Translate this page into:
Demographic profile, spectrum, awareness, and cost of renal replacement therapy of chronic kidney disease patients in a public tertiary care center in Rajasthan, India
*Corresponding author: Rajesh Jhorawat, Department of Nephrology, All India Institute of Medical Sciences (AIIMS), Jodhpur, Rajasthan, India. jhorawat2000@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Jhorawat R, Meena RK, Kularaj SS, Sharma SK, Beniwal P, Gupta R, et al. Demographic profile, spectrum, awareness, and cost of renal replacement therapy of chronic kidney disease patients in a public tertiary care center in Rajasthan, India. Indian J Med Sci. 2024;76:99-104. doi: 10.25259/IJMS_240_2023
Abstract
Objectives:
Chronic kidney disease (CKD) is widely recognized as the leading cause of death worldwide. Diabetes and hypertension are common risk factors. This is the only study on CKD from Rajasthan that highlights basic CKD profiles in patients attending public tertiary care centers.
Materials and Methods:
This observation study included diagnosed cases of CKD attending nephrology outpatient department (OPD) from January to December 2020. Data regarding the cause of CKD, its stage, mode of renal replacement therapy (RRT), and direct cost of medication were collected. The state runs various schemes, including free dialysis facilities for all, below-poverty level cards (below poverty line [BPL] cards, which had complete free treatment), and state health cards Bhamasha Swasthya Bima Yojana (BSSY) under the government scheme.
Results:
A total of 252 patients were included in the study. Patients on dialysis were highest, followed by stage V and stage IV CKD, representing 33.73%, 18.65%, and 17.86%, respectively. Hypertension was the predominant cause of CKD, representing 29.37% and CKD (u) prevalence in our study was 14.68%. The direct cost of treatment at CKD stages I, II, III, IV, and V were Rs. 520 ($6.93), Rs. 2435.71 ($32.48), Rs. 3400 ($45.33), Rs. 3405.57 ($45.41), and Rs. 4815.97 ($64.21) per month, respectively. The monthly medicine cost of treatment on hemodialysis was Rs. 6730.60 ($89.74), Rs. 30,278 ($403.71) on peritoneal dialysis, and Rs. 5021.74 ($66.96) on renal transplant. BPL card holders were 8.33%, 39.68% had BSSY card, 16.27% had Insurance, and around one-third (35.71%) were without support.
Conclusion:
Age, socioeconomic status, and geographical location affect CKD etiology. The accessible dialysis facility, insurance, and government policies affect the selection of the RRT.
Keywords
Demographic profile
Spectrum
Awareness
Cost
Renal replacement therapy
Chronic kidney disease
INTRODUCTION
Chronic kidney disease (CKD) is extremely common and has emerged as one of the leading non-communicable causes of death worldwide. It is projected to affect an increasing number of individuals over time and to further rise in importance among the various global causes of death.[1] CKD contributes toward cardiovascular disease and increases mortality with a disproportionately large fraction of available healthcare resources burden.[2,3] In India, several factors contribute to the high prevalence of CKD, such as consanguinity, increased congenital anomalies, deficiency or hypovitaminosis A, or malnutrition with poverty exposed to known and unknown nephrotoxin during pregnancy leading to small kidney volume at birth. Added to these exposures is the growing burden of hypertension and diabetes mellitus. By 2030, India is expected to have the world’s largest population of patients with diabetes.[4-8]
Baseline characteristics of CKD patients in developing countries are lacking, especially in India which is a very heterogeneous country from social, cultural, economic, genetic, and climate and geography perspectives. More detailed, in-depth analysis will better understand factors such as age, ethnicity, level of development, and poverty in different regions on CKD causes and burden. This study was conducted to know how underlying demography, cost, and choice of renal replacement therapy (RRT) options for CKD prevalent in patients attending public tertiary care center in Rajasthan, India.
MATERIALS AND METHODS
It was an observational study that included a total of 252 CKD patients. These included patients who were on conservative treatment, on dialysis, and those who received renal transplantation. Patients who were attending the nephrology outpatient department from January 2020 to December 2020 were included in the study. During this period, CKD based on the kidney disease improving global outcome (KDIGO) was included in the study.[9] All the patients were evaluated based on history taking, clinical examination, and laboratory investigations. Staging of CKD was done based on the KDIGO staging system. Glomerular filtration rate was estimated using CKD-EPI (creatinine) formula.[9]
Inclusion criteria
The following criteria were included in the study:
Age ≥18 year
CKD patients on conservative treatment
Patient on dialysis (both hemodialysis [HD] and peritoneal dialysis [PD])
Renal transplant patients >6 months.
Exclusion criteria
The following criteria were excluded from the study:
Age <18 year
Patient on immunosuppression except for renal transplantation
Patient with another systemic disease with renal involvement (e.g., cirrhosis and congestive heart failure)
Patient with undiagnosed renal disease (awaiting kidney biopsy)
Patient with acute kidney injury.
The demographic profile of the patients was measured using pro forma.[10] Total of 252 patients were included, attending the nephrology outpatient department (OPD). The sample size was calculated using the prevalence of CKD of unknown origin (16%).[11,12] The study center was a public tertiary care center. Here, various health schemes such as “Mukhyamantri free dialysis scheme,” “Bhamasha Swasthya Bima Yojana (BSSY),” or “Ayushman Bharat Mahatma Gandhi Rajasthan Swasthya Bima Yojana” were being run by the state government. Under these schemes, patients had free access to HD facilities at government centers, and medicines were available free or at a subsidized rate.[10] PD was not free under the government scheme. In cost of treatment, additional money spent on purchasing medicine was included. Transport costs were not included in the study. Diabetic kidney disease was defined as a patient on anti-diabetic drugs or hemoglobin A1C >6.5%. Hypertension as a cause of CKD was defined as a patient who had a history of hypertension of ≥5 years, and there is no prior history of body swelling or hematuria. Chronic tubulointerstitial nephritis (CTIN) was defined as preserving urine output, no edema, no diabetes, no hypertension or hypertension control with one drug, and evidence suggestive of kidney damage, for example, nephrolithiasis, obstructive uropathy, systemic disease, and on chronic drugs. The CKD of unknown origin (CKDu) was defined as a patient with clinical findings suggestive of CTIN, no diabetes, hypertension, urine protein ≤2, and no apparent cause of kidney damage. Chronic glomerulonephritis (CGN) as a cause of CKD was defined as a history of edematous illness or oliguria or hypertension <5 years of duration or histopathological evidence of glomerular pathology. Our study was cleared from the Institute Ethical Committee (280/MC/EC/2021).
The Statistical Package for the Social Sciences (SPSS) 28 software (SPSS, Chicago, IL) was used for statistical analysis. The data were measured in both categorical and numerical values. The categorical parameter was estimated in frequencies or percentages, and numerical values were estimated as mean values ± standard deviation or proportions. The categorical data were compared using appropriate contingency tables and the Chi-square test. The continuous data were compared using the t-test or Mann–Whitney U-test. P < 0.05 was accepted as significant.
RESULTS
Demographic profile, CKD-cause, stage, and awareness of RRT
A total of 252 patients were included in the study. The mean age of the patients was 47.20 ± 15.53 years, and 70.23% were male. The body mass index (BMI) of the study population was 21.70 ± 4.67 kg/m2. Jaipur was the predominant draining district, followed by Alwar. Around 30% of the population neither read nor write, 17% studied up to the eighth standard, 14.68% were graduates or had an equivalent degree, and 7.14% were studied above it. Agriculturists and laborers comprise around one-third of the patients, followed by self-employed people or those running their businesses; most females were housewives (64%).
The predominant cause was hypertension, followed by CGN and diabetes, consisting of 29.37%, 21.43%, and 15.87%, respectively. Nephrolithiasis and its complications were the predominant cause of CTIN. Around 14.68% were CKD of unknown origin, and 7.14% were genetic/adult polycystic kidney disease (ADPKD) patients. Diabetes was more common in the elderly, and CGN was more frequent in the young [Figure 1]. Diabetes was more frequent in patients with high income than CKD (u), seen in the low-income group. The majority of our patients were in the advanced stage of CKD. More than 50% were in stage V, 33.73% were on dialysis, 7.14% were on PD. CKD Stages I, II, and III were unaware of the RRT or its option. In Stage IV, only 4.4% were aware, and in Stage V, 17% of the patients were aware of the RRT and its option.
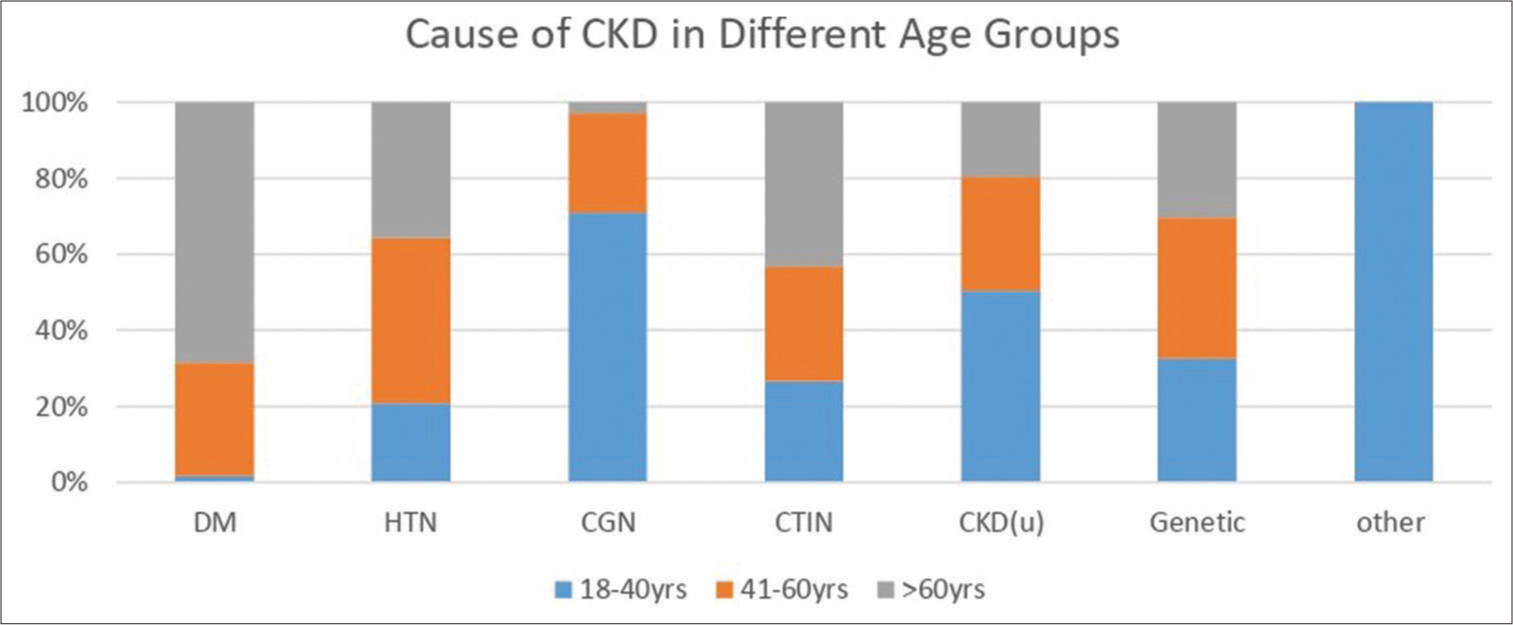
- Bar diagram showing cause of CKD in different age groups. Age groups between 18 and 40 years were the predominant population in our study (40.08%). DM is the most common cause of CKD in >60 years and CGN is most frequent in young ages (18–40 years). CKD: Chronic kidney disease, HTN: Hypertension, DM: Diabetes mellitus, CGN: Chronic glomerulonephritis, CTIN: Chronic tubule-interstitial nephritis, CKD (u): CKD of unknown etiology.
CKD-differences in urban and rural population
Table 1 highlighted the urban and rural populations with CKD in our study. Around 41% of the rural population was uneducated. The rest half studied up to 8th or 12th standard and hardly 10% of rural patients graduated or had a PG degree, whereas one-third of urban CKD patients had a degree of graduation or above. The rural population’s financial status was poor compared to the urban population, and drinking water sources differed between the two groups. However, the chronic familial disease was more in urban CKD patients than in rural, and the financial support of the two populations was also different. Rural patients had the financial support of below poverty line (BPL) cards or BSSY cards. In contrast, the urban population was proportionally more self-dependent/owned business (no support) or had Insurance [Table 1].
| Urban (%) | Rural (%) | P-value | |
|---|---|---|---|
| Total patients | 129 | 123 | 0.705 |
| Male/female | 90/39 | 87/36 | 0.441 |
| Age | 50.25±15.73 | 44.01±14.71 | 0.189 |
| BMI (kg/m2) | 22.87±5.24 | 20.47±3.62 | 0.12 |
| Education | |||
| None | 24 (18.60) | 53 (41.08) | <0.05 |
| Up to 8th | 20 (15.50) | 23 (18.70) | |
| 9–12th | 44 (34.11) | 30 (24.39) | |
| Some college | 0 (0) | 3 (02.44) | |
| Graduate/degree | 24 (19.38) | 12 (09.76) | |
| PG/master/professional | 16 (12.40) | 2 (1.6) | |
| Occupation | |||
| Agriculturist | 3 (2.32) | 40 (32.52) | <0.05 |
| Laborer | 15 (11.62) | 30 (24.39) | |
| Self-employed | 32 (24.80) | 10 (8.13) | |
| Salaried employee | 13 (10.07) | 9 (7.3) | |
| Housewife | 29 (29.48) | 19 (15.45) | |
| Student | 4 (3.10) | 6 (4.87) | |
| Unemployed | 10 (7.75) | 8 (6.5) | |
| Retired | 22 (17.05) | 1 (0.81) | |
| Other | 1 (0.78) | 0 (0) | |
| Family income | |||
| Rs. <2000/month | 8 (6.2) | 31 (25.20) | <0.05 |
| Rs. 2–5000/month | 20 (15.50) | 29 (23.57) | |
| Rs. 5–10,000/month | 33 (25.58) | 34 (27.64) | |
| Rs. >10,000/month | 68 (52.71) | 29 (23.58) | |
| Drinking water | |||
| Well | 16 (12.40) | 59 (47.96) | <0.05 |
| Tap water | 57 (44.18) | 33 (26.83) | |
| RO | 56 (43.41) | 27 (21.95) | |
| Pond/lake | 0 (0) | 1 (0.81) | |
| Other | 0 (0) | 3 (2.44) | |
| Family H/o chronic disease | |||
| Yes | 84 (65.12) | 48 (39.02) | <0.05 |
| No | 45 (34.88) | 75 (60.98) | |
| Cause of CKD | |||
| Diabetes | 28 (21.70) | 12 (9.75) | 0.89 |
| Hypertension | 45 (34.88) | 29 (23.57) | |
| CGN | 24 (18.60) | 30 (24.39) | |
| CTIN | 10 (07.75) | 14 (11.38) | |
| CKD (u) | 12 (09.30) | 24 (19.51) | |
| Genetic/ADPKD | 9 (06.98) | 9 (07.31) | |
| Other | 1 (0.77) | 5 (04.06) | |
| Financial support | |||
| BPL card | 6 (4.65) | 15 (12.19) | <0.05 |
| BSSY card | 30 (23.65) | 70 (56.91) | |
| Self | 62 (48.06) | 28 (22.76) | |
| Insurance (central/state/Pvt.) | 31 (24.03) | 10 (08.13) |
CKD: Chronic kidney disease, HTN: Hypertension, DM: Diabetes mellitus, CGN: Chronic glomerulonephritis, CTIN: Chronic tubulointerstitial Nephritis, CKD (u): CKD of unknown etiology, ADPKD: Adult polycystic kidney disease, RRT: Renal replacement therapy, BSSY: Bhamasha Swasthya Bima Yojana, BPL: Below poverty line, H/o: History of, RO: Reverse osmosis, Pvt.: Private, PG: Postgraduate, BMI: Body mass index, (1$: Rs. 75.00)
Characteristics of end-stage renal disease (ESRD) and RRT selection
In our study group, the mean age of stage V CKD patients was 51.21±15.00 years. However, younger patients underwent renal transplantation and HD, whereas patient on PD were more aged. The factors that affected RRT selection in our study were age and financial support. In our study, those with BBSY cards and no support selected HD in our center, and those with Insurance went for PD. The cost of PD was highest among RRT options. Factors such as education, occupation, family income, and CKD cause do not affect the selection of RRT [Table 2]. Of those who chose HD, only 5.97% were initiated through AV fistula, and the rest, 94.03%, initiated HD through a temporary dialysis catheter.
| Stage V (%) | HD (%) | PD (%) | RTx (%) | P-value | |
|---|---|---|---|---|---|
| Total patients | 47 | 67 | 18 | 23 | |
| Age | 51.21±15.00 | 41.61±13.12 | 61.5±11.51 | 36.03±10.67 | <0.05 |
| BMI | 22.93±5.37 | 20.3±3.95 | 22.39±3.84 | 21.03±2.94 | 0.89 |
| Female | 21 (44.68) | 16 (23.88) | 5 (27.78) | 2 (8.70) | 0.29 |
| Occupation | |||||
| Agriculturist | 10 (21.28) | 14 (20.89) | 0 | 7 (30.43) | 0.39 |
| Laborer | 6 (12.76) | 15 (22.39) | 0 | 2 (8.69) | |
| Self-employed | 11 (23.40) | 14 (20.89) | 1 (5.55) | 6 (26.08) | |
| Salaried employee | 1 (2.13) | 5 (7.46) | 5 (27.78) | 3 (13.04) | |
| Housewife | 12 (25.53) | 10 (14.93) | 4 (22.22) | 1 (4.35) | |
| Student | 1 (2.13) | 2 (2.98) | 1 (5.55) | 2 (8.69) | |
| Unemployed | 2 (4.26) | 6 (8.96) | 0 | 2 (8.69) | |
| Retired | 4 (8.52) | 1 (1.49) | 7 (38.89) | 0 | |
| Family income | |||||
| <Rs. 2000/months | 8 (17.02) | 9 (13.43) | 0 | 8 (34.78) | 0.46 |
| Rs. 2–5000/months | 7 (14.89) | 14 (20.89) | 0 | 2 (8.69) | |
| Rs. 5–10,000/months | 19 (40.42) | 21 (31.34) | 0 | 7 (30.43) | |
| >Rs. 10,000/months | 13 (27.66) | 23 (34.33) | 18 (100) | 6 (26.08) | |
| Cause of CKD | |||||
| Hypertension | 14 (30) | 13 (19.4) | 5 (27.8) | 6 (26) | 0.13 |
| DM | 9 (19) | 8 (11.9) | 12 (66.7) | 1 (4.3) | |
| CGN | 5 (10.6) | 25 (37.3) | 1 (5.5) | 12 (52.2) | |
| CTIN | 14 (30) | 18 (26.9) | 0 | 4 (17.4) | |
| ADPKD/genetic | 4 (8.5) | 3 (4.5) | 0 | 0 | |
| Other | 1 (2.0) | ||||
| First dialysis started | - | - | |||
| AV fistula | 4 (5.97) | ||||
| Catheter (Tempo) | 63 (94.03) | ||||
| Avg. cost of treatment | Rs. 4815.96/month | Rs. 6730.60/month | Rs. 30,278/month | Rs. 5021.74/month | <0.05 |
| Financial support | |||||
| Insurance | 7 (14.9) | 2 (3) | 14 (77.8) | 0 | <0.05 |
| BSSY | 19 (40.4) | 33 (49.3) | 0 | 8 (34.8) | |
| BPL | 2 (4.3) | 4 (6) | 1 (5.6) | 8 (34.8) | |
| No support (self) | 19 (40.3) | 28 (41.8) | 3 (16.6) | 7 (31.4) |
CKD: Chronic kidney disease, HTN: Hypertension, DM: Diabetes mellitus, CGN: Chronic glomerulonephritis, CTIN: Chronic tubulointerstitial nephritis, ADPKD: Adult polycystic kidney disease, HD: Hemodialysis, PD: Peritoneal dialysis, TX: Transplantation (renal), RRT: Renal replacement therapy, RTx: Renal transplant, AV: Arteriovenous, BSSY: Bhamasha Swasthya Bima Yojana, BPL: Below poverty line, BMI: Body mass index, (1$: Rs. 75.00)
Cost of treatment and financial support
The monthly cost of direct treatment is highlighted in Table 2. At Stage I, the direct cost of treatment was Rs. 520/month, which increased to Rs. 4814.96/month at Stage V. For the patients opting for HD, around Rs. 6730.60/month was the additional direct cost, and those on continuous ambulatory peritoneal dialysis (CAPD), it was around Rs. 30,000/month. For renal transplant recipients, direct medication costs them around Rs. 5021/month. BSSY was the predominant financial support for patients in our study population, followed by Insurance (that includes state government or central government or Private) for around 16.27% of patients. One-third of patients had no financial support and 8.33% were BPL cardholders.
DISCUSSION
Rajasthan is the largest state in the Indian Union; however, the representation of CKD data is lacking. Two studies, Seek-India and Indian CKD (ICKD), published basic demographic details of CKD, its prevalence, and pattern in India except in Rajasthan.[8,13] This is the only study from the state highlighting basic CKD details. Our study population was younger and more undernourished compared to the ICKD study population (47.20 ± 15.53 years. vs. 50.3 ± 11.8 years) and 21.70 ± 4.67 kg/m2 vs. 24.4kg/m2.[8] Our state, which has a rural-dominated population (75.1%), had equal representation of the rural and urban populations in our study. This might be a referral bias as data collection was from the urban public tertiary care center, and most patients were in advanced CKD.[14] Moreover, around half of the CKD patients in our study were from the capital city and countryside, likely due to our center’s free dialysis facilities. Among the CKD population, 47.62% had attended less than high school compared to the SEEK-India study; only 37.6% had less than high school. Younger population, more under-nutrition, poor education status, and more advanced CKD in our study population compared to the ICKD study population.
One interesting and surprising finding was the cause of CKD in our study population. In the ICKD study, which included a pan-India CKD population, diabetes was the most common cause of CKD, followed by CTIN and CKD of unknown origin. However, in our study, hypertension was the most common cause of CKD, followed by CGN and diabetes. One fundamental difference in our study was that it is a single-center study and contains a younger, advanced CKD population from a more compromised socioeconomic status. In our study, the highest age distribution was between 18 and 40 years, and it is well highlighted that as age increases, diabetes, a cause of CKD, increases [Figure 1]. Even the prevalence of diabetes has a strong correlation with per capita income and BMI and our population had low BMI compared to ICKD population. Moreover, our study population was younger and belonged to the lower socioeconomic status, and all these factors are associated with a decreased prevalence of diabetes.[8,15] On the flip side, younger population in our study explains the high prevalence of CGN as a cause of CKD [Figure 1]. Hence, rather than unifying the causes of CKD, different age groups, socioeconomic status, and geographic distribution are likely to have an impact on CKD causation.
The cost of treatment increases as the stage of CKD increases. In our study, CKD Stage II direct monthly cost was Rs. 2435.71 (Rs. 29,228.52 annually), which increased to Rs. 4815.96 (Rs. 57,791.52 annually) at stage V. Similar trend was seen in a study by Ahlawat et al.[16] However, there is a sharp jump in the cost of treatment in CAPD compared to HD. This is due to free HD to all ESRD patients in the state. Interestingly, this difference is lost when we compare the cost of CAPD and HD with those of Insurance. Similar results were seen in another Indian study by Jeloka et al., where the cost of treatment between CAPD and HD in self-paying patients was not different.[17] Due to free access to HD, most of the patients in Stage V and on HD were of BSSY or who had no financial support [Table 2]. A similar trend was also reflected in renal transplants. However, CAPD was only opted by those who had insurance.
In addition, our study showed a significant difference in rural and urban CKD populations. The rural CKD patients had poor education and were predominantly agriculturists and laborers. CKD (u) is more seen in rural populations than in urban. They were more financially weak and had low family income. The financial support was in the form of BPL or BSSY cards. On the other hand, urban CKD patients were better educated, self-employed, and had higher family incomes. Diabetes and hypertension were more frequent in the urban population. Urban patients were financially more self-dependent and had more insurance cover compared to rural patients. Financial support, either in the form of a BSSY card, free dialysis, or Insurance, impacts decision to select the mode of RRT in our study [Table 2].
Our study is the first such attempt to highlight the basic information on CKD in the state. However, there are many limitations that need to be highlighted. First, this was a single-center-based study which might not reflect an accurate picture of CKD at the community level. Second, our study population reflects more advanced CKD, which is reflected in a high proportion of Stage V and HD patients due to the availability of free dialysis at our center. Third, as most patients were from weaker sections of society, this spectrum might not be reflected in patients attending corporate hospitals or center-based screening of CKD. Fourth, though this study hints toward variation in causes of CKD depending on social, economic, nutritional, and geographical location, generalization of information from this study on community-based CKD or non-public sector health care will not be justifiable. Fifth, the cost of medicines and RRT under various government schemes cannot be generalized to all patients. In addition to population differences, variability in practice patterns and access to healthcare services may be responsible for other additional differences.
CONCLUSION
Our study highlighted that different factors such as age, socioeconomic status, and geographic distribution have an impact on the causes of CKD. Age and financial support, either in the form of insurance or government policies, have an important impact on RRT selection.
Ethical approval
The research/study approved by the Institutional Review Board at SMS Medical College and Hospital, Jaipur, number 280/MC/EC/2021, dated 4/3/2021.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- The ascending rank of chronic kidney disease in the global burden of disease study. Nephrol Dial Transplant. 2017;32:ii121-8.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351:1296-305.
- [CrossRef] [PubMed] [Google Scholar]
- Differences in the care of ESRD patients worldwide: Required resources and future outlook. Kidney Int Suppl. 1995;50:S7-13.
- [Google Scholar]
- A challenge to chronic kidney disease in Asia: The report of the second Asian forum of chronic kidney disease initiative. Nephrology (Carlton). 2010;15:248-52.
- [CrossRef] [PubMed] [Google Scholar]
- Population-based estimation of renal function in healthy young Indian adults based on body mass index and sex correlating renal volume, serum creatinine, and cystatin C. Int J Nephrol Renovasc Dis. 2016;9:243-7.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic kidney disease in India: A clarion call for change. Clin J Am Soc Nephrol. 2018;13:802-4.
- [CrossRef] [PubMed] [Google Scholar]
- Global, regional, and national burden of chronic kidney disease, 1990-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2020;395:709-33.
- [CrossRef] [PubMed] [Google Scholar]
- The Indian Chronic Kidney Disease (ICKD) study: baseline characteristics. Clin Kidney J. 2022;15:60-9.
- [CrossRef] [PubMed] [Google Scholar]
- On translation of LD, IL and SFC given according to IEC-61131 for hardware synthesis of reconfigurable logic controller. IFAC Proc Vol. 2014;19:4477-83.
- [CrossRef] [Google Scholar]
- AB-MGRSBY : Ayushman bharat mahatma gandhi rajasthan swasthya bima yojana 2022. p. :1-13.
- [Google Scholar]
- What do we know about chronic kidney disease in India: First report of the Indian CKD registry. BMC Nephrol. 2012;13:10.
- [CrossRef] [PubMed] [Google Scholar]
- Sample size calculation in medical studies. Gastroenterol Hepatol Bed Bench. 2013;6:14-7.
- [Google Scholar]
- Epidemiology and risk factors of chronic kidney disease in India-results from the SEEK (Screening and Early Evaluation of Kidney Disease) study. BMC Nephrol. 2013;14:114.
- [CrossRef] [PubMed] [Google Scholar]
- Rajasthan at Glance. 2021. Available from: https://urban.rajasthan.gov.in/content/raj/udh/ctp/en/urban-profile/rajasthan-at-glance.html# [Last accessed on 2023 Dec 21]
- [Google Scholar]
- Diabetic kidney disease in the elderly: Prevalence and clinical correlates. BMC Geriatr. 2018;18:38.
- [CrossRef] [PubMed] [Google Scholar]
- Direct cost for treating chronic kidney disease at an outpatient setting of a tertiary hospital: Evidence from a cross-sectional study. Value Health Reg Issues. 2017;12:36-40.
- [CrossRef] [PubMed] [Google Scholar]
- Monthly cost of three exchanges a day peritoneal dialysis is same as of thrice a week hemodialysis in self-paying Indian patients. Indian J Nephrol. 2012;22:39-41.
- [CrossRef] [PubMed] [Google Scholar]






