Translate this page into:
Acute appendicitis as the first manifestation of HenochSchönlein purpura
*Corresponding author: Pedro Nogarotto Cembraneli, Department of Medical Sciences Course, Health Sciences School, Faculdade Ceres (FACERES), Avenida Anísio Haddad, nº 6751, São José do Rio Preto, SP, Brazil. pedrocembranelli@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Cembraneli PN, Cavalcante JBF, Cavalcante RBF, Cavalcante JES. Acute appendicitis as the first manifestation of HenochSchönlein purpura. Indian J Med Sci 2021;73(1):114-6.
Abstract
Henoch-Schönlein purpura (HSP) is a small vessel systemic vasculitis. Typical symptoms include palpable purpura, joint pain, and abdominal pain. Most cases improve after a few weeks, not requiring any treatments other than symptom control. Acute abdomen resulting from vasculitis is very rare and should be treated as a surgical emergency. We report the case of a 9-year-old boy with acute gangrenous appendicitis as the first manifestation of HSP.
Keywords
Acute abdomen
Appendicitis
Henoch-Schönlein purpura
INTRODUCTION
Henoch-Schönlein purpura (HSP) is a systemic idiopathic vasculitis related to deposits of immune complexes, mainly containing immunoglobulins A (IgA) on the walls of small vessels. The disease is characterized by the association of cutaneous, joint, and gastrointestinal signs.[1] Skin involvement is almost constant and is the first sign of HSP in more than two-thirds of the cases. The course of this illness is usually self-limited, with a good prognosis in most cases.[2] Digestive manifestations can be moderate, spasmodic pain, but they can be severe, leading to a surgical outcome.[3] We report the case of a 9-year-old male patient with acute gangrenous appendicitis as the first manifestation of HSP.
CASE REPORT
A 9-year-old male patient was taken to the emergency room due to a complaint of abdominal pain for a week. It had started as a feeling of discomfort in the abdominal region associated with nausea, anorexia, and unverified fever. The mother reported that the child had just had the flu and she suspected that the abdominal pain could be part of the infectious disease. However, the boy began to feel a lot of pain in the region of the right iliac fossa, and his parents sought for medical help. Physical examination revealed that he was pale, dehydrated, and afebrile, with pain from diffuse palpation of the abdomen and showed defensive reflexes of the abdominal muscles. The boy underwent a laparotomy that evidenced acute gangrenous appendicitis complicated by purulent peritonitis [Figure 1].
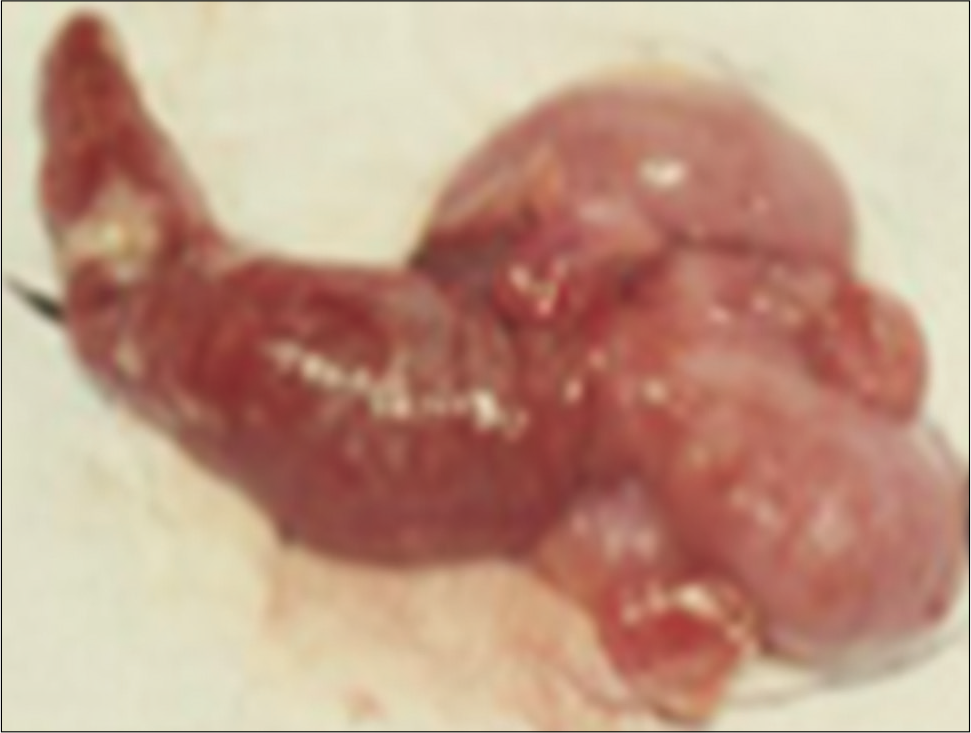
- Surgical specimen showing an appendix with inflammation, hyperemia, and signs of necrosis.
On the 2nd post-operative day, he remained dehydrated and presented with tachycardia, tissue perfusion of 4 s, diffuse abdominal pain, decreased breath sounds (hydrothorax), arthralgia in the wrists, and presence of palpable purpura in the lower limbs and gluteal region [Figure 2].
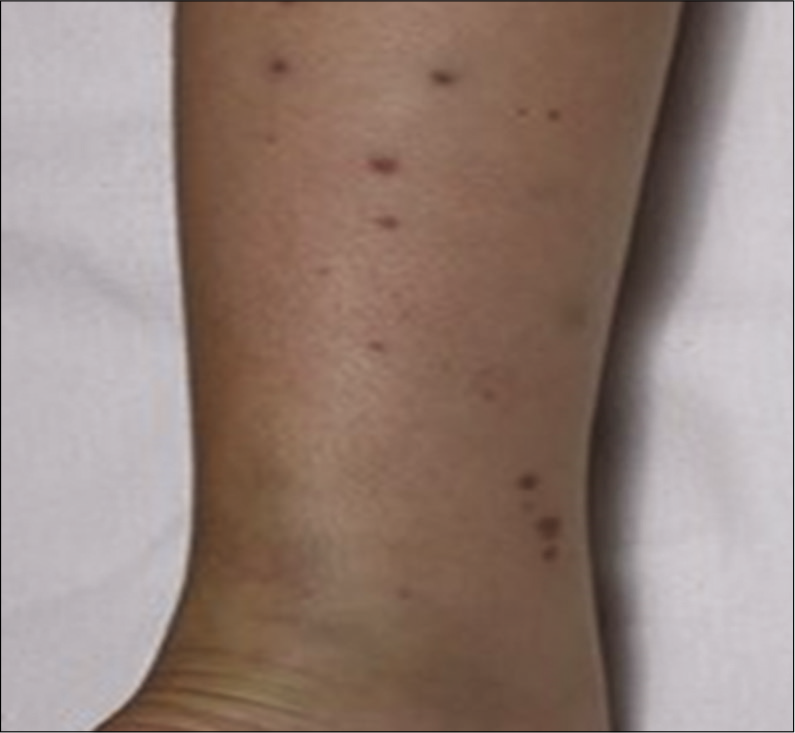
- Palpable purpura in the lower limb.
Laboratory tests showed leukocytosis with the left shift associated with a platelet count of 690,000, and the imaging tests revealed no changes. The anatomical pathology examination confirmed the diagnosis of acute gangrenous appendicitis [Figure 3].
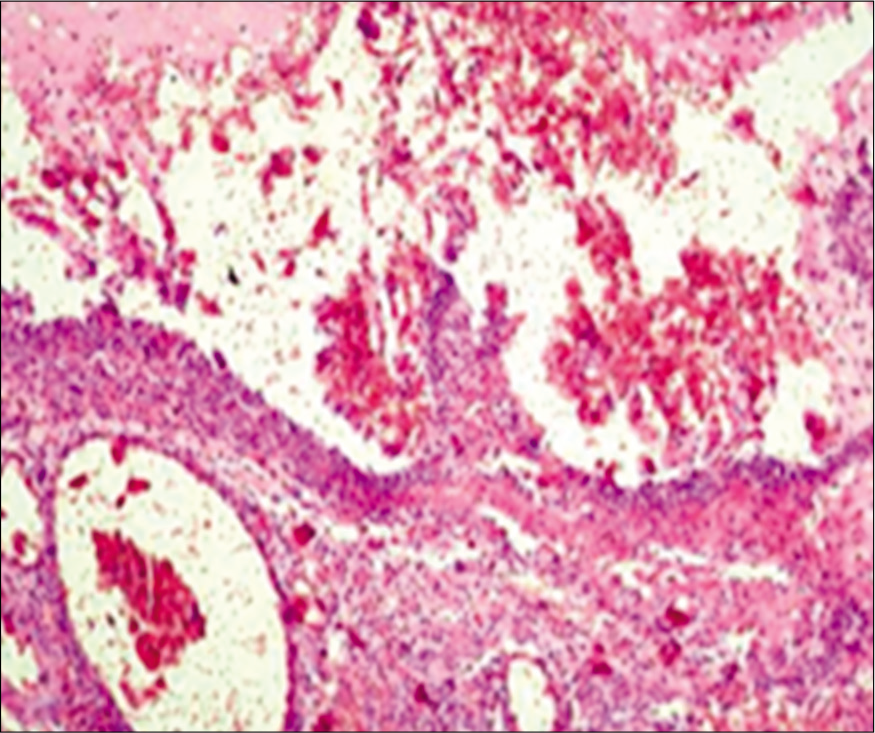
- Acute appendicitis with fibrinopurulent exudate in all layers of the appendix.
We decided to treat the patient postoperatively with a combination of ceftriaxone and metronidazole, associated with methylprednisolone, resulting in significant improvement of the condition. The patient showed good evolution, was discharged uneventfully 2 weeks after the surgery, and was followed up at the outpatient clinic.
DISCUSSION
Most cases of HSP are preceded by an upper respiratory tract infection, suggesting a potential infectious trigger.[4] The most characteristic pathological feature is a deposition of immune complexes containing IgA on the vessel walls of the affected organs and the renal mesangium.[5]
The main manifestations are palpable purpura, generally painless and non-pruritic, located predominantly in the lower limbs and gluteal region. Enteric vasculitis, leading to ischemia, edema, and hemorrhage, can occur in two-thirds of HSP cases, and the major symptom is abdominal pain of varying intensity. The acute abdomen condition may occur concurrently or preceding the skin rash and be associated with vomiting, transient paralytic ileus, ischemia, and necrosis. Intestinal perforation, massive intestinal bleeding, pancreatitis, pseudomembranous colitis, appendicitis, and fistula formation are more rare.[3]
The diagnosis of HSP is based on clinical criteria, i.e., palpable purpura (mandatory criterion) and at least one minor criterion: (1) Diffuse abdominal pain; (2) arthritis or arthralgia; (3) renal involvement; and (4) biopsy showing leukocytoclastic vasculitis with a predominant deposit of IgA or proliferative glomerulonephritis with a predominant deposit of IgA. The sensitivity of clinical criteria is 100%, and the specificity is 87% when applied to children.[6] Applied to adults, the diagnostic sensitivity is 99.2%, and the specificity is 86%, supporting this use in all patients with HSP.[7]
The treatment is controversial and depends on kidney involvement. In patients with the absence of renal involvement, the treatment is purely symptomatic. Pain medications, rehydration therapy, and surgery should be employed in specific cases.[8]
CONCLUSION
Gastrointestinal manifestations of HSP may precede other clinical manifestations of HSP by days, and although acute appendicitis is a very rare complication, health professionals should be aware of this possibility.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- The adult kidney 24 years after childhood Henoch-Schönlein Purpura: A retrospective cohort study. Lancet. 2002;360:666-70.
- [CrossRef] [Google Scholar]
- Henoch-Schönlein Purpura in adults: Outcome and prognostic factors. J Am Soc Nephrol. 2002;13:1271-8.
- [CrossRef] [PubMed] [Google Scholar]
- Henoch Schonlein Purpura in childhood: Epidemiological and clinical analysis of 150 cases over a 5-year period and review of literature. Semin Arthritis Rheum. 2005;35:143-53.
- [CrossRef] [PubMed] [Google Scholar]
- Temporal association of Streptococcus, Staphylococcus, and parainfluenza pediatric hospitalizations and hospitalized cases of Henoch-Schönlein Purpura. J Rheumatol. 2010;37:2587-94.
- [CrossRef] [PubMed] [Google Scholar]
- Aberrant glycosylation of IgA1 is inherited in both pediatric IgA nephropathy and Henoch-Schönlein Purpura nephritis. Kidney Int. 2011;80:79-87.
- [CrossRef] [PubMed] [Google Scholar]
- EULAR/PRINTO/PRES criteria for HenochSchönlein Purpura, childhood polyarteritis nodosa, childhood Wegener granulomatosis and childhood takayasu arteritis: Ankara 2008. Part I: Overall methodology and clinical characterisation. Ann Rheum Dis. 2010;69:798-806.
- [CrossRef] [PubMed] [Google Scholar]
- IgA vasculitis in adults: The performance of the EULAR/ PRINTO/PRES classification criteria in adults. Arthritis Res Ther. 2016;18:58.
- [CrossRef] [PubMed] [Google Scholar]
- Randomised, double-blind, placebo-controlled trial to determine whether steroids reduce the incidence and severity of nephropathy in Henoch-Schönlein Purpura (HSP) Arch Dis Child. 2013;98:756-63.
- [CrossRef] [PubMed] [Google Scholar]






