, 5 (0.25%) from internal medicine, and the rest from surgery and obstetrics and gynecology. Consent was granted and autopsy performed in 6 (0.3%) cases giving an average of 1.2 autopsies/year. Average hospital stay was 12.6 days and 36.3 days for those consenting to and those declining autopsy, respectively. Consenting persons belong to diverse socioeconomic strata.
Conclusion:
Autopsy rate is very low in our center. Attending clinicians and relatives of the deceased contribute to this trend. Vigorous education for all stakeholders about the benefits of hospital autopsy is recommended.
Keywords
Cause of death
Autopsy
Consent
Attending physicians
Bereaved persons
Stress of bereavement
INTRODUCTION
From prehistoric times, man has always been preoccupied with searching for the cause of death. As medicine developed, physicians carried out postmortem examination on dead bodies for this purpose. Greek physicians eventually called that inquiry “autopsy” which literally means “see for self.” Autopsy is a systematic, scientific examination of a dead body to determine the cause of death; the pathologies and processes leading to death; the extent of disease; the effects of treatment on the body; and the presence of undiagnosed diseases that may have contributed to death.[1] The various types of autopsy include complete autopsy and partial or restricted autopsy. Needle-only autopsy (including body fluid aspiration), molecular autopsy in which disease markers are looked for in tissues and body fluids, and postmortem imaging using computerized tomography (CT) scan and magnetic resonance imaging (MRI) are relatively new but promising techniques.[2]
Autopsy serves as an audit and quality control for safety, diagnosis, and treatment. By giving clearer understanding of the nature and cause of illness and death, it can provide families with “informed grieving” and therefore closure. In addition, autopsy may reveal diseases in the family that may be inheritable or communicable. It helps in advancement of medical research and education and provides information on the causes of death in a society and therefore provides useful information for policymakers for effective planning. Despite these benefits, the rate of autopsy is not only low but still declining globally. In the United States for instance, autopsy rate has fallen from 50% of all hospital deaths in the 1940s and 50s and 25–35% of the mid-1960s to the present day 7–9%.[3,4] Reasons for falling autopsy rate include religious considerations (e.g., questions about reincarnation; rumors about removal of body parts), social (need for cosmesis, delay of burial, etc.), and economic (cost of autopsy, who pays for an autopsy). Other reasons include continuing technology-driven improvement in antemortem diagnostic techniques, clinicians fear that autopsy may reveal their errors and therefore lead to litigation, non-handing down of the autopsy tradition through medical school training, and a waning interest of pathologists themselves.[5] The objective of the study was to ascertain the rate of utilization of clinical autopsy in a university teaching hospital and determine the factors affecting the practice.
MATERIAL AND METHODS
This is a retrospective study of autopsy practice in Enugu State University Teaching Hospital in Nigeria. It involved the use of standardized forms to extract data of a 5-year period from January 1, 2013, to December 31, 2017, from the hospital’s mortuary and histopathology department archives and also from the records of the relevant hospital clinical units. The hospital has 272-bed capacity with a yearly average in-hospital admission of 7929 persons and yearly average mortality (of those on admission) of 423.3. It has an in-facility mortuary and an autopsy suite; two full-time and two parttime pathologists. It is located in the city of Enugu the state capital which according to 2016 estimates has a population of about 815,272. The population is predominantly Igbo and Christian with a good blend of the major denominations, namely, Catholic, Evangelical, and Pentecostal. The literacy level of the population is high and the main occupations are civil service, commerce, and craftsmanship.
Following death of a patient on admission in the hospital, the body is transferred to the hospital mortuary for storage except in the rare occasion in which a body is removed within few hours of death. Record of such stored bodies is kept in a dedicated register in the hospital mortuary. In addition, a record of autopsies performed in the mortuary is kept in a dedicated register stored in the histopathology department. Attending clinicians are expected to inform relations of a demised patient about the need for autopsy on the body of the deceased and subsequently seek consent for same. If obtained, the consent is passed onto the pathologist with a request for autopsy and the deceased’s case note. This is a process of interdepartmental consulting. On receiving such a request, the pathologists proceed to perform an autopsy after a meeting with the person or persons who gave consent if he/they are willing for such a meeting. After an autopsy procedure, the pathologist’s report when ready is issued to the attending clinician for onward transfer to the deceased’s relation(s) while a copy is archived in the histopathology department of the hospital.
Data were collected by the first author who was assisted by a house officer who had been trained for the purpose. Data collected included demographic characteristics of the deceased namely sex, age, marital status, religious affiliation, educational qualification, and last occupation before death. Other information collected includes place, month and time of death, length of stay in the hospital, and clinical diagnosis; whether consent for autopsy was sought and reason for refusing autopsy. The following information about the person from whom consent was sought and obtained (or not obtained) were also retrieved: sex, age, relationship with deceased, highest educational qualification, and occupation at the time of the death event.
Coroner deaths, that is, deaths reported to the police including sudden unnatural deaths, deaths from interpersonal violence, and other forms of trauma including various forms of accidents, deaths before arriving to the hospital (brought in dead) were excluded from the study. Data obtained were analyzed by simple statistical methods for means and proportions using Microsoft Excel. Ethical clearance was obtained from our hospital’s ethical clearance committee.
RESULTS
A total of 2125 bodies were received in the hospital mortuary in the period under review out of which 149 were excluded from the study for various reasons as outlined in the methodology section. Of the 1976 studied, there were 1078 males and 898 females (M:F = 1:1.2). Ninety-six (4.9%) were aged below 18 years while 1880 (95.1%) were aged 18 years and above. Although attending clinicians claim that they generally often suggest the need for autopsy to a deceased’s relations, actual request for autopsy was made in 22 (1.1%) of cases distributed as follows: 13 (0.66%) from pediatrics, 5 (0.25%) from internal medicine, surgery, 2 (0.1%), and obstetrics and gynecology, 2 (0.1%). Consent was granted and autopsy performed in 6 cases (27.3% of requested consent and 0.3% of total number of deaths) giving an average of 1.2 autopsies per year. Four (66.6%) of the autopsies were performed on pediatric subjects while 1 each (16.6%) was from internal medicine and obstetrics and gynecology. The average hospital stay for those who consented to autopsy is 12.6 days and 36.3 days for those that declined autopsy. Representatives of the deceased and/or deceased family from whom the consent for autopsy were requested (obtained or declined) belonged to diverse socioeconomic and educational strata, as shown in Table 1. Reasons for declining autopsy are grouped into religious, social, and economic and are displayed in Figure 1 and include concerns about disfiguring the body, delay in burial and cost of, and payment for autopsy among others.
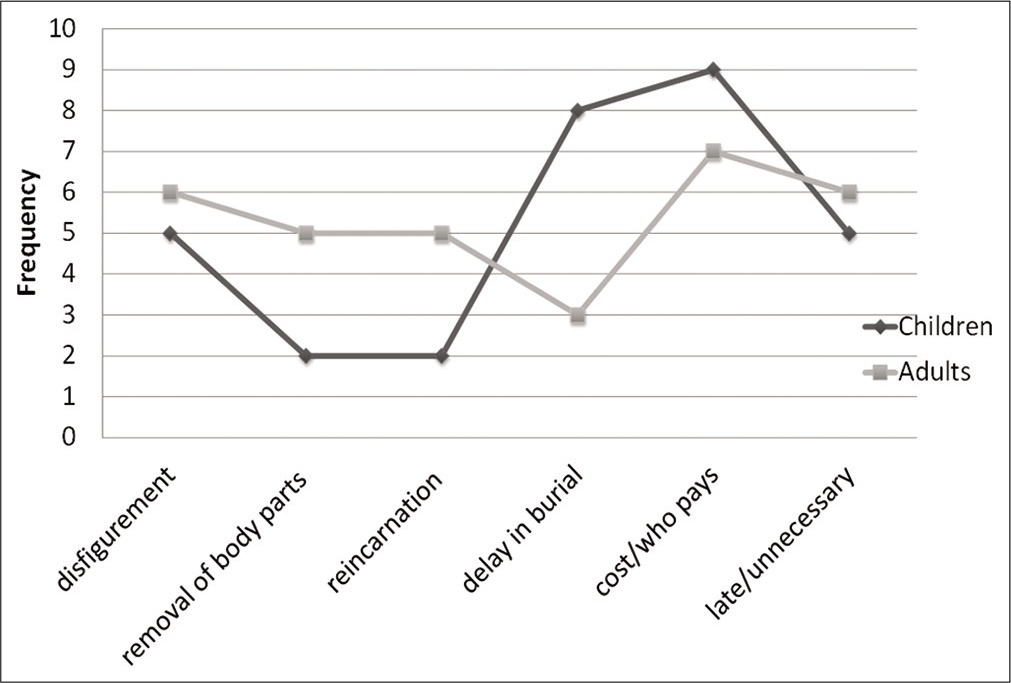
- Reasons of declining autopsy.
| Deceased | Deceased’s survivors/relations | |||||
|---|---|---|---|---|---|---|
| Cases | Age; sex of deceased | Relationship with deceased | Age of survivor (years) | Highest education | Occupation | Denomination |
| Cases in which autopsy was performed | ||||||
| 1. | 8 months; Male | Father | 34 | Primary | Bus driver | Catholic |
| 2. | 15 years; Male | Father | 43 | Secondary | Civil servant | Evangelical |
| 3. | 58 years; Female | Daughter | 33 | Secondary | Trader | Catholic |
| 4. | 23 days; Female | Father | 40 | Tertiary | Banker | Catholic |
| 5. | 63 years; Male | Son | 35 | Tertiary | Construction engineer | Evangelical |
| 6. | 11 years; Male | Father | 50 | Secondary | Upholster | Pentecostal |
| Cases in which consent for autopsy was declined | ||||||
| 1. | 29 years; Male | Father | 59 | Secondary | Retiree | Catholic |
| 2. | 12 years; Female | Uncle | 48 | Tertiary | Civil servant | Pentecostal |
| 3. | 68 years; Female | Son | 42 | Secondary | Trader | Catholic |
| 4. | 55 years; Female | Husband | 63 | Tertiary | Civil servant | Catholic |
| 5. | 13 years; Male | Father | 37 | Secondary | Trader | Evangelical |
| 6. | 11 years; Male | Father | 44 | Tertiary | Journalist | Pentecostal |
| 7. | 10 months; Female | Father | 27 | Primary | Artisan | Catholic |
| 8. | 58 years; Male | Brother | 51 | Secondary | Artisan | Catholic |
| 9. | 15 years; Male | Father | 43 | Secondary | Company worker | Evangelical |
| 10. | 27 years; Female | Brother | 38 | Tertiary | Business man | Catholic |
| 11. | 63 years; Male | Son | 37 | Secondary | Self-employed | Pentecostal |
| 12. | 11 years; Male | Father | 29 | Secondary | Tricycle driver | Evangelical |
| 13. | 8 months; Male | Aunt | 34 | Tertiary | Civil servant | Catholic |
| 14. | 15years; Male | Father | 40 | Primary | Artisan | Pentecostal |
| 15. | 53 years; Female | Son | 26 | Secondary | Self-employed | Catholic |
| 16. | 26 days; Male | Husband | 29 | Primary | Trader | Evangelical |
DISCUSSION
Performance of autopsy on a body is in some respects unlike any other medical procedure or service rendered in medical practice. Except in a case where someone left consent for autopsy on his or her body in a will before demise, the service is one for which consent is sought from someone else. Second, the person who seeks consent for this procedure is usually different from the person who will carry out the procedure since the former is the one in contact with the subject of the autopsy and his or her relation(s) while the subject was alive. These peculiarities about autopsy can ultimately affect the willingness of the bereaved to give consent as the attending clinician may not be very keen on persuading the person(s) concerned about autopsy. Furthermore, the bereaved person may not trust the pathologist who he or she may only be seeing or hearing about for the first time after the death event. There is also the issue of the skills of persons who approach the bereaved family for consent for an autopsy. In our study, junior doctors, namely, residents and sometimes, house officers are saddled with the task of obtaining consent from bereaved persons. The limited skill and experience of this category of doctors in this regard plus their youthfulness usually make them inadequate for such profound duties. Some researchers have advocated that experienced doctors, possibly the attending physician, should be the ones to take up this role while in addition, some centers train some staff, especially for the purpose.[5,6]
In this study, clinicians sought for consent for autopsy in only 1.1% of deaths. This apparent lack of interest in autopsy is similar to that of physicians elsewhere as reported by other workers.[5,7,8] Clinicians in our center blamed their lack of interest in requesting autopsy following a death event in part on the paucity of pathologists in our center a condition similar that was reported by other workers.[5,9] There is also the concern that autopsy may reveal clinician’s errors that may lead to litigation. This concern from clinicians is also reported by other workers.[5,8,10] Contrary to this fear, however, autopsy has been reported to bring about more favorable legal outcomes for clinicians than otherwise when litigation arose about a clinician’s care of a patient.[10] Clinicians also prefer to take sides with relations of a bereaved person when they decline autopsy. The reason for this may be to just not aggravate the stress of bereavement. Consent was eventually obtained and autopsy performed in only 6 (0.3%) cases. This rate is similar to findings in other parts of Nigeria[11,12] and much lower than figures reported by workers in developed countries.[3,4] Similar to other studies,[5,13] the pediatrics unit constituted the highest source of both requests for and performed autopsies. Gordijn et al.[14] on literature review reported an average rate of 38% of perinatal autopsy in Europe.
The reasons for refusing autopsy in our study are similar to those reported elsewhere and include fear that the body may be mutilated which extrapolates to concerns about cosmesis, namely, disfiguring the dead body, fear of angering the ancestors who forbid cutting the dead, concerns about reincarnation, and concerns about the cost of and payment for the autopsy.[5,9,11,12] Refusal of pediatric autopsy was mostly hinged on desire to avoid time loss as parents usually wanted to remove a dead child for immediate burial. Lishimpi et al.[15] reported similar reason from Zambia. Another reason that resonated with most people refusing autopsy in our study was the concern about removing body parts for ritual purposes. Our study also revealed that length of hospital stay before death had an inverse relationship with giving consent. At present, our hospital does not charge a fee for clinical autopsies a situation which is in contrast to what obtains elsewhere.[5] A curious aspect of our population’s lack of enthusiasm for autopsy was that even when clients are not required to pay for the service and pathologists were available to perform an autopsy, an overwhelming majority of people still refused to give consent.
Even with improved diagnostic techniques, studies still show significant disparity between antemortem and postmortem diagnosis.[16,17] Our study found similar outcome with postmortem diagnosis in 2 cases (33.3%) being different from clinical diagnosis. This seems to further underscore the importance of the clinical autopsy as an important clinical procedure. To make autopsy more acceptable to people, several innovative modifications of procedure are being tried.[8] One example is the verbal autopsy. Some pediatricians in our center appear keen on employing this method. Its value is, however, limited by associated recall bias and by culture’s potential to interfere with people’s attitude to and interpretation of symptoms.[9] It is also limited by its dependence on the type of health care available to the respondents and on local doctors’ knowledge of the characteristics of the diseases in an area.[18] Another innovation is the group of procedures described as minimal invasive autopsy which includes needle-only autopsy, body fluid aspiration, molecular autopsy and postmortem imaging using CT scan, MRI and 3D optical scanning, and postmortem angiography.[5,9] These procedures are, however, very expensive where available and cannot interpret color and certain other morphological changes, infection condition, and artifacts. Some people have advocated including in hospital admission protocols a clause that bodies of people that dies in the hospital shall be subjected to autopsy as a matter of protocol. Arguments against this include its potential to violate patient’s autonomy and also to worsen stress of bereavement. In addition, it can also worsen the pathologist’s workload problem, especially against the backdrop of the limited number of pathologists.
A limitation of this work is in the nature of bereavement, especially as it is in our culture. A proper assessment of people’s attitude to autopsy may be difficult to achieve by sampling people who are presently dealing with the loss of a relation.
CONCLUSION
Clinical autopsy is very poorly utilized in our center. Clinicians and relatives of deceased persons contribute to this state of continuing decline of autopsy. Long hospital stay appears to discourage relations from accepting autopsy. There is a need for education of the general public on the benefits of autopsy. Furthermore, there should be concerted efforts to create avenues for engagements between clinicians and pathologists as a way of addressing the issues that create disinterest and, sometimes, outright fear of autopsy in the clinicians. Efforts should be made to increase the exposure of medical students to autopsy while observation and performance of autopsy should be mandatory for pathology trainees during training and examinations.
Acknowledgment
The authors are grateful to the staff of the mortuary of the hospital where this work was done.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- VIRTOPSY: Minimally invasive, imaging-guided virtual autopsy. Radiographics. 2006;26:1305-33.
- [CrossRef] [PubMed] [Google Scholar]
- The impact of declining clinical autopsy: Need for revised healthcare policy. Am J Med Sci. 2009;337:41-6.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of simple interventions on necropsy when active informed consent is required. Lancet. 1999;354:1391-2.
- [CrossRef] [Google Scholar]
- Searching for cause of death through different autopsy methods: A new initiative. J Fam Med Prim Care. 2017;6:191-95.
- [CrossRef] [PubMed] [Google Scholar]
- The conventional autopsy in modern medicine. J R Soc Med. 2008;101:177-81.
- [CrossRef] [PubMed] [Google Scholar]
- Requesting perinatal autopsy: Multicultural considerations. Am J Mater Child Nurs. 2007;32:81-6.
- [CrossRef] [PubMed] [Google Scholar]
- The role of the autopsy in medical malpractice cases, I. A review of 99 appeals court decision. Arch Pathol Lab Med. 2002;126:1023-31.
- [Google Scholar]
- Paucity of clinical autopsies: A great concern. Highl Med Res J. 2009;8:83-7.
- [CrossRef] [Google Scholar]
- Trends in clinical autopsy rates in a Nigerian tertiary hospital. Afr J Med Sci. 2007;36:267-72.
- [Google Scholar]
- How the pediatric autopsy yields valuable information in a vertically integrated health care system. Arch Pathol Lab Med. 2004;128:1239-46.
- [Google Scholar]
- Value of the perinatal autopsy: Critique. Paed Dev Pathol. 2002;5:80-8.
- [CrossRef] [PubMed] [Google Scholar]
- Necropsies in African children: Consent dilemmas for parents and guardians. Arch Dis Child. 2001;84:463-7.
- [CrossRef] [PubMed] [Google Scholar]
- Analysis of the sensitivity of death certificates in 440 hospital deaths: A comparison with necropsy findings. J Clin Pathol. 2002;55:499-502.
- [CrossRef] [PubMed] [Google Scholar]
- Death certificates are not reliable: Revivification of the autopsy. South Med J. 2006;99:728-33.
- [CrossRef] [PubMed] [Google Scholar]
- Validation of verbal autopsy methods for assessment of child mortality in SubSaharan Africa and the policy implication: A rapid review. Pan Afr Med J. 2019;33:318.
- [CrossRef] [PubMed] [Google Scholar]






